Giant Cell Tumor of Tendon Sheath
David R. Lucas, MD
Key Facts
Terminology
Localized tenosynovial giant cell tumor, localized PVNS, nodular tenosynovitis
Etiology/Pathogenesis
Balanced translocation involving 1p13 (CSF1 gene) in many tumors
Arises from tendon sheath, intraarticular site, or bursa
Clinical Issues
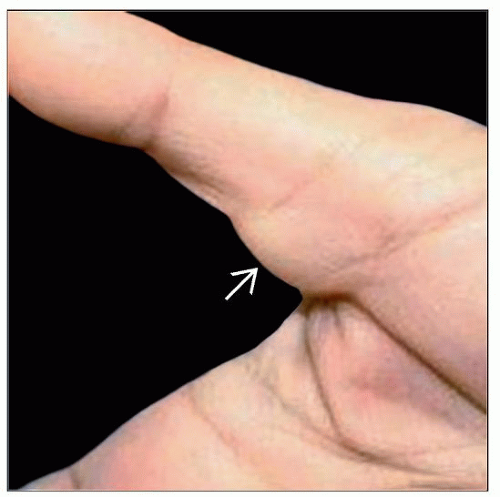
2nd most common tumor of hand
Any age; peak 3rd-4th decade
Digits (85%)
Large joints (10%)
Intraarticular tumors called localized PVNS
Benign but recurs locally (around 20%)
Rarely involves overlying skin
Macroscopic Features
Average size: 1.1 cm (range: 0.5-6 cm)
Well demarcated
Multinodular with fibrous septa
Microscopic Pathology
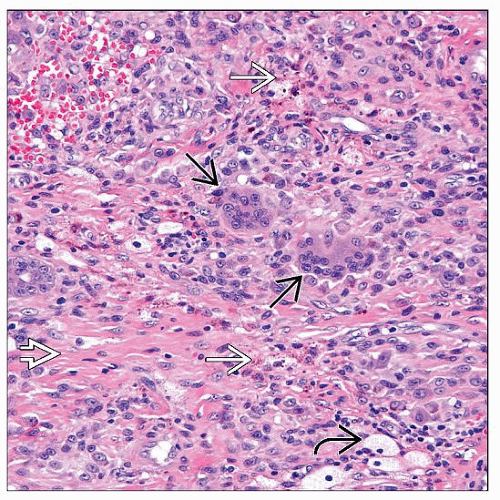
Polymorphous population of stromal cells, macrophages, and osteoclast-like giant cells
Stromal fibrosis and hemosiderin deposits
Mitotic rate: 1-20 mitoses per 10 high-power fields (average: 5/10)
Top Differential Diagnoses
Dermatofibroma
Giant cell tumor of soft tissue
Diffuse-type tenosynovial giant cell tumor/PVNS
TERMINOLOGY
Abbreviations
Giant cell tumor of tendon sheath (GCTTS)
Synonyms
Localized tenosynovial giant cell tumor, localized pigmented villonodular synovitis (PVNS), nodular tenosynovitis
Definitions
Benign soft tissue tumor of synovial origin
Polymorphous population of neoplastic stromal cells, macrophages, and osteoclast-like giant cells
Well circumscribed, noninvasive
ETIOLOGY/PATHOGENESIS
Histogenesis
Neoplastic growth
Balanced translocation involving 1p13 (CSF1 gene) in many tumors
CSF1 overexpression by neoplastic stromal cells
Recruitment and activation of intratumoral macrophages by CSF1R activation
CLINICAL ISSUES
Epidemiology
Incidence
2nd most common tumor of hand
Age
Any age; peak 3rd-4th decade
Gender
Women outnumber men 2:1
Site
Digits (85%)
Especially fingers (75%)
Tendon sheath (usually volar) or interphalangeal joint
Large joints (10%)
Ankle, knee, wrist, elbow
Bursa
Intraarticular tumors called localized PVNS
Skin secondarily involved in < 5% of cases
Presentation
Painless mass
Slow growing
Uncommon findings: Triggering, carpal and ulnar tunnel syndromes
Treatment
Surgical approaches
Complete local excision
Prognosis
Benign, but recurs locally (around 20%)
Risk factors for recurrence: Degenerative joint disease, distal phalanx, interphalangeal joint of thumb, osseous erosion
IMAGE FINDINGS
Radiographic Findings