http://evolve.elsevier.com/Edmunds/NP/
One of the oldest and most widely prescribed primary care medications in the world is the glycoside digoxin. The principal indication for digoxin is HF. It is used for systolic HF, not diastolic, because of its inotropic properties. It is also used as an antiarrhythmic to control ventricular response to atrial tachyarrhythmia because it is an AV nodal blocker. Digoxin is the only glycoside that is in common use, and it is the only one discussed here. Although digoxin remains only one of the drugs used in the treatment of HF, its wide usage throughout the world, low cost, and narrow therapeutic window dictate that the clinician must understand how and when to use this product. (Additional drugs used in the treatment of HF are discussed in other chapters [Table 19-1].) Hospitalizations due to heart failure fell 29.5% in the United States between 1998 and 2008, possibly due to better control of risk factors.
TABLE 19-1
Other Medications Used for Heart Failure
| Drug | Chapter |
| Diuretics | 32 |
| ACEIs/ARBs | 22 |
| β-Blockers | 22 |
| Spironolactone | 32 |
| CCBs | 21 |
| Hydralazine | 17 |
| Nitrates | 18 |
Patients with HF commonly take at least two medications: a diuretic and an angiotensin-converting enzyme inhibitor (ACEI).
Because of its long half-life and narrow therapeutic window, patients treated with digoxin may easily become toxic. The elderly and those who are renally impaired are at increased risk for cardiac rhythm disturbance, as well as for toxicity from digoxin. Digoxin-induced arrhythmias must be differentiated from digoxin-treated ones, and the dose must be decreased, not increased.
Therapeutic Overview of Chronic Heart Failure
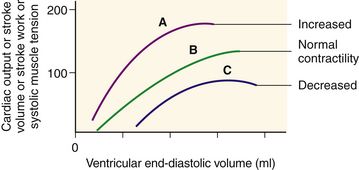
FIGURE 19-1 Frank-Starling law of the heart shows the relationship between length and tension in the heart.
End-diastolic volume determines end-diastolic length of ventricular muscle fibers and is proportional to tension generated during systole, as well as to cardiac output, stroke volume, and stroke work. A change in myocardial contractility causes the heart to perform on a different length-tension curve. A, Increased contractility. B, Normal contractility. C, Heart failure or decreased contractility. From McCance KL, Huether SE: Pathophysiology, ed 6, St Louis, 2010, Mosby.
Pathophysiology
HF usually originates with left-sided ventricular failure (Figure 19-2), which is systolic HF. This side is most affected by hypertension, valvular dysfunction, and coronary artery disease. When the ventricle fails to pump enough blood to meet the metabolic needs of the body, baroreceptors in the circulatory system cause reflex sympathetic nervous system activation. Veins and arteries constrict to increase critical organ, especially cardiac, perfusion. The Frank-Starling mechanism increases preload to increase myocardial contractile strength. HR increases, also to ensure perfusion. These changes reduce the blood flow to the kidneys, where receptors act to release renin, starting the angiotensin-aldosterone cascade, which leads to further vasoconstriction and sodium and water retention.
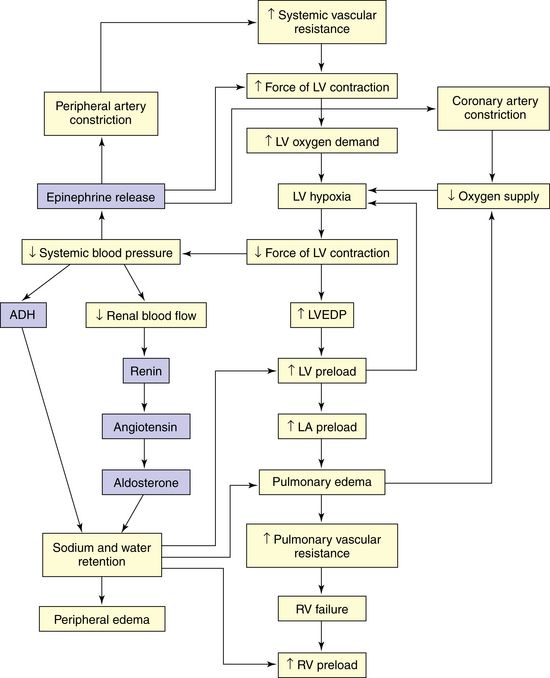
FIGURE 19-2 Left heart failure (CHF) from elevated systemic vascular resistance. Left-sided heart failure leads to right-sided heart failure. Systemic vascular resistance and preload are exacerbated by renal and adrenal mechanisms. ADH, Antidiuretic hormone; LA, left atrial; LV, left ventricular; LVEDP, left ventricular end-diastolic pressure; RV, right ventricular. (From Ignatavicius DD, Workman ML: Medical-Surgical Nursing: Patient-Centered Collaborative Care, ed 7, St Louis, 2013, Saunders.)
As HF progresses, the compensatory mechanisms can no longer maintain homeostasis. Rapid heart rhythm reduces the amount of blood pumped and, consequently, oxygen perfusion. Peripheral vasoconstriction forces the heart to pump harder, and the renin-angiotensin-aldosterone mechanism causes overfilling of the heart. The overall result is left-sided ventricular failure. The pulmonary system experiences increasing capillary pressure and fluid leakage into the interstitial space, resulting in pulmonary edema. As a further result, blood pools in the right ventricle, causing increased pressure in the systemic circulation (right-sided heart failure). This distends visceral veins, the liver and spleen become engorged, and jugular vein distention (JVD) and tissue edema in the extremities become evident, particularly in dependent areas such as the ankles and legs.
Diastolic HF is caused by a stiff left ventricle with decreased compliance and impaired relaxation, causing increased end-diastolic pressure. This leads to decreased ventricular filling. The causes and symptoms are similar to those of systolic failure, but the treatment may be different.
Disease Process
HF is a clinical syndrome characterized by signs and symptoms of volume overload and inadequate tissue perfusion. Common causes of HF are ischemic heart disease, systemic hypertension, valve disease, hypertrophic cardiomyopathy from end-stage hypertension, restrictive cardiomyopathy, hypothyroidism and hyperthyroidism, atrial fibrillation, and COPD.
Classification of Severity
Severity of HF is rated in accordance with the New York Heart Association (NYHA) functional classification system or its updated 1994 objective assessment system (Table 19-2).
Assessment
Perform a complete history and physical examination that includes measurement of lying, sitting, and standing BP and pulse. In general, left-sided heart failure manifests as pulmonary signs and symptoms; right-sided heart failure causes systemic signs and symptoms. Both left- and right-sided heart failure are present in most patients. The onset is often gradual and subtle. Left-sided symptoms include paroxysmal nocturnal dyspnea (PND), dyspnea on exertion (DOE), S3 (S4 may be present with hypertension) heart sounds, arrhythmias, and pulsus alternans. Right-sided symptoms include fatigue, syncope, decreased exercise tolerance, hepatomegaly, peripheral edema, JVD, ascites, decreased appetite, and early satiety.
Perform diagnostic tests (Table 19-3) to rule out other possible causes for the symptoms, to determine underlying causes of HF, and to establish a baseline from which to monitor the patient. Obtain a complete blood count because anemia can mask heart failure symptoms. Renal function studies are especially important for dosage determination. Potassium levels are crucial because of the risk for arrhythmia. Obtain blood glucose testing because the risk of heart failure was found to be 2.4- and 5-fold increased in men and women, respectively, in the Framingham study. Order thyroid function tests, especially if atrial fibrillation is detected. Brain natriuretic peptide (BNP) is an FDA-approved diagnostic tool that is a reliable measure of cardiac function in both systolic and diastolic failure. A low BNP rules out HF; BNP may have a role in monitoring of patients with HF. Classify HF according to systolic or diastolic heart failure to determine appropriate treatment.
TABLE 19-3
Recommended Tests for Patients with Signs and Symptoms of Chronic Heart Failure
| Test Recommended | Findings | Suspected Diagnosis |
| CBC | Anemia | Heart failure caused or aggravated by decreased oxygen-carrying capacity |
| ECG | Acute ST-T wave changes | MI |
| Atrial fibrillation- | Thyroid disease, rapid ventricular rate | |
| tachyarrhythmia | Sick heart | |
| Bradyarrhythmia | Diastolic dysfunction | |
| Left ventricular | Pericardial effusion | |
| hypertrophy | Reduced left ventricular performance | |
| Low voltage | ||
| Previous MI | ||
| Serum albumin | Decreased | Increased extravascular volume caused by hypoalbuminemia |
| Serum creatinine | Elevated | Volume overload caused by renal failure |
| Thyroid studies: T4 and TSH | Abnormal T4 | Hypothyroidism |
| Abnormal TSH | Hyperthyroidism | |
| Urinalysis | Red blood cells and cellular casts | Glomerulonephritis |
| Proteinuria | Nephrotic syndrome |
Modified from AHCPR: Quick reference guide for clinicians, Publication No. 94-0613, Washington, DC, 1994, U.S. Government Printing Office.
Examine results from ECG and chest x-ray to identify any treatable causes of HF. The chest x-ray may show pulmonary congestion and cardiomegaly, which are consistent with HF. The ECG is usually abnormal in symptomatic patients with systolic HF. Echocardiograms also help in assessment of left ventricular function and in measurement of ejection fraction. In a person with HF, an ejection fraction less than 40% means left ventricular dysfunction or systolic heart failure; a normal ejection fraction >50% indicates diastolic heart failure. Systolic dysfunction is associated with reduced contractility and increased left ventricular end-diastolic volume. Diastolic dysfunction is associated with reduced ventricular filling. Table 19-4 lists factors that may precipitate an episode.
TABLE 19-4
Common Precipitating Factors for Chronic Heart Failure
| General Factors | Specific Factors |
| Patient factors | Alcohol intake |
| Excessive fluid intake | |
| Excessive salt intake | |
| Increased physical or mental stress | |
| Noncompliance with medication regimen | |
| Obesity, weight gain | |
| Progression of basic cause | Increasing hypertension, coronary artery disease |
| Increased cardiac workload | Arrhythmia (possibly caused by digoxin) |
| Electrolyte and acid-base abnormalities | |
| Increased or decreased blood volume, anemia | |
| Infection (cardiovascular or other, such as urinary tract infection) | |
| Pulmonary embolism | |
| Renal insufficiency | |
| Medications that impair cardiac performance | Cardiovascular drugs |
| Antiarrhythmics | |
| β-Blockers | |
| Calcium channel blockers | |
| Digoxin | |
| Corticosteroids | |
| Drugs that cause fluid retention | |
| NSAIDs |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Key drug.
Key drug. The potential for toxicity or lack of efficacy are the major disadvantages of digoxin use.
The potential for toxicity or lack of efficacy are the major disadvantages of digoxin use.