Skin
Atif Ahmed
▪ Questions and Answers
1. The histologic picture of spongiosis can be found in all of the following situations EXCEPT:
a. Contact dermatitis due to poison ivy
b. Skin eruption from thiazide diuretics
c. Erythema nodosum
d. Pemphigus vulgaris
e. HIV patients with seborrheic dermatitis
View Answer
1. c. Spongiosis is an intracellular edema between keratinocytes in the epidermis. The edema may progress to spongiotic intraepidermal vesicles. Spongiosis is the hallmark of eczema but can be seen in other specific types of dermatitis. Erythema nodosum is characterized by a panniculitis-like picture with minimal epidermal involvement.
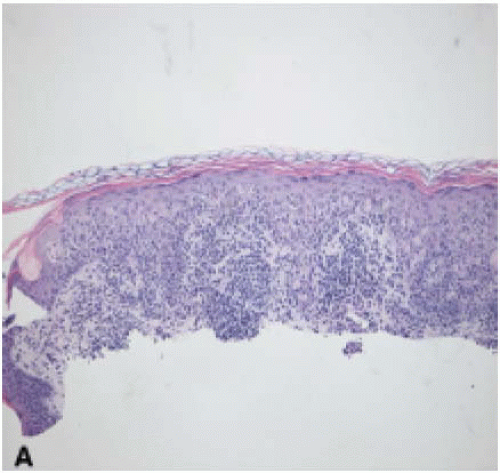
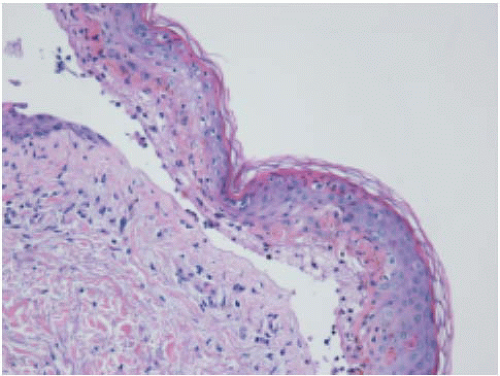
2. A biopsy of a solitary nonitchy papule on the skin reveals the following picture (Fig. 3.1). The cellular bodies indicated by the arrows are formed from:
a. Disintegrated collagen
c. Colloidal iron
d. Infiltrating IgM-positive histiocytes
e. Apoptotic koilocytes
View Answer
2. b. Colloid bodies are PAS-positive eosinophilic bodies found in the papillary dermis and lower epidermis in patients with lichen planus, drug eruptions, or lichenoid infiltrate. They consist of filaments and organelle remnants of apoptotic basal cells and appear as PAS-positive cytoplasmic inclusions. In lichen planus, they stain for IgM by direct immunofluorescence but they are not related to histiocytes.
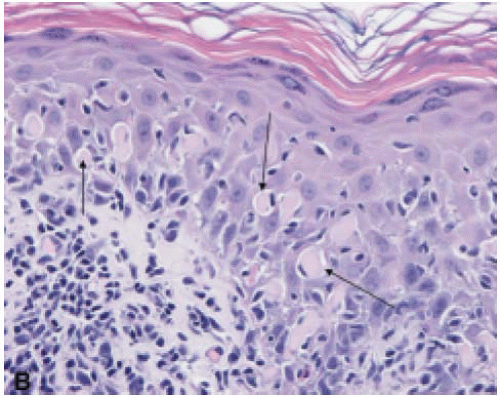
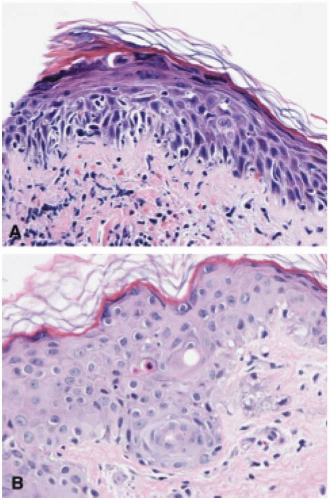
3. A 19-year-old HIV-positive man with a history of pneumocystis pneumonia developed erythematous, edematous macules symmetrically involving the skin of the arms, trunk, and legs, including the palms and soles. The diagnosis from this skin biopsy (Fig. 3.2) is:
a. Psoriasis
b. Seborrheic keratosis
c. Arthropod bite reaction
d. Erythema multiforme
e. Urticaria
View Answer
3. d. The image shows interface dermatitis, which can occur in erythema multiforme, toxic epidermal necrolysis, dermatomyositis, SLE, and cytoxic drug eruption. Erythema multiforme and toxic epidermal necrolysis display marked keratinocyte necrosis. Blisters may develop in both disorders. The most frequent etiology of erythema multiforme is infection. However, drugs, particularly sulfonamides, can result in more severe form, termed Stevens-Johnson syndrome.
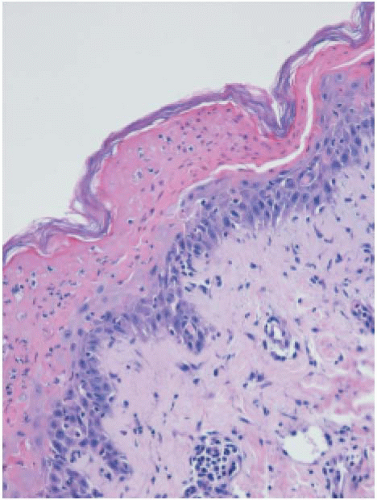
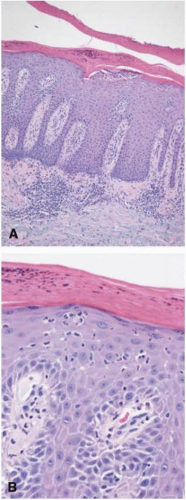
4. A 19-year-old African American woman with proteinuria and arthritis involving the knee and ankle developed a skin rash on the cheeks. Her serum was positive for anti-dsDNA antibodies. The patient’s skin biopsy is shown (Fig. 3.3). The diagnosis can be confirmed with any of the following tests EXCEPT:
a. Acid-fast stain
b. PAS stain
c. Colloidal iron stain
d. IgG and C3 immunofluorescence in biopsy from clinically normal skin
e. IgG and C3 immunofluorescence in biopsy from clinically involved skin
View Answer
4. a. Systemic lupus erythematosus is characterized by hyperkeratosis, follicular plugging, colloidal ironpositive dermal mucin, dermal lymphocytic infiltrate, and granular deposits of IgG and C3 along the epidermal basement membrane in lesional skin as well as normal skin. PAS stain will demonstrate thickened basement membrane.
5. Characteristic features of lymphomatoid papulosis include all of the following EXCEPT:
a. Clinical course following an arthropod bite
b. Perivascular lymphocytic inflammatory infiltrate
c. CD-30 positive lymphocytes in the epidermis
d. Clonal T-cell receptor gene rearrangement
e. Benign disease with spontaneous regression
View Answer
5. a. Lymphomatoid papulosis is a lymphoma-like lesion that is characterized by infiltrate of atypical CD30-positive, CD4-positive T-lymphocytes that may involve the epidermis. This lesion is benign but may progress to lymphoma or mycosis fungoides. An arthropod bite reaction does not give rise to lymphomatoid papulosis although the two entities may look similar in histology.
6. Lymphocytic cell infiltrate in the reticular dermis can be reliably diagnosed as mycosis fungoides if the cells are:
a. CD45+, CD30+, CD15+
b. CD3+, CD4+, CD8+
c. CD3+, CD4+, CD8+
d. CD20+, CD45+, CD10+
e. CD3+, CD8+, CD56+
View Answer
6. b. Mycosis fungoides may be considered a form of T-cell lymphoma of the T-helper phenotype. Cells express CD3 and CD4 and are negative for CD30 and CD7. The disease has a long course and appear as patches or plaques on the trunk that progress to infiltrative plaques. On histology, small cells with cerebriform or irregular nuclei infiltrate the dermis and epidermis.
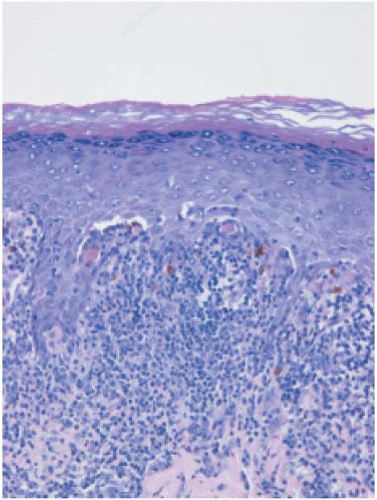
7. The diagnosis (Fig. 3.4) is most likely:
a. Staphylococcal scalded skin (SSS) syndrome
b. Toxic epidermal necrolysis (TEN)
c. Pemphigus vulgaris
d. Systemic lupus erythematosus
e. Pityriasis lichenoides et varioliformis acuta
View Answer
7. b. The image shows epidermal necrosis and bulla, which can occur in both SSS syndrome and TEN. In TEN, subepidermal bullae are formed. In SSS syndrome, the plane of cleavage is at or above the granular area. Toxic epidermal necrolysis causes extensive sloughing of skin and may be life threatening. It is usually due to sulfonamides, phenytoin, and other drugs.
8. Which of the following is NOT associated with human papillomavirus (HPV) viral infection?
a. Epidermodysplasia verruciformis
b. Condyloma acuminatum
c. Actinic keratosis
d. Bowen disease
e. Warty dyskeratoma
View Answer
8. e. Despite histologic similarities to viral warts, warty dyskeratoma is not a manifestation of human papilloma virus infection. All of the other lesions are related to HPV infection. More commonly, verruca vulgaris occurs on the acral skin of the hands and feet as manifestation of HPV type 2 infection.
9. A 17-year-old girl developed macular erythematous skin eruptions in the face, neck, and upper chest. Two weeks earlier, she received bone marrow transplantation after finishing a course of ablation chemotherapy. Two skin biopsies of different sites are represented in the picture (Fig. 3.5). The diagnosis is:
a. Pityriasis lichenoides et varioliformis acuta
b. Viral infection
c. Drug-associated linear IgA dermatosis
d. Radiation dermatitis
e. Acute graft-versus-host disease
View Answer
9. e. Acute graft-versus-host disease in the skin is characterized by spongiosis of the epidermis, vacuolization, and necrosis in the basal layer of the skin and subepidermal mononuclear cell infiltrate. Necrotic keratinocytes can also be seen in fixed drug eruption, pityriasis lichenoides, connective tissue disease, radiation dermatitis, and some viral infections. Thus, an appropriate clinical history in combination with histologic findings is needed for a proper diagnosis.
10. Tuberculosis of the skin may manifest as any of the following lesions EXCEPT:
a. Lupus vulgaris
b. Papulonecrotic skin lesions
c. Erythema induratum
d. Erythema nodosum
e. Hidradenitis suppurativa
View Answer
10. e. Tuberculosis of the skin is rare and can manifest in several forms. Lupus vulgaris presents as small red nodules in the face. Papulonecrotic tuberculid skin lesions show dermal necrosis, vasculitis, and edema. Erythema nodosum is subcutaneous panniculitis on the anterior surfaces of the legs. Erythema induratum occurs on the calves as subcutaneous nodules. Scrofuloderma results from extension to the skin of a tuberculous infection present in a lymph node or bone. All of these lesions may show granulomas with acid-fast bacilli. Hidradenitis is an adnexal inflammatory disease, not related to tuberculosis.
11. A 45-year-old white HIV-positive woman developed a generalized skin rash characterized by erythematous scaly papules and plaques with sharp borders. The diagnosis from this skin biopsy (Fig. 3.6) is:
a. Stevens-Johnson syndrome
b. Pemphigoid
d. Psoriasis
e. Acanthosis nigricans
View Answer
11. d. Psoriasis is a common inflammatory disorder that is characterized by scaly pink to red papules and plaques. It commonly involves the scalp, sacral region, and extensor surfaces of the extremities. It can extend to involve the entire skin. Histologically it is characterized by hyperkeratosis, parakeratosis, acanthosis, elongation of the rete ridges, and epidermal microabscesses (Monroe abscesses).
12. Which one of the following statements about lichen planus is true?
a. It characteristically involves the palms and soles.
b. Lesions show keratin-positive colloid bodies.
c. It is characterized by the presence of atypical cells.
d. It is differentiated from pemphigoid by absence of bullae.
e. It shows a scleroderma-like fibrosis of the dermis.
View Answer
12. b. Lichen planus involves the extensor surfaces and is characterized by hyperkeratosis, acanthosis, band-like dermal infiltrate, and colloid bodies. Bullae may occasionally be seen. No dyskeratotic or atypical cells are seen in lichen planus.
13. Which of the following is true about granuloma faciale?
a. It characteristically involves the face of young children.
b. It is a form of vasculitis.
c. Histology shows radial granulomas with necrotic centers.
d. It is characteristically associated with mycobacterial infection.
e. Histology resembles that of nodular panniculitis.
View Answer
13. b. Granuloma faciale is an idiopathic nonnecrotizing vasculitis forming dermal granulomas with eosinophils. The infiltrate is separated from the epidermis by a narrow band of uninvolved dermis. Typically it affects the face of adults as brown-red plaques. Streptococcal infections and radial granulomas are associated with erythema nodosum.
14. Erythema nodosum:
a. Presents with ulcerated skin lesions
b. Can progress to involve the muscles and bones
c. Is a vascular neoplasm
d. Is characterized histologically by nodular lymphoid infiltrate in the epidermis
e. Results from streptococcal skin infection
View Answer
14. e. Erythema nodosum is a nonulcerative self-healing lesion that involves the anterior surface of the legs. The histologic changes are present mainly in the subcutaneous tissue with mild inflammatory infiltrate affecting the dermis and the dermal-epidermal junction. Although streptococcal infection is the most common cause, other bacterial, fungal, and protozoal infections can also be associated with erythema nodosum. It can also occur with some cases of leukemia, lymphoma, and other malignancies.
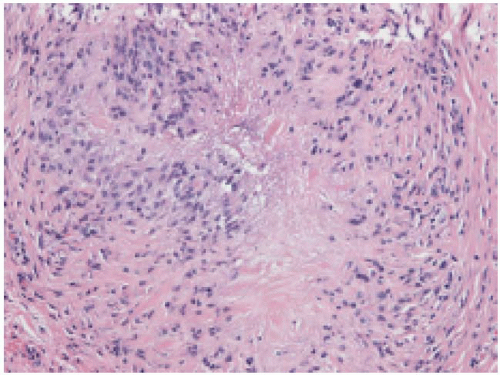
15. A 37-year-old woman has a firm nonpruritic papule located on her hand. The lesion was excised (Fig. 3.7). GMS and an acid-fast bacilli stain are negative. What is the most likely diagnosis?
a. Granuloma annulare
b. Sarcoidosis
c. Rheumatic nodule
d. Atypical mycobacterial infection
e. Epithelioid sarcoma
View Answer
15. a. Granuloma annulare occurs on the dorsum of the hands and feet and shows well-demarcated area of disintegrated collagen surrounded by fibroblasts and histiocytes that stain with vimentin and lysozyme and not with CD68 (KP-1). It is not associated with any systemic disease. Differentiation of granuloma annulare from necrobiosis lipoidica or rheumatoid nodules can be difficult because these lesions show similar histologic features.
16. Reactions to drugs can manifest as any of the following skin lesions EXCEPT:
a. Neutrophil-rich eccrine hidradenitis
b. Erythema multiforme
c. Photodermatitis
d. Eosinophil-rich lymphocytic vasculitis
e. Lichen simplex chronicus
View Answer
16. e. Drugs can cause various lesions in the skin, including maculopapular rashes, urticaria, vasculitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, fixed drug eruptions, lichenoid drug eruption, spongiotic reaction, psoriasiform reaction, photodermatitis, hyperpigmentation, and lupus erythematosus. Eccrine hidradenitis can result from reaction to some chemotherapeutic reagents.
17. Match each of the following pathologic findings (i-v) with their characteristic diseases listed below (a-e).
i) Subepidermal unilocular bullae
ii) Bullae with papillary microabscesses
iii) IgG “fish-net” immunofluorescence pattern in the epidermis
iv) Suprabasal epidermal bullae
v) Granular IgA staining at the tip of the dermal papillae
a. Dermatitis herpetiformis
b. Bullous pemphigoid
c. Erythema multiforme
d. Linear IgA bullous dermatosis
e. Pemphigus vulgaris
View Answer
17. i) b. ii) a. iii) e. iv) e. v) a. Intraepidermal bullae




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree