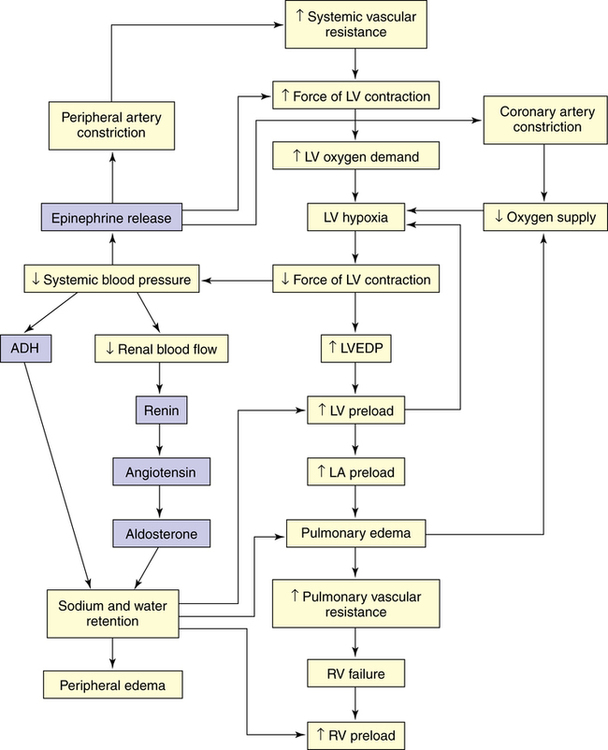
Chapter 19 One of the oldest and most widely prescribed primary care medications in the world is the glycoside digoxin. The principal indication for digoxin is HF. It is used for systolic HF, not diastolic, because of its inotropic properties. It is also used as an antiarrhythmic to control ventricular response to atrial tachyarrhythmia because it is an AV nodal blocker. Digoxin is the only glycoside that is in common use, and it is the only one discussed here. Although digoxin remains only one of the drugs used in the treatment of HF, its wide usage throughout the world, low cost, and narrow therapeutic window dictate that the clinician must understand how and when to use this product. (Additional drugs used in the treatment of HF are discussed in other chapters [Table 19-1].) Hospitalizations due to heart failure fell 29.5% in the United States between 1998 and 2008, possibly due to better control of risk factors. TABLE 19-1 Other Medications Used for Heart Failure • Cardiac output (CO) is the volume of blood ejected from the heart/unit time. • Stroke volume (SV) is the volume of blood ejected with each beat. • Heart rate (HR) is the number of beats/minute. • Calculation of CO: CO = SV × HR • Left ventricular work and myocardial oxygen consumption depend on HR and blood pressure (HR × BP). • BP = CO × systemic vascular resistance (SVR) (afterload) • Afterload is the force against which the ventricle must contract to eject blood, or the arterial pressure, arterial impedance, or resistance. • Preload refers to the amount of blood going to the heart and the filling pressure created by systemic vascular resistance. • The Frank-Starling law of the heart: Within limits, an increase in left ventricular filling increases the ventricular force of contractions, which increases the SV. After optimal filling is attained, increased volume no longer increases the SV. This is when the heart begins to fail. The Frank-Starling law keeps the output of the two ventricles balanced (Figure 19-1). HF usually originates with left-sided ventricular failure (Figure 19-2), which is systolic HF. This side is most affected by hypertension, valvular dysfunction, and coronary artery disease. When the ventricle fails to pump enough blood to meet the metabolic needs of the body, baroreceptors in the circulatory system cause reflex sympathetic nervous system activation. Veins and arteries constrict to increase critical organ, especially cardiac, perfusion. The Frank-Starling mechanism increases preload to increase myocardial contractile strength. HR increases, also to ensure perfusion. These changes reduce the blood flow to the kidneys, where receptors act to release renin, starting the angiotensin-aldosterone cascade, which leads to further vasoconstriction and sodium and water retention. Severity of HF is rated in accordance with the New York Heart Association (NYHA) functional classification system or its updated 1994 objective assessment system (Table 19-2). TABLE 19-2 New York Heart Association Classification of Severity of Heart Failure∗ ∗When there is reasonable uncertainty that the patient’s symptoms are due to cardiac disease, the diagnosis should be No heart disease. The Criteria Committee of the New York Heart Association: Nomenclature and criteria for diagnosis of diseases of the heart and great vessels, ed 9, Boston, 1994, Little, Brown & Co. Perform diagnostic tests (Table 19-3) to rule out other possible causes for the symptoms, to determine underlying causes of HF, and to establish a baseline from which to monitor the patient. Obtain a complete blood count because anemia can mask heart failure symptoms. Renal function studies are especially important for dosage determination. Potassium levels are crucial because of the risk for arrhythmia. Obtain blood glucose testing because the risk of heart failure was found to be 2.4- and 5-fold increased in men and women, respectively, in the Framingham study. Order thyroid function tests, especially if atrial fibrillation is detected. Brain natriuretic peptide (BNP) is an FDA-approved diagnostic tool that is a reliable measure of cardiac function in both systolic and diastolic failure. A low BNP rules out HF; BNP may have a role in monitoring of patients with HF. Classify HF according to systolic or diastolic heart failure to determine appropriate treatment. TABLE 19-3 Recommended Tests for Patients with Signs and Symptoms of Chronic Heart Failure Modified from AHCPR: Quick reference guide for clinicians, Publication No. 94-0613, Washington, DC, 1994, U.S. Government Printing Office.
Heart Failure and Digoxin
Drug
Chapter
Diuretics
32
ACEIs/ARBs
22
β-Blockers
22
Spironolactone
32
CCBs
21
Hydralazine
17
Nitrates
18
Therapeutic Overview of Chronic Heart Failure
Anatomy and Physiology
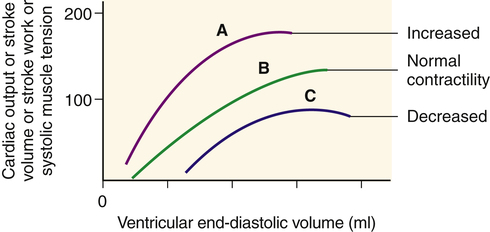
End-diastolic volume determines end-diastolic length of ventricular muscle fibers and is proportional to tension generated during systole, as well as to cardiac output, stroke volume, and stroke work. A change in myocardial contractility causes the heart to perform on a different length-tension curve. A, Increased contractility. B, Normal contractility. C, Heart failure or decreased contractility. From McCance KL, Huether SE: Pathophysiology, ed 6, St Louis, 2010, Mosby.
Pathophysiology
Disease Process
Classification of Severity
Functional Capacity
Objective Assessment
Class I: Patients with cardiac disease but without resultant limitation in physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea, or anginal pain.
A. No objective evidence of cardiovascular disease
Class II: Patients with cardiac disease resulting in slight limitation in physical activity. They are comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea, or anginal pain.
B. Objective evidence of minimal cardiovascular disease
Class III: Patients with cardiac disease resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary activity causes fatigue, palpitation, dyspnea, or anginal pain.
C. Objective evidence of moderately severe cardiovascular disease
Class IV: Patients with cardiac disease resulting in inability to carry on any physical activity without discomfort. Symptoms of heart failure or the anginal syndrome may be present even at rest. If any physical activity is undertaken, discomfort is increased.
D. Objective evidence of severe cardiovascular disease
Assessment
Test Recommended
Findings
Suspected Diagnosis
CBC
Anemia
Heart failure caused or aggravated by decreased oxygen-carrying capacity
ECG
Acute ST-T wave changes
MI
Atrial fibrillation-
Thyroid disease, rapid ventricular rate
tachyarrhythmia
Sick heart
Bradyarrhythmia
Diastolic dysfunction
Left ventricular
Pericardial effusion
hypertrophy
Reduced left ventricular performance
Low voltage
Previous MI
Serum albumin
Decreased
Increased extravascular volume caused by hypoalbuminemia
Serum creatinine
Elevated
Volume overload caused by renal failure
Thyroid studies: T4 and TSH
Abnormal T4
Hypothyroidism
Abnormal TSH
Hyperthyroidism
Urinalysis
Red blood cells and cellular casts
Glomerulonephritis
Proteinuria
Nephrotic syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Heart Failure and Digoxin
Only gold members can continue reading. Log In or Register to continue