HAND SURGERY: INTRODUCTION
INTRODUCTION
The prime functions of the hand are feeling (sensibility) and grasping. Sensibility is most important on the radial sides of the index, middle, and ring fingers and on the opposing ulnar side of the thumb, where one must feel and be able to pinch, pick up, and hold objects. The skin on the ulnar side of the small finger and its metacarpal, upon which the hand usually rests, must register the sensations of contact and pain to avoid burns and other trauma.
Mobility is critical for grasping. The upper extremity is a cantilevered system extending from the shoulder to the fingertips. It must be adaptable to varying rates and kinds of movements. Stability of proximal joints is essential for good skeletal control distally.
The specialization of the thumb has allowed humans to have superior aptitudes for defense, work, and dexterity. The thumb has exquisite sensibility and is a highly mobile structure with well-developed adductor and thenar (pronating) musculature. It is the most important digit of the hand, and every effort must be made to preserve its function.
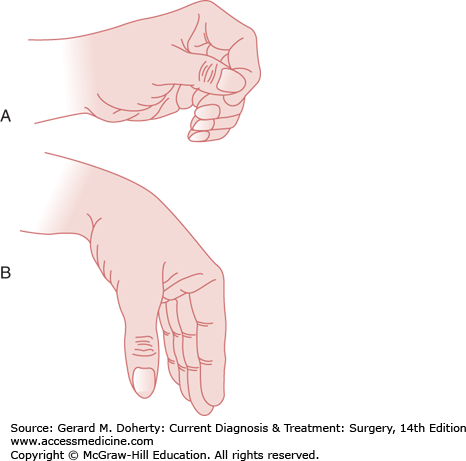
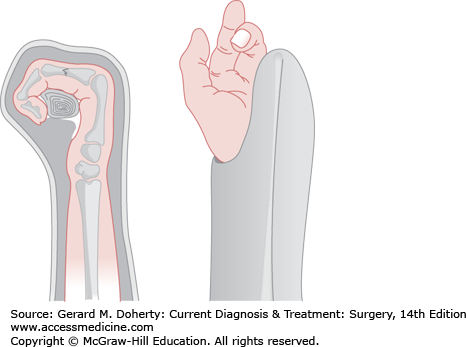
The position of function of the upper extremity favors reaching the mouth and perineum and achieves a comfortable, forceful, and unfatiguing grip and pinch. The elbow is held at or near a right angle, the forearm neutral between pronation and supination, and the wrist extended 30 degrees with the fingers flexed to almost meet the opposed (pronated) tip of the thumb (Figure 42–1A). This is the desired position of the extremity if stiffness is likely to occur, and it should be maintained when joints are immobilized by splinting, arthrodesis, or tenodesis.
Opposite to the position of function is the position of rest, in which the flexed wrist extends the digits, making grip and pinch awkward, uncomfortable, weak, and fatiguing (Figure 42–1B). The forearm is usually pronated, and the elbow may be extended. This habitus is assumed, without intention, after injury, paralysis, or the onset of a painful stimulus. For that reason, it is also called the position of the injury. Immobility in this position jeopardizes function.
ANATOMY
All references to the forearm and hand should be made to the radial and ulnar sides (not lateral and medial) and to the volar (or palmar) and dorsal surfaces. The digits are identified as the thumb, index finger, middle finger, ring finger, and small finger.
The skin is an elastic outer sleeve and glove of the arm and hand. Sacrifice of its surface area or elasticity by debridement and fibrosis can severely diminish the range of motion and constrict circulation. In the adult hand, the dorsal skin stretches about 4 cm in the longitudinal and in the transverse planes when the palm is flattened and spread. The long finger can have as much as 48 cm2 of skin cover, and the whole hand (exclusive of digits) has 210 cm2.
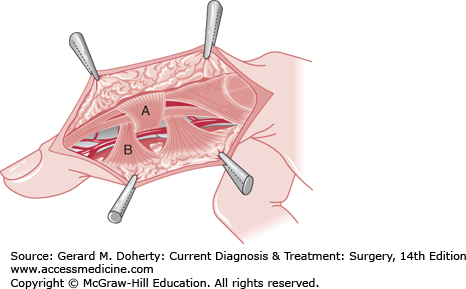
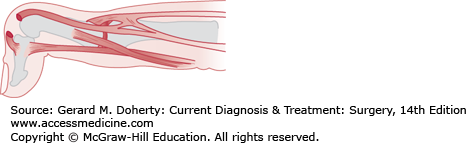
Fascia anchors the palmar skin to bone to make pinch and grip stable; the midlateral fibers of the Cleland and Grayson ligaments keep the skin sleeve from twisting around the digit (Figure 42–2). In the form of sheaths and pulleys, fascia holds tendons in the concavity of arched joints to convey mechanical efficiency and power. The fascial sleeve of the forearm, hand, and digits must sometimes be released along with skin to prevent or relieve congestion (eg, compartment syndrome). Any fascial compartment of the hand provides a space for infection or an avenue for its dissemination.
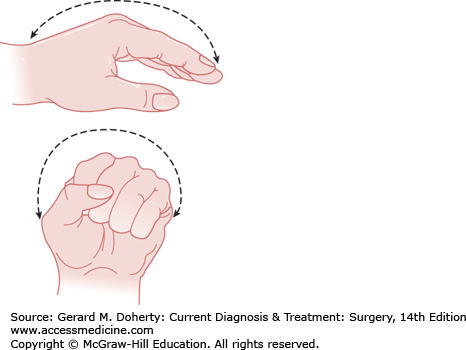
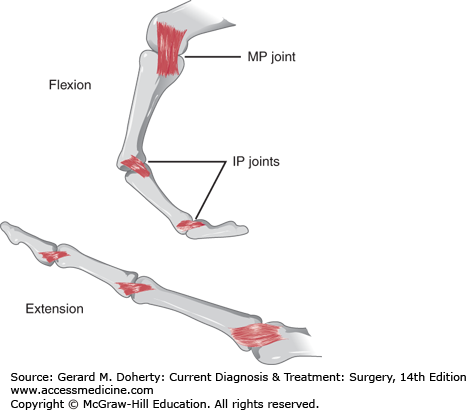
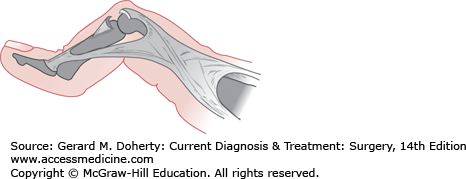
Each finger has three joints, the distal interphalangeal joint (DIP), the proximal interphalangeal joint (PIP), and the metacarpophalangeal joint (MCP). The thumb contains the IP, the MCP, and the carpometacarpal joint (CMC). The wrist is the “key joint” of the hand, governing motion of the digits, and may need to be included in the immobilization required for a major finger or hand problem. The position of the wrist governs the efficiency of extrinsic muscle contraction. The wrist is composed of a proximal and distal row of carpal bones. The proximal row contains the scaphoid, lunate, triquetrum, and pisiform, while the distal row contains the trapezium, trapezoid, capitate, and hamate. The stability of the digital joints and their planes of motion are governed by the length of the ligaments and the anatomy of their articulating surfaces. The longitudinal and transverse arches of the hand (Figure 42–3) are architectural prerequisites to gripping, pinching, and cupping, and are maintained by the active contraction and passive tone of intact muscles. The arches create the position of function. When the arches are collapsed, the hand assumes the position of injury. Loss of these arches is most often initiated by edema. They may be preserved by splinting in the position of function, elevation without constriction, and early restoration of active joint motion.
Each MCP and PIP joint has a distally anchored volar plate (Figure 42–4) in addition to collateral ligaments stabilizing the joint on either side (Figure 42–5). The thickened lateral portions of the volar plate form the checkrein ligaments, which prevent IP hyperextension.
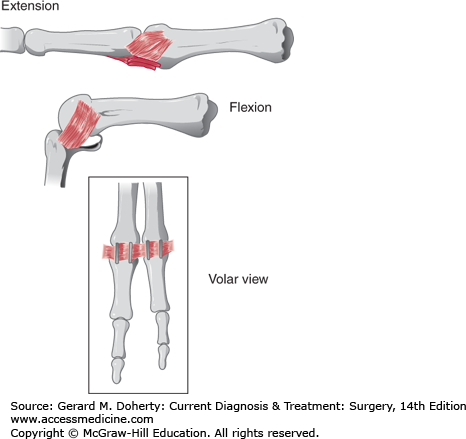
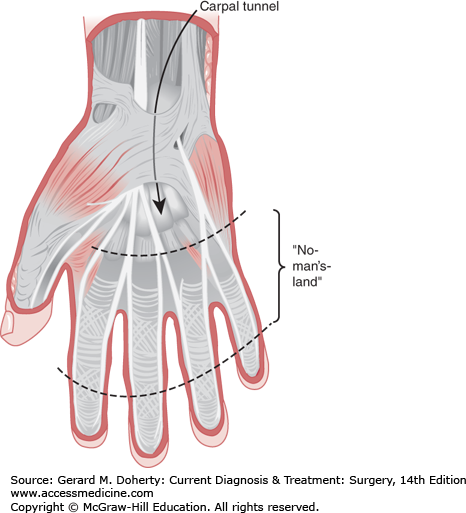
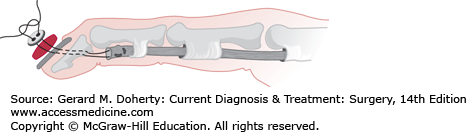
The extrinsic flexor tendons are contained in fibrous sheaths to prevent bowstringing and preserve mechanical efficiency as the digits flex into the palm. Pulleys (hypertrophied sections of the sheath) resist the points of greatest tendency to bowstring. The retinacular pulley system contains five annular bands and three cruciform bands. Sheaths are inelastic and relatively avascular. Therefore, they crowd and congest any swollen, inflamed, or injured tendons and curtail glide by friction, constriction, and the generation of inelastic adhesions. The A-2 and A-4 pulleys must be maintained to prevent tendon bowstringing. These are located over the proximal and middle phalanges, respectively. The A-1, A-3, and A-5 pulleys are located over the MCP, PIP, and DIP joints, respectively. Five flexor tendon zones have been described. Zone II, or “no man’s land,” is the zone from the middle of the palm to just beyond the PIP joint, wherein the superficialis and profundus tendons lay ensheathed together and where recovery of glide is difficult after wounding (Figure 42–6).
Across the wrist, the dense volar transverse carpal ligament closes the bony carpal canal (carpal tunnel) through which passes all eight finger flexors as well as the flexor pollicis longus and median nerve (Figure 42–6). The ulnar bursa is the continuation of the synovium around the long flexors of the small finger through the carpal tunnel, encompassing the other finger flexors which interrupted their separated bursa at the midpalm level. The radial bursa is the synovium around the flexor pollicis longus contained through the carpal tunnel. These two bursas may intercommunicate. Parona space is the tissue plane over the pronator quadratus in the distal forearm deep to the radial and ulnar bursas.
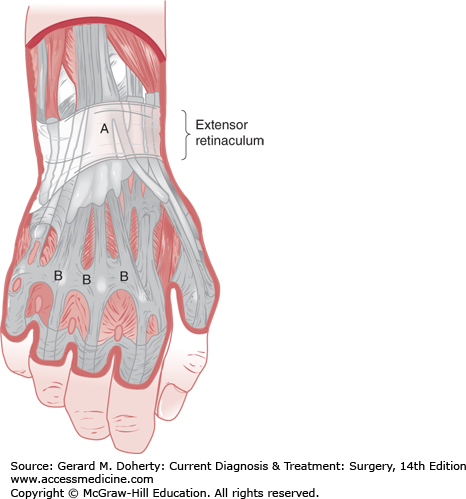
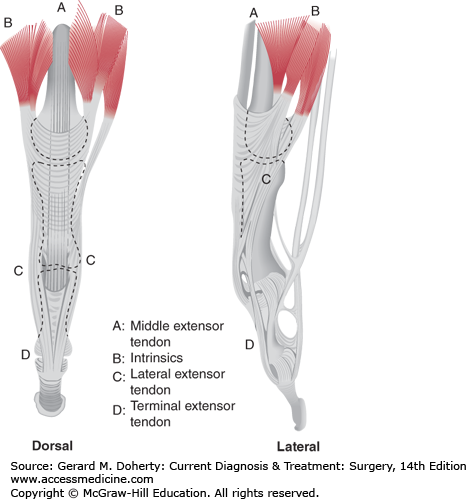
The extensor tendons are ensheathed in six individual compartments at the wrist beneath the extensor retinaculum (Figures 42–7 and 42–8), which predisposes to adhesions. Its role as a pulley is not as vital.
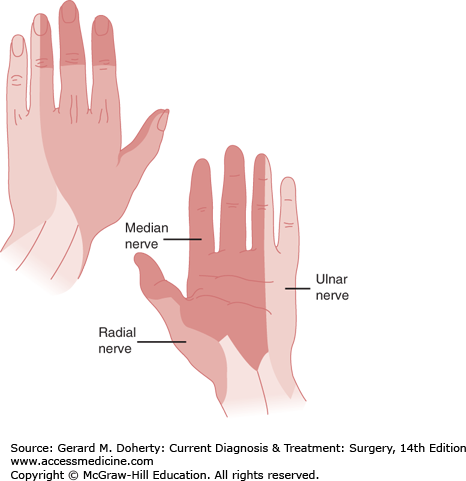
The nerves of greatest importance to hand function are the musculocutaneous, radial, ulnar, and median nerves. The importance of the musculocutaneous and radial nerves combined is forearm supination and of the radial nerve alone is innervation of the extensor muscles. The ulnar nerve innervates 15 of the 20 intrinsic muscles. The median nerve provides sensation to the thumb, index finger, middle finger, and the radial aspect of the ring finger; through its motor innervation, it maintains most of the long flexors, the pronators of the forearm, and the thenar muscles. Figure 42–9 shows the sensory distribution of the ulnar, radial, and median nerves.
CLINICAL EVALUATION OF HAND DISORDERS
The presenting complaint must be assessed in complete detail with regard to its mechanisms of onset, evolution, aggravating factors, and relieving factors. Age, sex, hand dominance, occupation, preexisting hand problems, and relevant matters pertaining to the patient’s general health must also be noted.
The examination should follow an orderly routine. Observe the neck, shoulders, both upper extremities, and the action and strength of all muscle groups, and be certain that all parts can pass painlessly and coordinately through a normal range of motion, starting with the head and neck and working down to the fingertips. Compare both upper extremities and keep detailed notes, diagrams, and measurements. Having the patient reach for the ceiling and simultaneously open and close both fists and then spread and adduct the fingers and, finally, oppose the thumbs sequentially to each fingertip will immediately demonstrate any abnormalities.
Observe habitus, wasting, hypertrophy, deformities, skin changes, skin temperature, scars, and signs of pain (including when the patient attempts to bear weight on the palms). Feel the wrist pulses and the sweat of the finger pads, and test reflexes and the sensibility of the median, ulnar, and radial nerves.
Serial x-rays and laboratory studies may clarify a problem with an indolent evolution (eg, Kienböck avascular necrosis of the lunate, causing unexplained wrist pain). Contralateral and multiple-view x-rays in different planes are often helpful. In addition, computed tomography (CT) scans, magnetic resonance imaging (MRI), bone scans, or all of these may aid in diagnosis. This is especially true in patients who have persistent bone and joint pain or limited motion or in patients who have not attained adult growth. In the case of wrist problems, arthrograms and arthroscopy may be of diagnostic value. MRI can be quite helpful in the diagnosis of subtle carpal bone problems.
The diagnosis is often made by noting the response to therapy. This is particularly true in the case of local corticosteroids injected at the site of noninfectious inflammatory conditions (eg, carpal tunnel syndrome, trigger finger).
GENERAL OPERATIVE PRINCIPLES
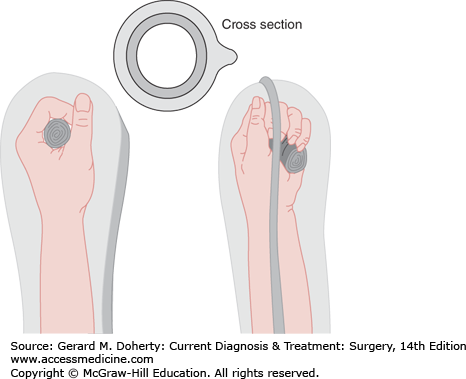
A bloodless field (eg, by tourniquet ischemia) is essential for accurate evaluation, dissection, and management of tissues of the hand. This is achieved by elevating or exsanguinating the extremity and then inflating a padded blood pressure cuff around the arm to 100 mm Hg above systolic pressure. This is readily tolerated by the unanesthetized arm for 30 minutes and by the anesthetized arm for 2 hours.
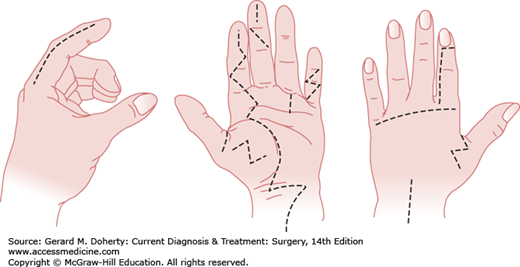
Incisions (Figure 42–10) must be either zigzagged across lines of tension (eg, must never cross perpendicularly to a flexion crease), termed Brunner incisions, or run longitudinally in “neutral” zones (eg, connecting the lateral limits of the flexion and extension creases of the digits), and whenever possible, must be designed so that a healthy skin-fat flap is raised over the zone of repair of a tendon, nerve, or artery.
Proper evaluation and treatment of an acute injury often requires extension of the wound. Normal structures can then be identified and traced into the zone of injury, where blood and devitalized tissue can make their identification difficult or impossible.
Constriction and tension by dressings must be avoided. The dressing should be applied evenly to the skin without wrinkles. The wound should be covered with a single layer of fine-mesh gauze followed by a moist spongy medium (fluffs, Rest-On, Kling, or Kerlix). Moisture facilitates the drainage of blood into the dressing, which should be applied with gentle pressure to restrict dead space.
Splinting and immediate elevation are paramount in controlling swelling and pain postoperatively. In general, plaster (fast-setting) or fiberglass is preferred because of its adaptability to specific requirements. More often than not, the wrist requires immobilization along with any other part of the hand (Figures 42–11 and 42–12).
It must be appreciated that effective immobilization of a finger most often requires concomitant immobilization of one or more adjacent fingers, usually in the position of function. Straight splints such as tongue blades involve a hazard of digital stiffness and distortion and should not be used across the MCP joint.
Persistence of pain signifies inadequate immobilization and, if throbbing is present, congestion. Congestion must be promptly relieved by elevation and sectioning of the cast and dressing and, if necessary, the skin and fascia.
CONGENITAL ANOMALIES OF THE HAND
Major congenital hand anomalies are not rare, with approximately 1 in 700 live births affected. When minor deformities are included, approximately 3% of all births are affected. Camptodactyly (bent finger), polydactyly (more than five fingers), and syndactyly (two or more fingers are joined together) are the most common malformations. Newborns with hand anomalies should be carefully examined for other malformations because multisystem syndromes can be present in 5% of patients (eg, vertebral, anal atresia, cardiac, trachea, esophageal, renal, and limb [VACTERL] syndrome with radial head dysphasia).
Anomalies may be inherited, caused by environmental factors (drugs, viral infections, irradiation, alcohol), or idiopathic. Major genetic or major environmental causes are infrequently found, suggesting that the cause of most defects is multifactorial.
In order to simplify an extremely complex clinical problem, the American Society for Surgery of the Hand (ASSH) and all major international hand societies have adopted a single classification system that divides anomalies into six main categories: failures of formation (absent digits, phocomelia [seal limb]), failures of differentiation (syndactyly), duplication (polydactyly), undergrowth (brachydactyly), overgrowth (macrodactyly), and constriction ring syndrome (focal necrosis, intrauterine amputation). There is considerable overlap in the categories, as might be expected.
Ideally, surgery is performed early in the first 2 years of life, but timing is individually tailored to the problem.
TENDON DISORDERS OF THE HAND
Movement of the muscles of the hand and arm are transmitted into finger and wrist motion by the tendons. The tendons are strong, compact units that glide within their individual compartments. Disruption of the tendon by trauma or loss of tendon gliding by inflammation hinders tendon excursion and therefore limits active motion of the joints. Passive motion of the joint is still possible with an isolated tendon problem and distinguishes tendon disorders from joint disorders when both active and passive motions are limited.
Tendon disruption can result from any penetrating injury and can be diagnosed by physical examination. A tendon injury should be suspected when the patient is unable to actively move a joint. Certain tendon lacerations, such as an isolated flexor digitorum superficialis disruption, may be masked because the profunda tendon can still move the entire finger. Blocking of profunda function by blocking flexion in the neighboring fingers (the profunda tendons are joined in the palm) reveals the injury to the superficialis when the injured PIP joint cannot be flexed.
The state of the wound and the complexity of the injury are the principal issues the hand surgeon must weigh in choosing between a primary or secondary tenorrhaphy. Clean wounds generally favor primary tenorrhaphy. Primary tenorrhaphy is defined as one that is done within 24-72 hours after injury. When wounds are unstable, contaminated, or complicated by fracture or ischemia, formal tenorrhaphy may have to be delayed for weeks or months until the tendon bed is more favorable to healing and glide. However, interim tacking of the tendons—together, to tendon sheaths, or to bone—to maintain the fiber length of a muscle may be done as a preliminary procedure.
Preoperative treatment of fresh lacerations consists of wound closure, immobilization, and prophylactic antibiotics. Such cases can be deferred for definitive primary repair for 24 hours or more. The timing of delayed secondary procedures depends on the resolution of wound edema and fibrous callus (ie, how soft and pliable it is). After 6-8 weeks, tendons that retract over 2.5 cm may defy full excursion because muscle elasticity has been lost or because the tendon is recoiled and congealed in scar.
Tenorrhaphy must be done without surface trauma along the tendon or its bed. The repair is made end to end or by weaving one tendon with the other, using a 3-0 or 4-0 braided synthetic polyester material, Prolene or nylon sutures. A flexor tendon graft is anchored distally to bone (Figure 42–13). Tenodesis will occur if the surface of the tendon and the surface where adherence is desired are roughened. The position of immobilization should relieve tension on the tendon juncture. The duration of immobilization after tenorrhaphy is generally no more than 3-4 weeks. Controlled early, passive or active mobilization after tenorrhaphy may be initiated as early as 1 week to minimize excessive tendon scarring. This requires a very cooperative patient and close supervision by the hand therapist to avoid rupture of the repaired tendon.
Adhesions invariably form wherever tendons are even slightly inflamed or injured and can severely limit tendon function. Even so, adhesions are necessary for a tendon to reestablish continuity. With continuous active and passive movement over months, tendon glide can be increased with maturation and molding of the collagen in the adhesions. If the adhesions remain thick and tendon excursion is limited, surgical release of the tendon adhesions (tenolysis) needs to be performed. Successful surgery requires the release of all adhesions limiting tendon glide without rupturing the tendon repair. Movement of the tendon as soon as possible after surgery (within 24-48 hours) under the guidance of the hand therapist is critical to avoid recurrence of adhesions.
The access to tenolysis should be through an incision offering effective exposure and placed where the immediate active and passive joint motion that must follow will not jeopardize healing of the wound by undue stretching or direct pressure. Performing a concomitant procedure requiring immobilization such as a neurorrhaphy should be avoided. The patient must understand that joint mobilization after tendon surgery is a time-consuming process, often taking many weeks or months to achieve maximum recovery.
Mallet finger (“baseball” or “drop” finger) (Figure 42–14) is due to disruption of the extensor tendon to the distal phalanx. A distal joint that can be passively but not actively extended is diagnostic. The injury most commonly results from sudden forceful flexion of the digit when it is held in rigid extension. Either the extensor is partially or completely ruptured or the dorsal lip of the bone is avulsed. Less frequently, the injury is due to direct trauma such as a laceration. An x-ray should be taken to determine the presence and extent of any fracture.
Treatment requires 6-8 weeks of continuous splinting in full distal joint extension (not hyperextension) with or without 40 degrees of PIP joint flexion. Patient education and compliance are essential for good results. Joint fixation internally with a percutaneous Kirschner wire or externally with padded aluminum, plastic, or plaster splints are equally effective. A lacerated tendon should be repaired. When a significantly displaced fracture fragment represents one-third or more of the surface of the joint, it should be reduced by wiring or pinning. If there is sufficient articular surface disruption, one may consider joint fusion.
Swan-neck deformity (Figure 42–14) is a frequent complication of mallet finger, but it may also be the result of disparity of pull between the extrinsic flexors and extensor hood with or without attenuation of the DIP joint extensor. It is seen in congenitally hypermobile joints, spastic, and rheumatoid states, and following resection of the superficialis tendon. The dorsal hood acts to extend the distal joint but is held back by its insertion at the base of the middle phalanx, which it therefore hyperextends. This in turn increases the tension on the profundus, which hyperflexes the DIP joint. If the mallet deformity is 25 degrees or less and there is some active distal joint extension, it may be treated by undermining and elevating the extensor hood at the PIP joint and severing its insertion on the base of the middle phalanx. Otherwise, the deformity may be corrected by tethering PIP joint extension with one slip of the flexor digitorum superficialis threaded through the flexor pulley of the proximal phalanx with the PIP joint flexed 20 degrees.
The boutonnière, or “buttonhole,” deformity (Figure 42–15) appears as the opposite of the swan-neck deformity: hyperextension of the DIP joint and flexion of the PIP joint. There is attenuation or separation of the dorsal hood, so that the middle extensor tendon becomes ineffective and the lateral extensor tendons shift volar to the PIP joint axis and the joint buckles dorsally. The entire extrinsic-intrinsic force on the hood passes onto the lateral extensor tendons, which flex the PIP joint and hyperextend the DIP joint. This deformity may develop suddenly or, more often, insidiously after closed blunt or open trauma over the dorsum of the PIP joint.
To avoid this complication, sutured extensor tendon lacerations and severe contusions over the PIP joint should always have the PIP joint alone splinted in extension for 3-4 weeks. Established deformities can be treated by such immobilization but more often require operative correction.
In stenosing tenosynovitis, there is a disproportion between the clearance inside a tendon pulley or tunnel and the diameter of the tendon or tendons that must glide through it. Any pulley or tunnel may be implicated. The more common sites are as follows:
The proximal digital (A1) pulleys in the distal palm, causing trigger finger or thumb. There is local tenderness of the pulley; pain, which may be referred to the PIP joint; and (usually but not always) locking of the digit in flexion with a painful “pop” as it goes into extension (ie, as the bulge in the tendon or tendons passes through the tight pulley).
The pulley over the radial styloid housing the abductor pollicis longus and extensor pollicis brevis (first extensor compartment), causing de Quervain tenosynovitis. Local tenderness and pain occur if these tendons are actively stretched (eg, Finkelstein test). The Finkelstein test is performed by having the patient bend the thumb into the palm and grasp with the fingers. The wrist is then bent ulnarly, and the first extensor compartment palpated. Pain in this area suggests de Quervain tenosynovitis.
Relief of the symptoms can be achieved by local injections of triamcinolone mixed with lidocaine. Immediate surgery is justified if the constriction is so tight that the tendon is locked. Surgical section of the constricting tendon sheath is also indicated if symptoms persist or recur. When releasing the flexor tendon, care is taken not to resect more than the section of sheath restricting the tendon or else the tendon will pull away from the finger like a bowstring and weaken the grip.
SKELETAL INJURIES OF THE HAND
Injuries to the bones and joints of the hand are the most common skeletal injuries treated by physicians. Recognition of the injury, appropriate diagnostic tests, and timely treatment are essential for minimizing the complications of these injuries. Some patients may neglect obvious fractures and dislocations in hope of spontaneous recovery. More subtle injuries to the wrist are more often neglected by the patient and sometimes even missed by physicians until further damage is done. The use of the fluoroscope, found in many offices, greatly enhances the surgeon’s ability to diagnose fractures. The machine allows real-time assessment of the bones as part of the physical examination. A common late sequela of skeletal injury at the articular surfaces is osteoarthritis, which is difficult to treat. Patients with symptoms related to the hand or wrist but without a discernible cause should be referred early to a hand specialist.
Fractures of the metacarpal and phalangeal bones such as distal phalanx tuft of the fingers caught in closing doors and metacarpal shaft fractures of the ulnar side of the hand (boxer’s fractures) create an obvious deformity and are easy to diagnose. Adequate x-rays of the specific site of the fracture with anteroposterior, lateral, and oblique views are essential for developing a treatment plan.
Fractures of the shaft can usually be treated with closed reduction and a cast or splint holding the hand in the position of function (Figure 42–1) for 3-4 weeks. Residual angulation of a metacarpal shaft fracture of up to 30 degrees in the fifth finger and 20 degrees in the fourth finger is functionally well tolerated, although a dorsal bump may be aesthetically unpleasant. However, even a small rotational misalignment of the fracture at the metacarpal bone results in scissoring of the fingers in flexion and causes severe dysfunction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree