The big picture237
14.1. The big picture
Skeleton
Nerves
Arteries
Veins
Lymph nodes
14.2. Skull bones and joints, cranial cavity
Bones
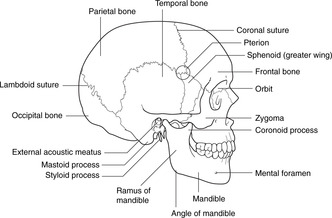
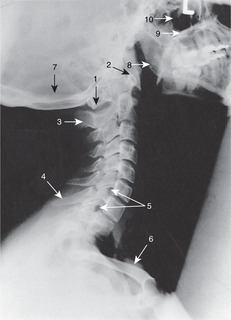
Fig. 14.2
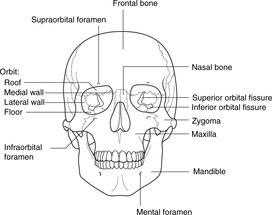
Fig. 14.3
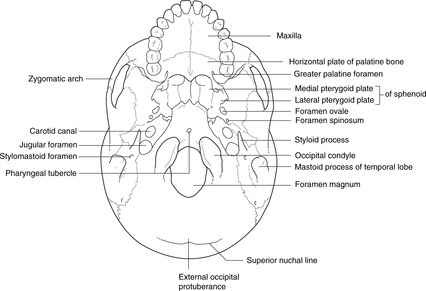
Fig. 14.4
Mandible (Fig. 14.6)
Occipital bone (Figs 14.4, 14.5)
Sphenoid bone (Fig. 14.5)
Temporal bone (Figs 14.2, 14.4, 14.5)
Bones worth only a brief survey
Bones you need only to have heard of
Internal aspect of the cranium, cranial fossas (Fig. 14.5)
Skull foramina
Bone
Name
Contents
Effect of damage at the foramen
Ethmoid
Cribriform plate
I
Post-traumatic anosmia and CSF rhinorrhoea
Sphenoid
Optic foramen
II, ophthalmic artery
Not likely, eye blindness
Superior orbital fissure
III, IV, Va, VI
Fractures may cause squints
Foramen rotundum
Vb
Not likely
Foramen ovale
Vc
Not likely
Foramen spinosum
Middle meningeal artery
Not likely
Sphenoid/temporal
Carotid canal
Internal carotid artery
Not likely
Mandible
Inferior alveolar
Inferior alveolar nerve and vessels
Mandibular fractures may damage this nerve (mental anaesthesia)
Mental
Mental nerve
Mental anaesthesia
Temporal bone
Stylomastoid foramen
VII
Facial palsy, weakness
Internal acoustic meatus
VII, VIII
Deafness, balance disorders
Occipital/temporal
Jugular foramen
IX, X, XI, internal jugular vein
Not likely
Occipital
Hypoglossal canal
XII
Not likely
Foramen magnum
Lower brain stem, vertebral arteries, XI, meninges
Trunk and limbs paralysis, death
Joints and growth of the skull
Sutures (Fig. 14.2)
Primary cartilaginous joints
Synovial joints
Fetal and neonatal skull
Fontanelles
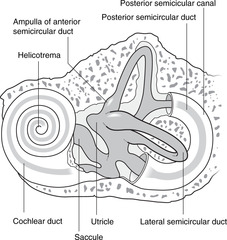
Fig. 14.37
Cephalhaematoma
14.3. Cervical vertebrae, joints and muscles of the neck
Vertebrae C3–7
Vertebra C2, the axis (Fig. 14.8)
Vertebra C1, the atlas (Fig. 14.8)
Joints of the cervical vertebral column
Joints below C2
C2–1: atlanto-axial joints and ligaments (Fig. 14.8)
Atlanto-occipital joints
Notochordal remnants
Movements of the cervical spine
Muscles (Fig. 14.9)
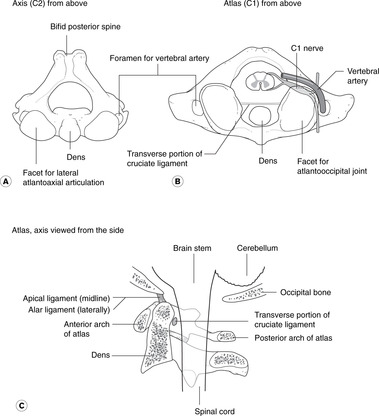
Fig. 14.9
Flexion, lateral flexion
Extension
Greater occipital nerve, C2
14.4. Cranial nerves
Functions, attachments and skull foramina of cranial nerves (Table 14.2)
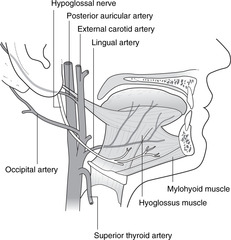
Fig. 14.14
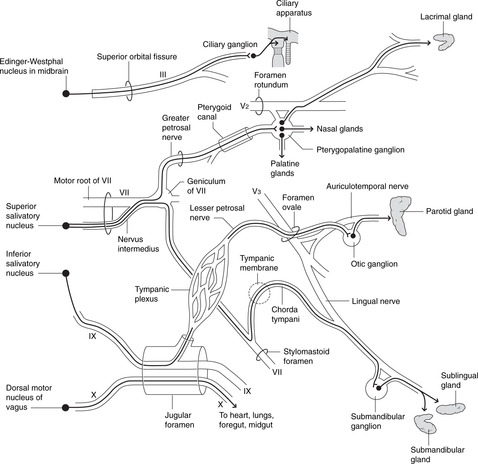
Fig. 14.15
Nerve
Type
Main function (less important functions in brackets
Typical symptoms of damaged nerve
I Olfactory
Sensory
Smell
Anosmia
II Optic
Sensory
Vision
Visual impairment
III Oculomotor
Motor
Movements of eyeball, upper eyelid
Squints, ptosis
Parasympathetic: pupilloconstriction, accommodation
Dilated pupil, poor accommodation
IV Trochlear
Motor
Superior oblique (only)
Squint
V Trigeminal
Mixed
Va Ophthalmic
Sensory
Eyeball, anterior scalp, upper face
Sensory loss in affected area
Vb Maxillary
Sensory
Nasal cavity and sinuses, palate, upper teeth, mid-face
Sensory loss in affected area
Vc Mandibular
Motor
Muscles of mastication
Impaired chewing
Sensory
Chin, temple, oral cavity, tongue, temporomandibular joint, lower teeth, ear
Sensory loss in affected area
VI Abducens
Motor
Lateral rectus (only)
Medial squint
VII Facial
Mixed
Motor
Muscles of facial expression
Facial palsy, weakness
(Motor)
(Parasympathetic: lacrimal, nasal, palatine, submandibular, sublingual glands)
(Dry mouth)
(Sensory)
(Taste, anterior tongue)
(Loss of taste)
VIII Vestibulocochlear
Sensory
Balance and position in space, hearing
Disturbance of balance and/or deafness
IX Glossopharyngeal
Mixed
Sensory
Oropharynx, posterior tongue, carotid body and sinus
Not often involved in disease
(Sensory)
(Taste, posterior tongue)
Loss of taste
(Motor)
(Stylopharyngeus)
(Motor)
(Parasympathetic, parotid gland)
Dry mouth
X Vagus
Mixed
Motor
Muscles of pharynx, larynx for swallowing, phonation
Impaired swallowing, hoarseness of voice (depends upon site of lesion)
(Motor)
(Parasympathetic: cardiac muscle; muscles and glands of foregut and midgut)
Not much
Sensory
Sensation from ear, pharynx, larynx
Abolition of cough reflex
(Sensory)
(Sensation from heart, lungs, abdominal viscera)
(Sensory)
(Taste: epiglottic region)
Loss of taste, abolition of cough reflex
XI Accessory
Motor
Sternocleidomastoid, trapezius
Limited head and neck movements and shoulder abduction beyond 90°
XII Hypoglossal
Motor
Tongue muscles
Impaired chewing and speaking
Cranial nerve attachments and skull foramina (Table 14.3)
Brain attachment
Nerve
Foramen or canal (cranial bone in brackets)
Forebrain
Cerebral cortex, frontal lobes
I
Cribriform plate (ethmoid)
Diencephalon
II
Optic canal (sphenoid)
Midbrain
Upper, ventral aspect
III
Superior orbital fissure (sphenoid)
Lower, dorsal aspect
IV
Superior orbital fissure (sphenoid)
Hindbrain
Pons
V
Va
Superior orbital fissure (sphenoid)
Vb
Foramen rotundum (sphenoid)
Vc
Foramen ovale (sphenoid)
Pontomedullary junction, medial
VI
Superior orbital fissure (sphenoid)
Cerebellopontine angle
VII
Internal acoustic meatus, facial canal, stylomastoid foramen (temporal)
Cerebellopontine angle
VIII
Internal acoustic meatus (temporal)
Medulla
IX, X
Jugular foramen (between occipital and temporal)
Medulla, spinal cord
XI
Jugular foramen (between occipital and temporal): see text
Medulla
XII
Hypoglossal canal (occipital)
Olfactory nerve: I
Oculomotor nerve: III
Trochlear nerve: IV
Trigeminal nerve: V (Fig. 14.10)
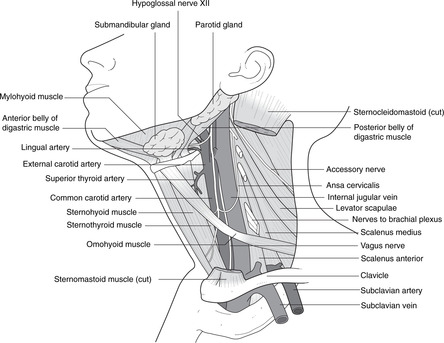
Fig. 14.10
Clinical notes
Ophthalmic nerve: Va
Origin, course and branches.
Clinical testing
Maxillary nerve: Vb
Origin, course and branches
Clinical testing
Mandibular nerve: Vc
Origin, course and branches
First branchial arch
Clinical testing
Abducens nerve: VI
Facial nerve: VII (Fig. 14.11)
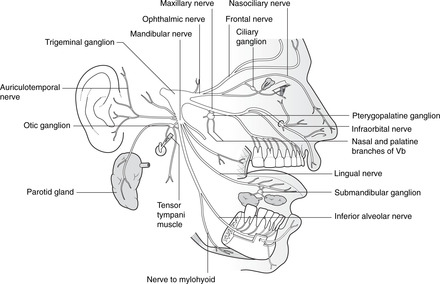
Fig. 14.11
Origin, course and branches
Intracranial course, within the cranial cavity and temporal bone
Extracranial course and branches
Second branchial arch, otic vesicle and facial nerve
Clinical notes
Clinical testing
Vestibulocochlear nerve: VIII
Glossopharyngeal nerve: IX
Origin, course and branches
Third branchial arch
Clinical testing
Vagus nerve: X (Fig. 14.12)
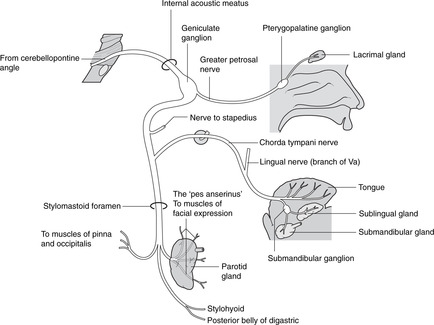
Fig. 14.12
Origin, course and branches
Fourth and sixth branchial arches
An alternative view of the vagus
Clinical testing
Accessory nerve: XI
Origin and course: there are two foramina
Clinical testing
Hypoglossal nerve: XII (Fig. 14.13)
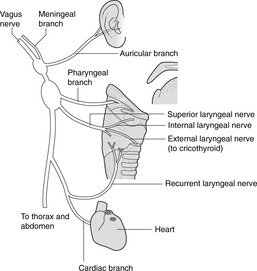
Fig. 14.13
Origin, course and branches
Clinical testing
Parasympathetics and taste in cranial nerves
Parasympathetic components (Fig. 14.14)
Taste fibres (Fig. 14.15)
Clinical testing
14.5. Neck
Fascial layers (Fig. 14.16)

Fig. 14.16
Visceral skeleton of the neck
Vertebral levels of the visceral skeleton of the neck
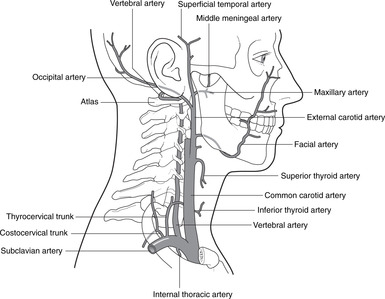
Arteries of the neck (Figs 14.17, 14.18)
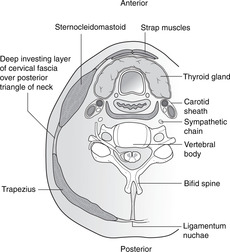
Fig. 14.17
Internal carotid artery
External carotid artery (Fig. 14.18)
Carotid pulse
Superficial temporal pulse
Vertebral artery
Veins of the neck
Internal jugular vein
External jugular vein
Anterior jugular veins
Surface markings of neck veins
Jugular venous pulsation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Head and neck
14.2 Skull bones and joints, cranial cavity238
14.3 Cervical vertebrae, joints and muscles of the neck243
14.4 Cranial nerves247
14.5 Neck257
14.6 Face, parotid, VII, scalp264
14.7 Anatomy of mastication268
14.8 Anatomy of swallowing and phonation273
14.9 Nose, nasal sinuses and the sense of smell: cranial nerve I279
14.10 Ear, hearing and vestibular function: cranial nerve VIII282
14.11 Orbit, eye movements, vision, visual reflexes; cranial nerves II, III, IV, VI288
14.12 Inside the skull, haemorrhages295
14.13 Sympathetic impulses to the head299
The head houses the brain, main sense organs and the upper end of the respiratory and alimentary systems. Twelve pairs of cranial nerves arise from the brain. Arterial blood comes from the common carotid and vertebral arteries. Veins drain principally to the internal jugular vein, and lymph to the deep cervical chain.
The skeleton of the head and neck serves several functions. Some of its components, the neurocranium, protect the brain and organs of the special senses. Some components, the viscerocranium, provide structural support for the cranial end of the gut tube and attachments for its muscles. Cervical vertebrae provide structural support for the head and muscle attachments for head and neck movements, and cartilages in the anterior neck provide a structural framework for the upper end of the respiratory system and attachments for muscles of phonation.
• Cranial nerves. The 12 pairs of nerves that pass through or into the skull bones are probably the most important aspects of head and neck anatomy as far as the general physician is concerned. They serve various functions:
– special senses: olfaction, vision, balance, hearing
– sustenance: ingestion, digestion
– communication: facial expression, speaking.
A survey and analysis of the cranial nerves follows (section 14.4, p. 247) to provide a foundation for their various aspects that appear and reappear as the several regions and functions of the head and neck are considered. Cranial nerves are referred to by Roman numerals, I, II, III, etc.
• Cervical spinal nerves 1–8 supply structures in the neck and contribute to the innervation of the upper limb, upper thoracic skin and diaphragm. They are similar in form and function to other spinal nerves.
The brain attempts to integrate, coordinate and control these neural functions.
• Carotid system. The right and left common carotid arteries bifurcate to give the internal and external carotid arteries of each side.
– External carotid arteries give branches in the neck to supply the neck, scalp, skull bones and cranial dura mater.
– Branches of the two carotid systems communicate, particularly in the scalp and around the orbit.
• Vertebrobasilar system. The vertebral arteries supply the cervical vertebrae and spinal cord. They enter the cranial cavity through the foramen magnum, uniting to form the basilar artery, which supplies the brain stem. It terminates by contributing to the arterial circle of Willis with the internal carotids.
• The arterial circle of Willis supplies the brain.
• Dural venous sinuses within the cranium: these form an intracranial network of veins that receive blood from the brain and drain to the:
• Internal jugular veins: deep veins in the neck, with tributaries from the face and neck.
• External and anterior jugular veins: superficial veins from the skull, face and superficial tissues.
• There are many communicating channels between the internal and external systems.
• Venous blood from the cranial cavity also drains through the foramen magnum to the internal vertebral venous plexus of the vertebral column.
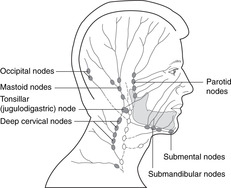
• Groups of lymph nodes, many palpable, are shown in Figure 14.1. In the head, lymph from a particular organ or region passes, in general, to whichever group of nodes is nearest. These then drain to the deep cervical chain and thence to the venous system at the union of the internal jugular and subclavian veins. The palpable lymph node at the top of the deep cervical chain, just behind the angle of the mandible, is the jugulodigastric or tonsillar node, so called because it is the node most commonly affected in tonsillitis. If you suffered as a child from frequent attacks of tonsillitis, you may have a permanently enlarged tonsillar node.
• The entrance to the gut tube is surrounded by Waldeyer’s ring of lymphoid tissue: tonsils, adenoids, and lingual tonsils. This is continuous with the upper end of the deep cervical chain and drains to it.
• Retropharyngeal nodes. Involvement of nodes between the vertebral column and the pharynx is dangerous. The nodes are deep and therefore impalpable, so if disease spreads to this group of nodes, it is likely to go undetected until it has also spread elsewhere, by which time it is likely to be too late for effective treatment. Retropharyngeal nodes are connected to the deep cervical nodes of both sides and so provide a pathway for lymphatic spread across the midline.
The skull is made up of several separate bones united by fibrous sutures. The only synovial joint in the skull is the temporomandibular joint at which the movements of chewing occur. The internal aspect of the cranium is divided into three cranial fossas. There are numerous named foramina to allow structures to pass through the cranium. The fetal skull is different from the adult skull in a number of ways apart from size.
There are two types of skull bones:
• Neurocranium: flat bones of the vault of the skull. These consist of two plates of cortical bone, inner and outer tables or diploë, between which is the diploic cavity containing marrow. This is a site of haemopoiesis and so has a rich blood supply.
• Viscerocranium: these are bones of the base of the skull surrounding the nasal cavity and sinuses, oral cavity, pharynx and larynx.
Study the bones of the skull (Fig. 14.2, Fig. 14.3, Fig. 14.4, Fig. 14.5 and Fig. 14.6). Most of them reach the external surface of the skull, so identify and palpate them on yourself. Four of them (see below) are worth studying in some detail.
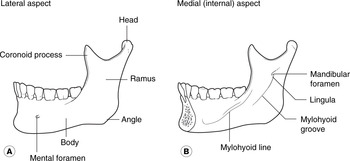
The right and left mandibles fuse in the second year after birth.
• Body and ramus, lateral aspect:
– mental foramen
– angle.
• Body and ramus, medial (internal) aspect:
– angle
– mandibular foramen, lingula
– mylohyoid line and groove.
• Alveolar (teeth) sockets.
• Coronoid process.
• Neck, head (condyle), articular surface.
• Basi-occiput: equivalent to the vertebral bodies below:
– foramen magnum
– condyles: convex, for the reciprocal surface of the atlas
– hypoglossal (condylar) canal
– pharyngeal tubercle.
• Squamous part, external aspect:
– external occipital protuberance
– superior nuchal lines.
• Squamous part, internal aspect:
– internal occipital protuberance, ridges for meningeal attachments.
• Body, articulating with the basi-occiput.
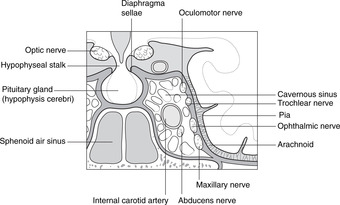
• Sphenoid air sinus.
• Pituitary fossa (sella turcica), dorsum sellae, clinoid processes.
• Greater wing, lesser wing, optic foramen, superior orbital fissure, foramen rotundum, foramen ovale, foramen spinosum, spine (inferior aspect).
• Lateral and medial pterygoid plates, hamulus (palpable in the mouth behind and medial to the third upper molar).
• Petrous temporal: ridge and apex.
• Internal acoustic (internal auditory) meatus.
• Mastoid process, mastoid antrum and air cells, middle ear cavity, orifice for Eustachian tube.
• Squamous temporal.
• External acoustic (external auditory) meatus.
• Articular (condylar) surface for the head of the mandible.
• Zygomatic process forming the zygomatic arch with the zygoma.
• Carotid canal, foramen lacerum.
• Styloid process.
• Stylomastoid foramen.
Pterion (Fig. 14.2). This is an area on the lateral side of the skull where the frontal, parietal, temporal and sphenoid bones meet. Its surface marking is about 4 cm above a point one-third of the way from ear to eye. Its importance will be pointed out later (p. 296).
• Parietal: diploë, grooves for meningeal vessels.
• Frontal: supraorbital margin and notch, frontal sinus.
• Zygoma: zygomatic arch formed by zygoma and temporal bone.
• Ethmoid: crista galli, perpendicular plate, cribriform plate, ethmoid sinuses, superior and middle turbinates.
• Vomer: a midline, unpaired, bone forming the posterior part of the nasal septum.
• Lacrimal bone: on the anteromedial aspect of the orbit, near the opening of the nasolacrimal duct.
• Inferior turbinate: the lowest of the three bones projecting into the nasal cavity from the lateral wall (the other two are parts of the ethmoid).
• Palatine: deep in the skull, forming the posterolateral palate and part of the lateral side of the nasal cavity.
• Nasal bone: the bony part of the nasal bridge, sometimes fractured.
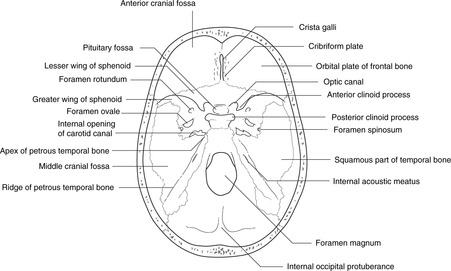
• The floor of the internal aspect of the cranial cavity is divided into three cranial fossas:
– Anterior cranial fossa: anterior to the lesser wing of the sphenoid, related to the frontal lobes of the brain and the olfactory bulbs. Its features include the cribriform plate and crista galli of the ethmoid.
– Middle cranial fossa: between the lesser wings of the sphenoid and the ridge of the petrous temporal bones, related to the temporal lobes and cavernous (venous) sinus. Its features include the pituitary fossa, foramina for cranial nerves II–VI, the carotid canal, and foramen spinosum.
– Posterior cranial fossa: posterior to the ridge of the petrous temporal bone, related to the medulla, pons and cerebellum. It is covered by the tentorium cerebelli. Its features include foramina for cranial nerves VII–XII and the foramen magnum.
• The vault of the skull is formed by frontal, parietal, squamous temporal and squamous occipital bones. The internal aspect of the vault displays grooves for meningeal vessels supplying bones and dura, and ridges for dural attachments forming intracranial partitions and the edges of the dural venous sinuses.
• Cranial meninges, meningeal vessels and venous sinuses are described in section 14.12 (p. 296).
Although not all these are important clinically, they are given here for the sake of completeness (Table 14.1). The list is not exhaustive.
Sutures are fibrous joints (see section 4.2, p. 21), the most important being:
• coronal – between the frontal bone and the two parietal bones
• sagittal – between the two parietal bones
• lambdoid – between the parietal bones and the occipital bone.
Suture lines are irregular and sometimes contain islands of bone (sutural bones, of no significance). Once sutures have fused no movement is possible, but before that there may be a little and the edges of the sutures may overlap. This is particularly so during childbirth when the fetal skull is deformed as it passes through the mother’s pelvis. Growth at the sutures stops at about puberty, after which they are gradually obliterated from inside out. The metopic suture between the two frontal bones fuses during childhood (but may persist for longer), the sagittal suture fuses in the third decade, and those around the temporal bone may be present until old age.
The joint between the occipital and sphenoid bones is a primary cartilaginous joint (see section 4.2, p. 21). Fusion of these bones occurs when anteroposterior growth ceases after puberty, usually in the mid-20s.
There is only one on each side, the temporomandibular joint (see p. 268).
Until the bones are completely ossified, the defects between them are occupied by fibrous connective tissue. Two such areas are large at birth:
• posterior fontanelle, in the midline between the occipital and parietal bones; it closes in the first 6 months of postnatal life
• anterior fontanelle, in the midline between the frontal and parietal bones; it closes between 18 months and 2 years after birth. It is clinically useful:
– It can be used to assess intracranial pressure and the state of hydration. In a healthy baby it should be slightly convex and ‘give’ only a little to the touch, but if the child is dehydrated the fontanelle will be concave and feel ‘floppy’. In raised intracranial pressure it may bulge markedly.
– Through it, drugs can be injected into the subarachnoid space and samples of cerebrospinal fluid can be withdrawn more easily than by performing a lumbar puncture. Beware: a needle inserted in the midline will yield blood, not cerebrospinal fluid, because of the superior sagittal sinus: see Figure 14.37.
A cephalhaematoma is a subperiosteal haemorrhage: the blood collects between the bone itself and the overlying periosteum. It may occur during birth, possibly as a result of the inept use during delivery of forceps or some other mechanical extraction device. The haematoma is limited to the shape of the underlying bone, because the periosteum is attached to the bone at the sutures.
Three of the more obvious differences between the neonatal skull and a mature skull are:
• Size: always state the obvious.
• Several protuberances of the skull bones form as a result of muscular attachments, of which a good example is the mastoid process, which develops postnatally as a result of the action of sternocleidomastoid. The lack of a mastoid process means that the facial nerve emerging from the stylomastoid foramen is superficial and vulnerable.
• As a proportion of the skull as a whole, the face is much smaller in the newborn, reflecting the fact that the child has not yet had to use its gut tube for sustenance.
There are seven cervical vertebrae with special functional adaptations in C1 and C2 to allow for nodding and rotation. Elsewhere, features of cervical vertebrae are similar to those of other vertebrae. The cervical spine is more mobile than other regions of the vertebral column.
Revise the features of a typical vertebra (see Fig. 5.1, p. 26). Vertebrae C3–7 are typical cervical vertebrae (see section 5.4, p. 26), the particular features of which are:
• triangular vertebral canal
• foramen in the transverse process (foramen transversarium) for vertebral vessels
• anterior and posterior tubercles on the transverse processes
• bifid posterior spinous process for the attachment of a tough nuchal ligament (ligamentum nuchae).
• Vertebra C2 can be thought of as a typical cervical vertebra with its body extended upwards to form the dens (tooth) or odontoid (tooth-like) process. This is a pivot around which vertebra C1 rotates. Embryologically, the dens is the body of C1, which has fused with C2, so there is no intervertebral disc between C1 and C2.
• There are large articular facets on the upper surface of the lateral sides of the body: these are the articulations for gliding movements with the atlas. Unlike facet joints elsewhere in the vertebral column, these are anterior to the emerging spinal nerves.
Noteworthy features of the atlas are:
• it has no body (see above)
• anterior arch, the posterior surface of which has a facet for articulation with the dens
• posterior arch
• lateral masses where the anterior and posterior arches meet, palpable immediately behind the angle of the mandible (the atlas is surprisingly wide)
• inferior articular facets for reciprocal surfaces on the axis (see above)
• superior articular facets, concave, for the convex occipital condyles, for nodding movements
• groove for the vertebral artery (see below) on the superior surface.
The atlas is higher than you might think: it lies behind the mouth, so radiographs of the dens and atlas are taken through the open mouth (if the mouth were closed, teeth would obscure the radiographic view).
These are as described in Chapter 5 (section 5.5, p. 27). There are symphyses with intervertebral discs in the midline and the facet joints laterally. The mobility of the cervical vertebral column means that there is considerable wear and tear on the facet joints and disease of them can cause cervical nerve root irritation and neck pain.
• In the midline. There is a synovial joint between the dens and the back of the anterior arch of the atlas (where facets may be seen), and a synovial bursa between the dens and the cruciate ligament behind it. The dens is kept in place by the cruciate ligament.
• Laterally. The lateral articular surfaces are flat to allow for gliding movements during rotation.
Cruciate ligament (Fig. 14.8). This cross-shaped ligament separates the dens from the spinal meninges. The horizontal component of the ligament is attached to the sides of the spinal canal, and the vertical component runs from the lower part of the body of C2 to the occipital bone above. There is a synovial bursa between the ligament and the posterior aspect of the dens.
These are synovial joints with reciprocally curved surfaces for nodding. They are anterior to the spinal nerves as they emerge from the intervertebral foramen.
Midline structures in this region (dens, apical ligament) are derived form the notochord, and tumours of notochordal remnants, chordomas, occasionally develop here.
Flexion and extension occur, as in the rest of the vertebral column. Lateral flexion and rotation are not limited by ribs, as they are in the thorax. The cumulative result of smaller movements between adjacent vertebrae adds up to great flexibility.
• Sternocleidomastoid. Attachments: sternum, clavicle–mastoid process. Nerve supply: accessory nerve (cranial XI). Sternocleidomastoid flexes the cervical spine and moves the chin upwards and away from the muscle. It is a good test of accessory nerve function: to test the right accessory nerve, ask the patient to rotate his head to the left against the resistance of your hand on his chin.
• Scalene muscles: lateral flexion. Nerve supply: branches from cervical nerves. These muscles arise from the transverse processes of C3–6, scalenus anterior passing to the first rib between the subclavian vein and artery, and scalenus medius passing to the first rib behind the subclavian artery (see section 10.4, p. 87).
• Prevertebral (longus) muscles run between anterior aspects of upper thoracic and cervical vertebrae and the skull. You need only know that they exist.
• Trapezius. Attachments: external occipital protuberance and nuchal ligament – spine and acromion of scapula. Nerve supply: accessory nerve (cranial XI). Trapezius extends the head and cervical spine and its role in shoulder abduction has been considered (section 12.3, p. 174). Shrugging the shoulders against resistance is a test of accessory nerve function.
• Postvertebral muscles (‘erector spinae’) muscles (see section 5.5, p. 27). Nerve supply: dorsal rami of spinal nerves.
• Small suboccipital muscles run between the atlas, the spinous process of the axis and the occipital bone and are supplied by branches of C1 and C2 nerves. They are responsible for movements that take place from minute to minute as we move our heads for listening, expressing emotion, talking, viewing and listening. You need know nothing of their detailed anatomy.
The greater occipital nerve is the dorsal ramus of C2. It is a large sensory nerve which emerges posteriorly between vertebrae C1 and C2, and passes backwards between the suboccipital muscles before turning upwards to supply the skin of the back of the head and scalp as far forwards as the vertex. It has been suggested that compression of the nerve in the suboccipital region, perhaps by muscular tension, may be the cause of many headaches – a theory which has not been disproved – so perhaps there is something in the postural exercises advocated by adherents of the Alexander technique who maintain that certain relaxation exercises involving the cervical spine and skull can improve posture, lessen neck pain and generally promote a feeling of well-being.
You will need to return to this section repeatedly as you come across cranial nerves in other parts of the text.
Cranial nerves arise from the brain and are numbered I–XII roughly in the order that they arise. Some are simple, either motor nerves or sensory nerves; some are complex: mixed motor and sensory, with parasympathetic and other impulses travelling with them and their branches on what appears at first sight to be a haphazard basis. Despite the complexity of some cranial nerves (particularly V, VII), each cranial nerve has one or two functions that matter more than the others. In the clinical situation cranial nerves are often referred to by number alone (I, II, III, etc.).
You should:
• list the names and numbers of all 12 cranial nerves
• be able to refer to cranial nerves by number only
• list the most important function of each cranial nerve
• describe how to test each cranial nerve (this will not be possible until you have completed your study of the head and neck)
• describe the principal features of the course of each cranial nerve (this will not be possible until you have completed your study of the head and neck).
A brief analysis
• Sensory nerves: I, II, VIII. These are nerves of the special senses.
• Motor nerves: III, IV, VI, XI, XII:
– III, IV and VI innervate muscles that move the eyeball.
– XI innervates sternocleidomastoid and trapezius.
– XII innervates tongue muscle.
• Mixed nerves: V, VII, IX, X. These nerves supply structures derived from embryonic branchial arches at the cranial end of the gut tube.
– Motor fibres are called branchiomotor: they are responsible for movements of the mandible, face, pharynx and larynx.
– Sensory components convey a mixture of cutaneous sensation (e.g. tactile, pain, temperature) and visceral sensation (e.g. taste) from the face, mouth, nose, pharynx and larynx, and in the case of X, visceral sensation from the thorax and abdomen.
• Preganglionic parasympathetic fibres leave the brain stem in III, VII, IX and X but in order to reach their destinations those in III, VII and IX leave these nerves and hitch a lift with branches of V, with the ganglion (synapse) somewhere on the way. Parasympathetic fibres in X pass to the thorax and abdomen (see p. 257 and Fig. 14.14).
• Sensory fibres in cranial nerves:
– Cutaneous and oral sensation (tactile, pain, temperature): most impulses reach the brain stem in V, with a few in X. In the brain stem they pass to the trigeminal sensory nuclei, so called (presumably) because the trigeminal nerve contributes most.
– Visceral sensation (e.g. taste, impulses from chemoreceptors): impulses reach the brain stem in VII, IX and X. In the brain stem the impulses pass to the nucleus of the solitary tract (tractus solitarius) in the medulla (see p. 257 and Fig. 14.15).
Cranial nerves I and II are attached to the cerebral hemispheres, and nerves III to XII to the brain stem (midbrain, pons and medulla). All nerves except IV arise from the ventral aspect.
The olfactory nerve is the nerve of smell. It transmits impulses from the olfactory epithelium of the nose to the brain and is described in more detail in section 14.9 (p. 279).
The oculomotor nerve innervates muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
The trochlear nerve innervates one of the muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
The trigeminal nerve conveys sensation from the face and anterior scalp, the oral and nasal cavities, the teeth and the meninges, and its mandibular division is motor to the eight muscles of the first branchial arch, known as the muscles of mastication.
It arises from the pons and passes forwards to the trigeminal (sensory) ganglion in a slight depression on the petrous temporal bone. It then divides into the ophthalmic (Va), maxillary (Vb) and mandibular (Vc) nerves, each described separately below.
• Shingles. The trigeminal ganglion, like all sensory ganglia, may harbour the herpes zoster virus causing shingles in the sensory distribution of the nerve. The virus may have been latent for years following chickenpox.
• Trigeminal neuralgia. This is severe pain in the distribution of one or more branches of V. Its cause is usually unknown and treatment difficult.
The ophthalmic nerve conveys sensation from the eyeball, the skin of the upper face and anterior scalp, the lining of the upper part of the nasal cavity and sinuses, and the meninges of the anterior cranial fossa.
Some peripheral branches convey parasympathetic fibres from elsewhere on their way to the ciliary and iris muscles, and the lacrimal gland.
From the trigeminal ganglion, Va passes in the lateral wall of the cavernous sinus and divides into the frontal (the largest), nasociliary and lacrimal (the smallest) branches, which pass through the superior orbital fissure into the orbit.
• Frontal nerve: supplies skin of forehead and scalp, and the frontal sinus. The nerve passes directly beneath the frontal bone and divides into supraorbital (larger, lateral) and supratrochlear (smaller, medial) nerves, which turn upwards at the supraorbital margin to the forehead and scalp.
• Nasociliary nerve: supplies the eyeball, upper part of the nasal cavity and neighbouring air cells, anterior nasal skin, and meninges. Its branches include:
– Long and short ciliary nerves conveying sensory fibres from the eyeball. They also convey parasympathetic impulses from III to the ciliary ganglion, and deliver postganglionic impulses to the ciliary body and constrictor pupillae.
– Anterior ethmoidal nerve, which supplies the upper part of the nasal cavity and associated sinuses. At the bridge of the nose it becomes superficial as the external nasal nerve supplying cutaneous sensation down to the nasal tip.
The ophthalmic nerve contains:
• Somatic sensory fibres: to the trigeminal sensory nuclei.
• In peripheral branches only, parasympathetic impulses from the Edinger–Westphal nucleus and III: to the ciliary ganglion (synapse) and eyeball (see p. 257).
• In peripheral branches only, parasympathetic impulses from the superior salivatory nucleus and pterygopalatine ganglion (synapse): to the lacrimal gland (see p. 257).
• Test the cutaneous sensation of the forehead and anterior scalp.
• Corneal reflex. When the cornea is touched, usually with a wisp of cotton wool, the subject blinks. This tests Va and VII. The nerve impulses pass thus: cornea → nasociliary nerve → Va → principal sensory nucleus of V → brain stem interneurons → facial motor nucleus → VII → orbicularis oculi muscle. This reflex does not test II, III, IV or VI.
The maxillary nerve conveys sensation from the malar skin (skin between lower eyelid and mouth), from the nasal cavity and sinuses, and from maxillary teeth. Some of its branches convey postganglionic fibres from the pterygopalatine ganglion to lacrimal, nasal and palatine glands.
From the trigeminal ganglion, Va passes through the foramen rotundum to the pterygopalatine fossa where it divides into:
• Infraorbital nerve: to infraorbital skin, upper lip, maxillary sinus. This passes between orbit and maxillary sinus to emerge at the infraorbital foramen.
• Zygomatic nerve: enters the orbit through the inferior orbital fissure and divides into nerves that penetrate the zygoma to supply overlying skin. It also conveys postganglionic parasympathetic impulses from the pterygopalatine ganglion on their way to the lacrimal nerve and gland.
• Nasal branches: pass to the nasal cavity and sinuses. Branches also convey postganglionic impulses from the pterygopalatine ganglion to nasal glands.
• Greater and lesser palatine nerves: descend in similarly named canals to the palate. Branches also convey postganglionic impulses from the pterygopalatine ganglion to palatal glands.
• Superior alveolar (dental) nerves: pass directly through the maxilla to the maxillary teeth and sinus.
• Pharyngeal branch: passes posteriorly to the nasopharynx.
The nerve contains
• Somatic sensory fibres: to the trigeminal sensory nuclei.
• In peripheral branches only, parasympathetic impulses from the superior salivatory nucleus and VII: to lacrimal, nasal and palatal glands (see p. 235).
Test the cutaneous sensation of the lower eyelid, cheek and upper lip.
The mandibular nerve is a mixed sensory and motor nerve. It conveys sensation from:
• skin over the mandible, side of the cheek and temple
• oral cavity and contents including the anterior tongue
• external ear, tympanic membrane and temporomandibular joint
• meninges of the cranial vault.
It conveys motor fibres to the eight muscles derived from the first branchial arch:
• temporalis, masseter
• medial, lateral pterygoids
• mylohyoid, anterior belly of digastric
• tensor tympani, tensor palati.
As an aid to memory, note the four groups of two: 2 tensors, 2 pterygoids, 2 big chewing muscles, 2 in the floor of the mouth. These are sometimes known as the muscles of mastication, but this is misleading since effective mastication also requires muscles supplied by other nerves: buccinator (VII) and tongue (XII).
Some of the peripheral branches of Vc also convey parasympathetic impulses to the salivary glands, and taste fibres from the anterior portion of the tongue.
• From the trigeminal ganglion, the mandibular nerve passes through the foramen ovale into the infratemporal fossa where it gives:
– branches to the muscles listed above.
• Inferior alveolar nerve: lower teeth, skin, mylohyoid, digastric. The inferior alveolar nerve passes between medial and lateral pterygoids and enters the mandibular foramen. It continues as the mental nerve emerging from the mental foramen of the mandible and supplies skin. Immediately before entering the mandibular foramen it gives the nerve to mylohyoid and anterior belly of digastric.
• Lingual nerve: tongue sensation. The lingual nerve passes between medial and lateral pterygoids and is joined by the chorda tympani, a nerve connecting the lingual nerve with VII. The lingual nerve is immediately below and medial to the third lower molar (wisdom) tooth and passes forwards in the floor of the mouth, crosses medially beneath the submandibular duct and supplies the anterior tongue and gums. Fibres it exchanges with the chorda tympani are taste fibres from the anterior tongue, and parasympathetic fibres to the submandibular ganglion.
• Auriculotemporal nerve: skin of temple, temporomandibular joint, external ear. The auriculotemporal nerve arises immediately beneath the foramen ovale by two rootlets ‘clasping’ the middle meningeal artery. It passes above (or through) the parotid gland, between the temporomandibular joint and the external acoustic meatus, and ascends on the side of the head close to the superficial temporal artery. For a short distance between its origin and the parotid gland it conveys parasympathetic impulses from the inferior salivatory nucleus to the otic ganglion for innervation of the parotid gland.
• Buccal nerve: skin and mucosa of cheek. The buccal nerve passes between the two heads of lateral pterygoid to the cheek. (It does not supply buccinator.)
• Muscular branches: deep temporal nerves to temporalis, and twigs to other muscles.
• Meningeal branches: branches in the infratemporal fossa re-enter the middle cranial fossa through the foramen ovale and other foramina.
The nerve contains
• Sensory fibres: to the trigeminal sensory nuclei.
• Branchiomotor fibres: from the trigeminal motor nucleus (pons).
• In peripheral branches only, taste fibres to the nucleus of the solitary tract: from the anterior portion of tongue via the lingual nerve, chorda tympani, VII.
• In peripheral branches only, parasympathetic impulses:
– from the superior salivatory nucleus and VII to the submandibular and sublingual glands (see p. 257)
– from the inferior salivatory nucleus and IX to the parotid gland (see p. 257).
The mandibular nerve is the main nerve of the first branchial arch, which gives rise to a precursor of the mandible (Meckel’s cartilage), the spine of the sphenoid, the sphenomandibular ligament, the malleus and incus, and the eight muscles listed above. All these structures are related to mandibular nerve function in some way.
• Sensory: test the cutaneous sensation of the chin and lower lip.
• Motor: feel the contractions of masseter and temporalis. Ask your patient to open the jaw against resistance (pterygoids, mylohyoid, anterior digastric).
The abducens nerve innervates one of the muscles that move the eyeball and is described with the orbit and eyeball (section 14.11, p. 290).
The facial nerve supplies the muscles of facial expression.
Its intracranial portion also conveys:
• taste sensation from the anterior portion of the tongue and oral cavity, which is conveyed to the facial nerve by the chorda tympani
• parasympathetic fibres for the first part of their journey to the submandibular, sublingual, lacrimal, nasal and palatine glands.
VII arises from the cerebellopontine angle by two adjacent roots, the motor root (larger, more medial) and the nervus intermedius (smaller, more lateral; sensory and parasympathetic fibres), so named because it is found between two larger nerves (the motor root of VII and VIII).
• The roots of VII enter the internal acoustic meatus (with VIII) and merge.
• The facial canal runs posteriorly along the medial wall of the tympanic (middle ear) cavity, and a branch passes to stapedius (attached to the stapes). The nerve turns downwards and laterally, and just before it emerges from the temporal bone it gives off the chorda tympani, which passes anteriorly across the tympanic membrane to the lingual nerve (Vc) in the infratemporal fossa.
• VII emerges at the stylomastoid foramen.
• Outside the stylomastoid foramen, small branches arise to supply the occipital belly of occipitofrontalis, stylohyoid and the posterior belly of digastric.
• VII enters the parotid gland in which it forms a plexus. Branches of VII are the most superficial structures passing through the gland.
• Five groups (usually) of branches emerge from the anterior border of the gland: temporal, zygomatic, buccal, mandibular and cervical. These supply the muscles of facial expression, including orbicularis oculi, orbicularis oris and buccinator.
The nerve contains:
• Branchiomotor fibres: from the facial motor nucleus.
• In the intracranial portion only, taste fibres to the solitary tract and nucleus: they carry taste sensation from the anterior portion of the tongue in the lingual nerve and gain the intracranial portion of VII through the chorda tympani.
• In the intracranial portion only, preganglionic parasympathetic impulses from the superior salivatory nucleus: to lacrimal, nasal and palatine glands, and to the submandibular and sublingual glands (see p. 257).
• Somatic sensory fibres: to the trigeminal sensory nuclei from a small and variable area of skin near or in the ear.
• The most important thing about the intracranial course of VII is its relationship to the temporal bone and middle ear. It can be affected in ear disease (see p. 285).
• The most important thing about the extracranial course of VII is its relationship to the parotid gland. It can be affected in parotid disease (see p. 266).
• Geniculate herpes. The herpes zoster virus may lie dormant in the geniculate ganglion (after chickenpox) and at a later stage cause a vesicular eruption in the small area of skin around the external acoustic meatus supplied by the facial nerve. There may also be signs on the anterior portion of the tongue because of involvement of taste fibres with cell bodies in the geniculate ganglion. The inflammation may spread to involve the motor fibres in VII, and a lower motor neuron lesion arising thus is known as Ramsay Hunt’s syndrome.
• Observe the face. Normal facial movements (lips, eyelids, emotions) and the presence of normal facial skin creases indicate an intact nerve.
• Test strength by trying to force apart the tightly closed eyelids; this should be difficult.
• Test the corneal reflex; see Va above.
The vestibulocochlear nerve is the nerve of equilibration (vestibular) and hearing (cochlear) and is described in section 14.10 (pp. 287–288).
The main function of the glossopharyngeal nerve is the sensory supply of the oropharynx, posterior third of the tongue, Eustachian tube and middle ear.
Its other functions are:
• motor to stylopharyngeus
• sensory from the middle ear, carotid sinus and carotid body
• conveying parasympathetic fibres part of the way to the parotid gland.
• IX arises from the medulla by rootlets lateral to the olive, above those of X.
• It leaves the posterior cranial fossa through the jugular foramen. Superior and inferior sensory ganglia containing cell bodies of sensory fibres are situated in and near the jugular foramen.
• The tympanic branch is given off in the jugular foramen. This contains parasympathetic impulses from the inferior salivatory nucleus (for the parotid gland) and sensory fibres from the ear.
• IX descends in the neck giving a branch to the carotid body, then enters the pharynx between superior and middle constrictors. Branches contribute sensory fibres to the pharyngeal plexus.
The nerve contains
• Visceral sensory fibres: to the nucleus of the solitary tract.
• Branchiomotor fibres: from the nucleus ambiguus to stylopharyngeus.
• In the proximal part of the nerve only, parasympathetic impulses from the inferior salivatory nucleus: to the parotid gland (see p. 257).
The glossopharyngeal nerve is the nerve of the third branchial arch that gives rise to part of the hyoid bone and the stylopharyngeus muscle. Arterial components of the third arch form part of the common and internal carotid arteries, thus explaining the carotid sinus innervation.
Gag reflex. Sensation supplied by the glossopharyngeal nerve is different in quality to that supplied by the trigeminal. Put your finger on the anterior part of your tongue (Vc) and then on the posterior part (IX) to demonstrate this. The gag reflex is mediated by IX (afferent limb) and X (efferent limb), so it tests both nerves.
The vagus is a mixed motor and sensory nerve supplying the gut tube as far as the transverse colon. This includes the pharynx and larynx for swallowing and phonation, and these are its most important functions.
It also supplies parasympathetic and sensory fibres to the heart, tracheobronchial tree and abdominal viscera, and conveys a few cutaneous sensory fibres from the posterior part of the external acoustic meatus and the tympanic membrane.
The vagus is the most extensively distributed cranial nerve, its name reflecting both the distribution and the type of sensation it conveys (Latin: vagus = vague, indefinite, wandering).
• X arises from the medulla by rootlets lateral to the olive, below those of IX.
• It leaves the posterior cranial fossa through the jugular foramen. Superior and inferior sensory ganglia for cell bodies of sensory fibres are situated in and near the jugular foramen.
• The auricular branch passes through a canal in the temporal bone and conveys sensory fibres from the posterior part of the external acoustic meatus and tympanic membrane.
• X descends in the carotid sheath between the internal jugular vein and the carotid arteries. It gives pharyngeal branches, and the superior laryngeal nerve.
• Cardiac (slowing the heart rate) and tracheal (sensory) branches arise in the root of neck and upper thorax. It enters the thorax and, on the left side, crosses the arch of the aorta.
• Recurrent laryngeal nerves arise in the mediastinum: that on the left is related to the ligamentum arteriosum, that on the right to the subclavian artery. Both recurrent nerves re-ascend between the trachea and oesophagus to supply laryngeal muscles and give sensory fibres to the larynx below the vocal cords, the trachea and the oesophagus.
• The vagus forms the oesophageal plexus and enters the abdomen through the oesophageal hiatus in the diaphragm. See Chapters 10 and 11.
The motor function of the vagus in the neck is branchiomotor: in the thorax and abdomen it is parasympathetic.
• Branchiomotor fibres: from the nucleus ambiguus to pharyngeal and laryngeal muscles.
• Parasympathetic fibres: from the dorsal motor nucleus of vagus to the heart and thoracoabdominal viscera (foregut and midgut, see p. 257).
• Somatic sensory fibres: to the trigeminal sensory nuclei. From the posterior wall of the external acoustic meatus and the posterior portion of the external surface of the tympanic membrane, fibres pass in the auricular branch of X to the main trunk in the jugular foramen.
• Visceral sensory fibres: to the nucleus of the solitary tract from taste buds in the epiglottic area, visceral sensory fibres from gut tube derivatives and aortic baro- and chemoreceptors.
The vagus is the nerve of the fourth and sixth branchial arches. Structures derived from these include the pharyngeal and laryngeal cartilages and muscles. The sixth arch artery on the left gives rise to the ductus arteriosus (ligamentum after birth) around which the left sixth arch nerve, the recurrent laryngeal, is trapped in embryonic life. The sixth arch artery on the right degenerates, so the right recurrent laryngeal nerve is related to the most caudal persisting branchial arch artery, the fourth, which becomes the right subclavian.
The vagus controls the entry into the gut tube (swallowing), and mediates sensation of most of the gut tube. This includes the bronchial tree, another gut tube derivative. The heart develops from cells initially found in the wall of the yolk sac, from which the gut tube develops. Sustenance is a common theme here, whether the absorption of nutrients from the yolk sac (gut tube) or their propulsion round the body by the force of cardiac contractions. Perhaps the ‘big picture’ is that the vagus is the nerve of sustenance – the yolk sac nerve.
• If speech is normal, there is no need to test X at all since it supplies the muscles that move the vocal cords causing phonation.
• Say ‘aah’. Observing the elevation of the palate when a subject says ‘aah’ tests motor function in fibres from the nucleus ambiguus in X.
• Gag reflex – see IX above.
The accessory nerve has two parts: cranial and spinal. Oddly enough, when clinicians refer to the eleventh cranial nerve, or accessory nerve, they mean the spinal accessory.
• Cranial accessory. This arises from a caudal extension of the nucleus ambiguus by rootlets below and in series with those of IX and X. It joins X, from which it is functionally indistinguishable (its name means accessory vagus). This book considers the cranial accessory no more and neither need you.
• Spinal accessory: this is the one to remember (Fig. 14.9). This is motor to the muscles bounding the posterior triangle of the neck: sternocleidomastoid and trapezius.
• Rootlets from the upper four or five segments of the spinal cord (in series with those of IX, X and cranial XI) emerge between the ventral and dorsal spinal nerve roots.
• The spinal accessory ascends through the foramen magnum to enter the posterior cranial fossa and briefly runs with cranial XI before it (the cranial) joins the vagus.
• XI descends through the jugular foramen into the neck and passes deep to sternocleidomastoid, which it supplies.
• XI enters the posterior triangle of the neck about one-third of the way down the posterior border of sternocleidomastoid and passes across to enter trapezius about one-third of the way up its anterior border.
The nerve contains
• Motor fibres: cell bodies are in the lateral part of the ventral grey horn of cervical cord segments 1–5.
• Ask your patient to move his chin up to one side against resistance (contralateral sternocleidomastoid).
• Ask your patient to shrug his shoulders (trapezius) against resistance.
• Ask your patient to put his hand on his head (trapezius: shoulder abduction beyond 90°).
The hypoglossal nerve supplies the muscles of the tongue. Movements of the tongue are important in chewing, in the initial stages of swallowing, and in speech.
It also conveys fibres from C1 which contribute to the innervation of the strap muscles.
• It passes through the hypoglossal (condylar) canal in the occipital bone.
• It receives motor fibres from C1 and descends to the submandibular region.
• It turns forwards, lateral to the external carotid artery and hooks beneath the origin of the occipital artery.
• It gives a branch to the ansa cervicalis, which carries some fibres from C1 to the strap muscles; other C1 fibres remain with XII to supply geniohyoid.
• It enters the tongue from below passing lateral to hyoglossus and supplies the muscles of the tongue.
The nerve contains:
• Motor fibres: from the hypoglossal nucleus in the floor of the fourth ventricle in the medulla, to the tongue muscles.
• Ask your patient to protrude the tongue. If it deviates to one side, then the nerve of that side is damaged – the tongue is pushed to the paralysed side by muscles of the functioning side.
• Ask the patient to push the tongue into the cheek, then palpate the cheek to feel tone and strength of tongue muscles.
Parasympathetic and taste components in cranial nerves, although one is efferent and the other afferent, share some peripheral pathways connecting branches of one cranial nerve to another (e.g. chorda tympani, petrosal nerves). These pathways provide material for nit-picking examinations, and are of embryological interest, but from a functional point of view they are insignificant. They may have to be interrupted, for example in ear surgery, and although food and drink may lose some savour, and the patient may subsequently suffer from a dry mouth, this could never be described as life-threatening.
• Edinger–Westphal nucleus–III–ciliary ganglion (synapse)–branches of Va–iris, ciliary body.
• Superior salivatory nucleus–VII–greater petrosal nerve–pterygopalatine ganglion (synapse)–branches of Vb–lacrimal, nasal, palatine glands.
• Superior salivatory nucleus–VII–chorda tympani–submandibular ganglion (synapse)–branches of Vc–submandibular, sublingual glands.
• Inferior salivatory nucleus–IX–lesser petrosal nerve–otic ganglion (synapse)–branches of Vc–parotid gland.
• Dorsal motor nucleus of the vagus–X–gut tube derivatives and heart (synapses in or near destination).
• Taste sensation from palate–branches of Vb–greater petrosal nerve–VII (cell bodies in geniculate ganglion)–solitary tract of brain stem.
• Taste sensation from anterior tongue and mouth–branches of Vc–chorda tympani–VII (cell bodies in geniculate ganglion)–solitary tract of brain stem.
• Taste sensation from posterior tongue–IX (cell bodies in sensory ganglia of IX)–solitary tract of brain stem.
• Taste sensation from pharynx–X (cell bodies in sensory ganglia of X)–solitary tract of brain stem.
• Pupillary light reflex: this tests parasympathetic fibres from the Edinger–Westphal nucleus (see section 14.11, pp. 294, 295).
• Salivary glands. Ask your patient to suck something bitter (e.g. a lemon) to provoke salivary secretion. This is more usually done to try to locate the position of a calculus in the duct of a salivary gland, usually the submandibular.
• Taste. Testing taste is possible but hardly worth the trouble.
Fascial sheets surround various structures in the neck and are important in the spread of disease. Bones and cartilages in the anterior neck form the visceral skeleton of the larynx. Arteries and veins travel anterior to, or through the vertebral column. The neck is divided into posterior and anterior triangles.
• The investing layer of cervical fascia encloses the deep structures like a sleeve. It is attached posteriorly to the nuchal ligament and splits around trapezius and sternocleidomastoid. Cutaneous nerves are superficial to it.
• The carotid sheath is a vertical fascial tube deep to the investing layer of fascia. It contains the common and internal carotid arteries, the internal jugular vein, the vagus nerve and the deep cervical chain of lymph nodes.
• The prevertebral ‘space’ is the area between the prevertebral muscles and the pharynx/oesophagus containing loose connective tissue and lymph nodes. It allows disease to spread from one side of the neck to the other. The cervical sympathetic chain is found here, immediately posterior to the carotid sheath.
• The pretracheal fascia in front of and to the sides of the trachea encloses the thyroid gland and with the investing layer of cervical fascia anteriorly forms sheaths around the strap (infrahyoid) muscles of the neck.
• Platysma muscle is directly subcutaneous. When it contracts it raises ridges in the skin of the neck and is useless except for those who shave. It is supplied by VII and is a now-redundant muscle of ‘facial’ expression.
• Hyoid bone. This is palpable immediately underneath, almost inside, the mandible at the top of the neck. The greater horns (cornua) extend backwards from the sides of the body (be careful when palpating these – too much pressure will fracture the bone).
• Thyroid cartilage. Right and left laminae join in the midline to form the thyroid prominence or Adam’s apple. Superior horns extend up towards the hyoid bone, and inferior horns articulate with the cricoid cartilage below.
• Cricoid cartilage. This is a cartilaginous ring at the top of the trachea. It has a lamina posteriorly and facets for synovial joints with the inferior horns of the thyroid cartilage at the sides.
• Membranes attach these cartilages to each other so that they move as one.
– thyrohyoid membrane, palpable between hyoid bone and thyroid cartilage
– cricothyroid membrane, palpable between thyroid and cricoid cartilages. Laryngotomy is performed here.
Despite movement during swallowing, these vertebral levels are worth remembering:
• hyoid bone: about C2
• thyroid cartilage, upper margin of lamina (surface marking of bifurcation of common carotid artery): about C3
• vocal cords: about C4
• thyroid cartilage, lower margin of lamina: about C5
• cricoid cartilage (surface marking of beginning of trachea and oesophagus): C6.
This has no branches in the neck, but enters the skull through the carotid canal. It is called internal because it passes into the cranium, not because of its position in the neck.
This gives branches as follows:
• Superior thyroid: to thyroid gland, larynx, pharynx. This may arise from the bifurcation or even from the common carotid artery.
• Ascending pharyngeal (not important).
• Lingual: to the tongue.
• Facial: to the face. The lingual and facial may arise by a common trunk.
• Occipital: to the back of the head. The occipital comes off the posterior border at about the same level as the lingual and facial arise anteriorly, and at its origin is intimately related to XII.
• Posterior auricular: to the region around the ear.
• The two terminal branches, arising behind the neck of the mandible, are:
– superficial temporal: to the side of the head and scalp, usually visible and palpable
– maxillary: to the mandible, maxilla, cheek, nasal cavity, skull bones and cranial meninges.
Press posteriorly lateral to the upper border of the thyroid cartilage. You are compressing the common carotid artery against the anterior aspect of the transverse process of vertebra C3. Do not push too hard, and do not palpate both sides together.
Place your fingers about 2 cm above the middle of a line joining the top of the pinna to the side of the orbit.
This is a branch of the first part of the subclavian artery. It ascends through the foramina transversaria of vertebra C6 (usually) to C1, then turns medially, grooving the upper surface of the atlas behind the atlanto-occipital joint facet, pierces the meninges and enters the subarachnoid space. It passes through the foramen magnum, ascends on the anterior aspect of the brain stem and unites with its opposite number to form the basilar artery.
• Branches in the neck supply deep neck structures and give twigs through intervertebral foramina to the spinal cord.
• Branches in the cranium supply the spinal cord, brain stem, vital centres, vestibular apparatus and the posterior cerebral cortex.
This emerges from the jugular foramen of the skull and descends in the carotid sheath with the common carotid artery and X. It terminates behind the sternoclavicular joint where it joins the subclavian to form the brachiocephalic vein. It receives tributaries from the face and thyroid gland.
This is formed behind the angle of the mandible from superficial veins of the face and passes obliquely towards the midpoint of the clavicle. It receives tributaries from superficial neck tissues and terminates by joining the subclavian vein either directly or indirectly.
These are situated near the medial (anterior) border of sternocleidomastoid and form a venous arch that drains to the brachiocephalic veins.
Get Clinical Tree app for offline access
• Internal jugular: ear lobe (roughly)–sternoclavicular joint. It is deep to sternocleidomastoid, so is neither visible nor palpable.
• External jugular: angle of mandible to midpoint of clavicle. This is superficial and is visible throughout its length.