aScoring: 0 = no errors; 1 = 1 error; 2 = ≥2 errors.
bAn answer of either Market or Market Street is acceptable.
cA total weighted error score of ≥9 indicates a need for further assessment.
Modified from Katzman R, Brown T, Fuld P, et al. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry 1983;140:734–739.
Assessment of Function
- Many disorders come to the attention of the physician if they are impairing job performance or function at home.
- Diagnoses such as dementia require documentation of new-onset functional impairment, and improvements in functional status are often used as a marker of treatment success.
- In addition, a review of the activities of daily living can assist in targeting additional assistance that may be needed at home.
- Clinicians should be prepared to quickly assess and document the presence of functional impairment due to any illness and should monitor for changes over time.
- Two mnemonics for basic and instrumental activities of daily living are listed in Table 38-2.2
TABLE 38-2 Activities of Daily Living
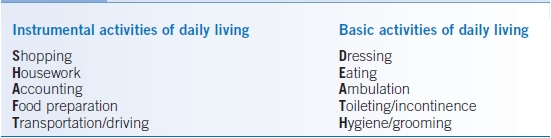
Modified from Fleming KC, Evans JM, Weber DC, et al. Practical functional assessment of elderly patients: a primary care approach. Mayo Clin Proc 1995;70:890–910.
Geriatric Assessment
- Geriatric assessment is a holistic approach to patient care and focuses on the physical, functional, social, and psychological health of the individual along with providing assistance to caregivers.
- Geriatric assessment can be practically performed in the outpatient setting by the primary care clinician in conjunction with a social worker or a gerontologic case manager, who can be consulted in difficult cases.
- The role of the social worker may include locating a chore worker to assist the caregiver, finding a durable power of attorney (DPOA), providing financial information, assisting with Medicare or Medicaid eligibility, management of caregiver stress, counseling, referral to state and local area agencies on aging, addressing advance directives, or recommending relocation to assisted living or long-term care centers.
- Geriatric evaluations should include the physical, functional, social, and psychological assessment of patients in the context of their current environment. These assessments can assist patients and their families regarding the myriad of issues that can affect the independence of frail older adults in the community.
Drug Prescribing in Older Adults
Factors That Affect Drug Metabolism
- The duration that a particular drug exerts its effect in any patient is based on the volume of distribution (Vd) of the drug, the metabolism of the drug (hepatic function), and the clearance (renal function), all of which can change with aging.
- The time for a drug to decline to one-half of its concentration is known as the drug’s biologic half-life. The half-life is directly proportional to the Vd and inversely proportional to the clearance. Vd is determined by the degree of plasma protein binding and by the patient’s body composition.
Age-Related Changes in Drug Metabolism
Changes in Body Composition
- The proportion of adipose tissue increases with aging. This increase results in a larger Vd and longer half-life, and therefore, lipophilic medications such as benzodiazepines have a longer duration of action.
- Total body water decreases by 15% in those >80 years of age. The Vd for hydrophilic drugs, such as lithium, cimetidine, and ethanol, is decreased, resulting in higher drug concentrations.
- On average, elderly persons have decreased lean body mass. Digoxin, which binds to muscle adenosine triphosphatase, may have a decreased Vd, resulting in toxicity at lower doses.
- The concentrations of plasma proteins such as albumin also tend to decline in older adults. This results in a reduced protein-bound form of many drugs and greater amount of free drug levels. Examples include digoxin, phenytoin, and warfarin. Most drug level determinations measure total (protein-bound and free levels) drug concentrations. Thus, total drug levels may not accurately reflect drug activity.
Changes in Hepatic and Renal Metabolism
- In general, there is a decrease in the number of hepatocytes and liver mass with age.
- Drugs that have a large first-pass effect in the liver, such as β-blockers, nitrates, calcium channel blockers, and tricyclic antidepressants (TCAs), may be effective at lower doses.
- Phase I (cytochrome P-450) oxidation declines on average with aging, and doses of medications such as benzodiazepines should be reduced. Knowledge about cytochrome P-450 drug interactions has grown and should be reviewed by all prescribing clinicians.
- Medications that are primarily excreted by the kidney often need to be adjusted by estimating creatinine clearance by age and body weight (see Chapter 23). Examples such as aminoglycosides, digoxin, atenolol, vancomycin, lithium, and acyclovir require dose reductions in older adults.
Changes in Pharmacodynamics
- End-organ responsiveness to a drug at the receptor level may change with age. Changes in receptor binding, a decrease in receptor number, or altered translation of a receptor-initiated cellular response into a biochemical reaction may be responsible.
- Consistent findings in the literature include the following:
- Decreased response to β-blockers.
- Increased sensitivity to benzodiazepines, opiates, warfarin, and anticholinergics.
- Clinicians should be aware that dose adjustments in these drugs may be necessary.
- Decreased response to β-blockers.
Steps in Preventing Polypharmacy and Drug Toxicity
Reducing Medications
- The initial step in assessing polypharmacy is to identify all prescription and over-the-counter drugs.
- Older adults may be treated by several physicians and obtain their medications at several pharmacies.
- The patient and, if necessary, a family member should bring in all medications to each visit for review including over-the-counter medications and herbal products.
- All drugs should be recorded by generic name, and unnecessary medications should be discontinued. The clinical indication should be identified for all drugs.
- The side effect profiles should be reviewed and safer medications substituted. Side effects may not be reported by patients, so obtaining a careful history focused on drug side effects is very important.
Starting New Medications
- Before a new drug is started, risk factors for adverse drug reactions, such as advanced age, liver or kidney disease, or use of multiple medications, should be identified.
- Providers should review a patient’s specific allergic reactions to medications, and drugs that have cross-reactivity should be identified.
- It is imperative to make a firm diagnosis before drug therapy is initiated.
- Attempts should be made to manage medical conditions (e.g., hypertension, diabetes) without drugs when possible.
- The clinician should establish a therapeutic goal and an appropriate time frame for treatment duration.
- Generic medications are generally preferred for their lower cost. However, this can be challenging when prescribing medications with a narrow therapeutic index. Significant variations may occur when changing between a name brand and generic or between different generic suppliers.
- Choosing a once-a-day drug, starting at a low dose, and titrating slowly are sound principles when prescribing to older adults.
- Avoid treating side effects of one drug with more drugs (e.g., treating edema from calcium channel blocker with furosemide).
Adherence
- The risk of medication errors increases dramatically with the number of medications taken by the patient.
- Several steps to improve adherence when ordering medications are suggested:
- Drug regimens should be simple.
- Use the same administration schedule with other drugs and time with a daily routine such as a meal.
- Instruct relatives and caregivers on drug regimens and enlist others, such as home health nurses and pharmacists, to assist with education and appropriate delivery.
- Be sure that the patient can afford the medication, has transportation to the pharmacy, can open the container, and read the label.
- Encourage the use of aids, such as pillboxes, calendars, and an updated medication record.
- Attempt to treat multiple problems with one medication.
- Drug regimens should be simple.
- Reviewing patients’ knowledge of the reason they take each medication and inquiring about adverse drug reactions on each visit are essential aspects of successful pharmacotherapeutic prescribing in the elderly.
Avoid Drugs with Anticholinergic Side Effects
- Medications with anticholinergic side effects can contribute to falls, cognitive impairment, delirium, and urinary retention in elderly patients. Physicians need to be aware of potential anticholinergic side effects of drugs.
- An anticholinergic risk scale (ARS) is available to estimate the extent to which an individual patient is at risk of anticholinergic side effects that may lead to cognitive impairment and delirium.3
- Higher ARS scores have been associated with an increased risk of anticholinergic adverse effects in elderly patients. High-risk medications include early TCAs, first-generation antihistamines, early typical antipsychotics, and oxybutynin. Moderate-risk medications include desipramine, nortriptyline, selective antihistamines, tolterodine, loperamide, and cimetidine. Relatively lower-risk medications include metoclopramide, mirtazapine, paroxetine, ranitidine, quetiapine, and risperidone.3
- Clinicians should be aware that even if an individual drug has weak anticholinergic activity (e.g., prednisone, furosemide), the combination of drugs may be cumulative and cause side effects.
- Higher ARS scores have been associated with an increased risk of anticholinergic adverse effects in elderly patients. High-risk medications include early TCAs, first-generation antihistamines, early typical antipsychotics, and oxybutynin. Moderate-risk medications include desipramine, nortriptyline, selective antihistamines, tolterodine, loperamide, and cimetidine. Relatively lower-risk medications include metoclopramide, mirtazapine, paroxetine, ranitidine, quetiapine, and risperidone.3
- Antibiotic overuse is a concern in older adults, and geographic areas with high prescribing rates could benefit from targeted programs to reduce unnecessary prescription.4
- High-risk drugs include insulin, warfarin, digoxin, sulfonylureas, benzodiazepines, and antipsychotics. These drugs should be prescribed with caution, especially in frail older adults with complex comorbidities.5
- In general, drugs should usually be tapered down at the same rate at which they were titrated up when the drug therapy was initiated. Common drugs that may require tapering include opioids, β-blockers, clonidine, gabapentin, memantine, selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), TCAs, and benzodiazepines.6
- In 2012, the American Geriatrics Society updated the Beers criteria for medications that should be used with caution in the elderly. The Beers criteria include but are not limited to first-generation antihistamines, antispasmodics, α1-blockers, TCAs with high anticholinergic side effects, digoxin >0.125 mg a day, antipsychotics, anxiolytics, metoclopramide, nonsteroidal antiinflammatory drugs (NSAIDs), and skeletal muscle relaxants.7
- More recently, Screening Tool of Older Person’s (potentially inappropriate) Prescriptions (STOPP) criteria for potentially inappropriate prescriptions (PIPs) were found to be more highly associated with adverse drug events that cause or contribute to urgent hospitalization when compared to Beers criteria.8 By the STOPP criteria, the most commonly prescribed inappropriate medications include proton pump inhibitors (>8 weeks), aspirin, benzodiazepines, loop diuretics (as first-line antihypertensives), NSAIDs (long-term use), opiates, and neuroleptics.
Falls
GENERAL PRINCIPLES
- Accidents were the eighth leading cause of death in the older adult population in 2011. Common accidents in older adults include falls and motor vehicle crashes. Burns, accidental poisoning, smoke inhalation, and hypothermia in demented patients are not uncommon, especially in patients with cognitive impairment.
- Falls are the leading cause of injury among the elderly and are important to identify and prevent in older adults.9
- Compared with adults 65 to 74 years old who fall, individuals 75 years old and older with falls are four to five times as likely to be admitted to a long-term care facility for a year or longer.10
- Safety issues should be addressed for all older adults. Extrinsic factors contribute to 30% of falls. Thus, home safety assessments, such as those provided by occupational therapists, should be considered to modify the environment to prevent falls and injuries.
- Osteoporosis should be identified and, if present, treated. Adequate calcium intake and vitamin D should be assessed and provided to all individuals.
- A family history of fracture, patient history of fracture or falls, gait difficulties, balance impairment, and/or medications should be evaluated and addressed.
Risk Factors
- To prevent falls and subsequent injury, a thorough review of the patient and environment is needed to target recommendations.11,12
- Risk factors for falling as identified by the U.S. Preventative Services Task Force (USPSTF) are advanced age, history of mobility difficulties and falls, as well as poor performance on the up-and-go test (see below).
- Common intrinsic factors contributing to falls in older adults include the following:
- Medical and neuropsychiatric conditions
- Gait and balance disorders
- Proximal muscle weakness
- Visual or hearing impairment
- Postural hypotension
- Vertigo
- Medical and neuropsychiatric conditions
- Common causes of these disorders include the following: dementia, Parkinson disease, diabetes, cerebrovascular accidents, peripheral neuropathy, deconditioning, arthritis, cataracts, glaucoma, foot abnormalities, and dehydration.
- Medications and human factors causing impaired cognition, delirium, and orthostatic hypotension contribute to falls. These include the following:
- Hypnotics, sedatives, anxiolytics, psychotropics, antihypertensives, diuretics, systemic glucocorticoids, and hypoglycemics
- Alcohol consumption and illicit drug use
- Hypnotics, sedatives, anxiolytics, psychotropics, antihypertensives, diuretics, systemic glucocorticoids, and hypoglycemics
- Syncope, seizures, vestibular dysfunction, acute illnesses, arrhythmia, subclavian steal, and carotid sinus hypersensitivity should be considered but are less common.
- Common extrinsic or environmental factors contributing to falls in older adults include the following:
- Lack of or inappropriate use of assistive devices (e.g., walker, cane, grab bars, raised toilet seat, shower chair) or improper footwear
- Environmental hazards such as low light, steps in poor repair, lack of railing, throw rugs, low-lying furniture, clutter, and pets.
- Lack of or inappropriate use of assistive devices (e.g., walker, cane, grab bars, raised toilet seat, shower chair) or improper footwear
Prevention
- Providing appropriate therapy for intrinsic risk factors and elimination or modification of extrinsic risk factors as described above are the first steps in prevention.
- A home occupational therapy assessment can assist with management of environmental risk factors.13
- Physical therapy is often helpful for gait and balance training, evaluation for an assistive device, and muscle strengthening when indicated.
- Community engagement in classes that focus on balance such as tai chi, group exercise classes, and home physiotherapy has shown a cumulative 13% decreased risk in falls in individuals at increased risk for falling.13
- Vitamin D supplementation, especially in individuals with low levels, has been shown to reduce the risk of falling.13
- There are mixed results on the use of hip protectors to prevent hip fractures from falls. A 2010 Cochrane review of randomized and quasi-randomized studies of hip protectors used in the community and nursing homes was unable to find significant benefit after eliminating several biased randomized controlled trials. However, hip protectors may reduce hip fractures in the frail elderly living in a nursing home setting if there is good compliance.14
- Vision correction is not associated with reduced risk of falling, but is associated with higher confidence of not falling.13
DIAGNOSIS
Clinical Presentation
- Careful history including thorough medication review, comprehensive review of symptoms (e.g., urinary frequency, nocturia), and evaluation for potential extrinsic as well as intrinsic factors should be completed.
- Screens that detect impairment in lower extremity muscle strength, gait, and balance appear to be a powerful predictor of disability in the older adult.15
- A lower extremity mobility screen such as the up-and-go test should be considered for older adults.16 Gait, balance, and strength are assessed during this test.
- Lower extremity strength can be assessed with a chair stand test (i.e., standing up from a chair and sitting down as quickly as possible with arms crossed against the chest). There are several variations of this test. One measures the time to complete five chair stands with a cutoff score of ≥12 seconds requiring further evaluation, while another version measures the number of chair stands completed in 30 seconds. Patients requiring the use of hands and those who are slow likely have lower extremity weakness. Endurance is also evaluated in the 30-second test.
- A progressive Romberg test may be used to evaluate balance.
- A lower extremity mobility screen such as the up-and-go test should be considered for older adults.16 Gait, balance, and strength are assessed during this test.
Diagnostic Testing
- Laboratory testing and/or if indicated neuroimaging should be performed.
- Laboratory tests include complete blood count (CBC), basic metabolic profile (BMP), glucose, vitamin B12, thyroid-stimulating hormone (TSH), and 25-hydroxyvitamin D.
- Bone density scan should be considered.
TREATMENT
- A thorough examination of the older adult for occult fractures on presentation after a fall is mandatory.
- A high clinical index of suspicion for a nondisplaced fracture should be maintained in older adults who have persistent joint pain and negative plain films. A low threshold should exist for obtaining a bone scan or MRI in these patients. Common occult fractures that are missed on plain films include pelvic insufficiency and hip fractures.
- CT scan of the head should be considered in a patient with a head injury. Anticoagulation status should be reviewed, and neurologic exam should be performed serially.
- Evaluate skin for hematomas. Clinical awareness for potential development of intramuscular or retroperitoneal hematomas is important, especially for patients on anticoagulation. Also refer to the Prevention section above.
Physical Activity
- Physical activity can be health enhancing. Inactivity has been associated with poor outcomes, and high levels of activity have been associated with improved morbidity, mortality, function, and quality of life. Data exist to indicate that physical activity reduces the risk for many diseases such as diabetes, stroke, cancer, osteoporosis, and depression. In older adults, exercise can promote weight loss, reduce falls and hip fractures, as well as reduce the risk of functional impairment and sarcopenia.
- Clinicians should counsel their patients on engaging in routine exercise. Patients should be provided with an activity prescription that emphasizes practical activity such as walking, gradual increase in activity over time, and referral to a supervised evidence-based program that can provide social support.
- 150 minutes a week (30 minutes 5 days a week) of moderate level of aerobic activity is recommended, if not limited for health reasons (e.g., cardiac, musculoskeletal).17
- Balance training, especially tai chi, has been associated with a reduction in fall risk.
- Resistance training is recommended three times a week for muscle strengthening, along with flexibility exercises.
- High-level intense activity such as running should be recommended with caution and close scrutiny, especially in those that have been extremely sedentary or have significant comorbid illnesses.
- Exercise can be part of a weight reduction program in older adults with elevated BMIs who are motivated to lose weight.
- Clinicians should consider adopting a brief assessment of the level of physical activity such as the Rapid Assessment of Physical Activity.18
Driving and Older Adults
GENERAL PRINCIPLES
- Driving issues in the older adult may come to the attention of the primary care physician due to concerns raised by the family or patient, the presence of comorbidities, or requests for referrals for fitness-to-drive evaluations from the Department of Motor Vehicles (DMV).
- Patients without dementia may have insight into their declining driving skills and may question their own ability to drive safely and/or avoid exposure to high-risk situations.
- Older adults are statistically the safest age group based on absolute crash risk per year, but are more vulnerable to injury than other age groups in motor vehicle crashes.
- The average older adult lives about 7 years without the ability to drive a car, and clinicians should assist transitions into driving retirement with community mobility counseling.
- There is no off-road test or group of tests that can provide a determination of who is fit to drive, but some tests have been associated with increased risk of a motor vehicle crash and/or impaired road performance.
DIAGNOSIS
Clinical Presentation
- The assessment should start with a history and physical examination as well as a functional assessment and some type of disease severity measure.19
- Inquiries about crashes, tickets, near misses, or becoming lost in previously familiar environments should be addressed to the patient and, if possible, a friend or family member. Information from an informant who has driven with the patient may be useful.
- A review of medications that have the potential to sedate the older adult should be sought, with efforts at drug reduction or substituting safer alternatives.
- A search for diseases that have the potential to increase crash risk should be pursued and may include, but are not limited to, dementia, psychiatric disorders, stroke, sleep apnea, arthritis, alcohol use, sensory deprivation, seizures, diabetes, or heart disease.
- Vision, hearing, attention, visuospatial skills, judgment, muscle strength, and flexibility should be assessed.
Diagnostic Testing
- The American Medical Association has recently recommended that office practitioners adopt a brief set of office tests that may identify older adults who are at risk for driving problems.20
- Referral to a subspecialist or neuropsychologist may be necessary if the primary care physician is unsure as to whether the patient is safe behind the wheel.
- Occupational therapists or driving rehabilitation specialists who have experience in assessing older drivers can be invaluable in the evaluation process with on-the-road tests or by recommending and implementing adaptive equipment.
TREATMENT
- Efforts should be made at stabilizing or improving comorbid illnesses or functional abilities when possible.
- Counseling older drivers to use safety restraints, refrain from drinking alcohol when driving, obey the speed limit, avoid cellular phones, and consider a refresher course for driving such as the American Association of Retired Persons (AARP) Driver Safety Program may be useful in reducing crash rates and injury.
- In the event that the clinician makes a recommendation to stop driving, this information should be communicated in a professional and sensitive manner and documented in the medical record.
- It is helpful to discuss alternate modes of transportation. If the clinician is not well versed in this area, referral to a social worker or gerontologic care manager may be in order.
- Patients may refuse to stop driving despite the advice of their physician or family or both.
- Demented drivers may lack insight into their own safety risk. Therefore, removing the car from the premises, hiding the car keys, changing the locks, filing down the ignition key, or disabling the battery cables may be necessary.
- Letters can be written to the DMV to reveal medical conditions and/or provide opinions on traffic safety and may be ethically appropriate. Some states have laws that grant physicians civil immunity from reporting unsafe drivers, and some have mandatory reporting requirements. Physicians should be aware of state and local requirements for reporting and obtain legal advice before breaching confidentiality.
Urinary Incontinence
GENERAL PRINCIPLES
- UI, involuntary leakage of urine, is a common problem for older adults. It is not a normal condition of aging.
- Women experience UI twice as frequently as men with its prevalence increasing with age. This may be due to a variety of factors including female urinary tract anatomy, childbirth, and/or menopause.21
- Reversible causes of UI can be remembered using the DIAPERS mnemonic: drugs (e.g., diuretics), infection, atrophic vaginitis, psychological (depression, delirium, dementia), endocrine (polyuria due to medical conditions such as hyperglycemia, hypercalcemia), restricted mobility or retention, and stool impaction.
- Anatomic causes of UI include the following:
- Nerve damage, spinal cord injury, and other neurologic disorders
- Anatomic floor defects, such as vaginal prolapse
- Enlarged prostate
- Cancer
- Nerve damage, spinal cord injury, and other neurologic disorders
Types of Incontinence
- Urge incontinence is part of the overactive bladder syndrome and is presumed to be due to uninhibited bladder contractions or detrusor overactivity.
- Stress incontinence or stress leakage occurs when increases in intra-abdominal pressure overcome sphincter closure mechanisms in the absence of a bladder contraction. Stress UI is the most common cause of UI in younger women and the second most common cause in older women. It may occur in older men after transurethral or radical prostatectomy.
- Mixed incontinence is the most common type of UI in women. This is generally thought to represent the overlap of two mechanisms: detrusor overactivity and impaired urethral sphincter function.
- Functional incontinence occurs in individuals with medical problems that effect mobility and cognition, interfering with their ability to reach a toilet without assistance.
- The term overflow incontinence has been used to describe the dribbling and/or continuous leakage associated with incomplete bladder emptying due to impaired detrusor contractility and/or bladder outlet obstruction. Leakage typically is small volume, although its continual nature can lead to significant wetting.
DIAGNOSIS
Clinical Presentation
History
- Patients may be reluctant discussing UI with a physician, so all women who have had children, patients at increased risk for UI (i.e., diabetes, neurologic disease), and all patients >65 years of age should be asked specifically about incontinence symptoms.
- Patients should be asked about symptoms compatible with urinary tract infections (UTI) such as dysuria/burning, frequency, urgency, suprapubic pain, hematuria, back/flank pain, and fever.
- Vaginal symptoms (discharge, odor, dryness, pruritus, and dyspareunia) may suggest a gynecologic cause.
- Urgency is accepted as both a sensitive and specific symptom for detrusor overactivity, but published trials are lacking.
- Leakage with stress maneuvers (e.g., coughing, nose blowing, laughing, bending over, running, changing position) is highly sensitive for stress UI.
- With overflow incontinence, there may be a weak urinary stream, dribbling, intermittency, hesitancy, frequency, and nocturia. It is seen more frequently in men and can be caused by blockage of the urethra, such as by prostate enlargement, stone or neoplasm, or constipation.
- A bladder diary of fluid intake, measured voided volumes, activities, and occurrences of urinary leakage is helpful.
- Assessment of quality of life is important along with cognitive and physical status.
Physical Examination
- Unless the history and/or other portions of the physical examination are highly suggestive of a specific cause, a genital and rectal examination should be done.
- A cough test with a full bladder to assess for urinary leakage may be performed in the office. Immediate leakage is consistent with stress UI, and delayed leakage is associated with urge UI.
Diagnostic Testing
- A urinalysis with reflex culture should be done to evaluate for a UTI.
- Postvoid residual volume should be measured; elevated levels are associated with overflow incontinence.
- Patients with complicated incontinence-associated extensive pelvic surgery, pelvic radiation, hematuria, recurrent UTIs, pain, possible fistula, high postvoid residual, significant pelvic prolapse, or failure to improve within the scope of your practice require referral to a urologist or urogynecologist for a more detailed evaluation (e.g., urodynamic testing, cystoscopy).
TREATMENT
The first step in the management of UI is to identify and/or treat reversible causes by avoiding caffeine, alcohol, and excessive fluid intake and treating UTIs, uncontrolled diabetes, and so forth.
Medications
- Pharmacologic treatment of UI is widely used for urge and mixed incontinence if behavioral therapy alone is not successful.
- Anticholinergics with antimuscarinic effects are the most frequently prescribed medications for urge incontinence. Commonly used agents include the following:
- Oxybutynin started at a low dose of 2.5 mg two to three times daily up to 20 mg/day in divided doses (immediate release) and 5 to 10 mg/day titrated by 5 mg/week to 30 mg/day maximum (extended release). It is also available in gel that can be applied to the shoulders, upper arms, abdomen, or thighs. It is also available over the counter as a transdermal patch.
- Tolterodine 1 to 2 mg twice a day (immediate release) and 2 to 4 mg/day (extended release).
- Fesoterodine, start 4 mg once daily, may increase to 8 mg once daily.
- Trospium 20 mg twice daily dose needs to be decreased to 20 mg once daily in the elderly and those with renal impairment (immediate release) and 60 mg daily with renal and hepatic exclusions (extended release).
- Because of their anticholinergic actions, patients need to be monitored for side effects (e.g., dry mouth, drowsiness, constipation, blurred vision, urinary retention).
- Oxybutynin started at a low dose of 2.5 mg two to three times daily up to 20 mg/day in divided doses (immediate release) and 5 to 10 mg/day titrated by 5 mg/week to 30 mg/day maximum (extended release). It is also available in gel that can be applied to the shoulders, upper arms, abdomen, or thighs. It is also available over the counter as a transdermal patch.
- Agents like solifenacin and darifenacin are more selective for M3 muscarinic acetylcholine receptors that are found in the bladder and gastrointestinal tract, but evidence for superior clinical efficacy and tolerability is not clear.
- β-3 adrenergic receptor agonists (selective, mirabegron) are extended-release antispasmodics, which relax bladder smooth muscle. This medication requires adjustment for both renal and hepatic disease.
- α-Adrenergic antagonists (nonselective: terazosin and doxazosin; selective: tamsulosin, alfuzosin, and silodosin) can be used in men with overflow incontinence due to benign prostatic hypertrophy (BPH).
- 5-α-reductase type I and II antagonists (finasteride and dutasteride) block the conversion of testosterone to 5-α-dihydrotestosterone, which may help men with BPH and urinary symptoms through prostate shrinkage. Tadalafil, a phosphodiesterase type 5 inhibitor, is also Food and Drug Administration (FDA) approved for BPH.
- Topical estrogen may be tried in postmenopausal women with atrophic vaginitis.
- OnabotulinumtoxinA (Botox) injections into the bladder cause muscle relaxation through acetylcholine antagonism. This procedure is FDA approved for those who cannot tolerate or do not adequately respond to anticholinergic medications.
Other Nonpharmacologic Therapies
- One to two voidings per night is normal in older adults. Sleep disorders should be excluded such as obstructive sleep apnea.
- For nocturia, patients should restrict fluid intake four hours before bedtime.
- Eliminate medications (e.g., alcohol, diuretics) causing or exacerbating UI, if possible.
- Pessaries may be used in women with vaginal or uterine prolapse.
- Nonpharmacologic behavioral interventions
- For stress and urge incontinence bladder retraining, regular voiding based on bladder diary and urgency control is recommended.
- Pelvic muscle/Kegel exercises also help control UI.
- Biofeedback can be used in combination with pelvic muscle exercises.
- For cognitively impaired population, prompted toileting every 2–3 hours during the daytime is recommended.
- For stress and urge incontinence bladder retraining, regular voiding based on bladder diary and urgency control is recommended.
- Neuromodulation is FDA approved for individuals with urge UI unresponsive to biofeedback and medications. Surgical placement is only completed if an external modulator yields a fifty percent reduction in symptoms.
Surgical Management
- Surgical treatment can be considered in stress UI when patients do not respond to medical treatment adequately.
- There are three main types of surgery for women with stress UI including retropubic suspension (Burch) and two types of sling procedures. Tension-free vaginal tape (TVT) is also being successfully used.
- Surgical treatments are available for men with UI due to nerve injury including artificial sphincter, male sling, and urinary diversion. Artificial sphincters can be created in women as well.
- Surgical treatment of BPH may also be indicated and effective but may result in postoperative incontinence due to prostatectomy itself.
SPECIAL CONSIDERATIONS
- For individuals unable to maintain adequate hygiene, pads or adult diapers should be encouraged along with routine disposal of soiled protective products and changing of soiled garments.
- Avoid the use of urinary catheters for UI or chronic urinary retention due to their increased risk of bacterial colonization. They may be considered in the treatment of nonhealing stage III or IV pressure ulcers or when requested by patient or family for comfort measures.
Pressure Ulcers
GENERAL PRINCIPLES
Definition
- The National Pressure Ulcer Advisory Panel (NPUAP) defines pressure ulcers (formerly called decubitus ulcers) as a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure alone or in combination with shear.
- As a pressure ulcer heals, it should be described as healing of the deepest stage of that particular ulcer’s history, regardless of the current depth of the ulcer.
- Eschar (necrotic tissue/scab) describes black, brown, or tan tissue adherent to the wound bed or ulcer edges.
- Slough is mucinous yellow or white tissue/dead cells found in the wound bed.
- Granulation tissue refers to pink or dark red tissue with a shiny, moist, granular appearance.
- Epithelial tissue is new pink or shiny white tissue (skin) that develops from the edges of the wound or as islands on the ulcer surface.
- Closed/resurfaced wounds are completely covered with epithelium.
Classification
- Stage 1: Skin intact but with nonblanchable redness for >1 hour after relief of pressure.
- Stage 2: Blister or other break in the dermis with partial thickness loss of dermis, with or without infection.
- Stage 3: Full-thickness tissue loss. Subcutaneous fat may be visible; destruction extends into muscle with or without infection. Undermining and tunneling may be present.
- Stage 4: Full-thickness skin loss with involvement of bone, tendon, or joint, with or without infection. Often includes undermining and tunneling.
- Unstageable: Tissue loss in which the depth of the ulcer is unable to be determined due partial or complete coverage by slough or eschar.
- Suspected deep tissue injury: Localized discoloration, purple or maroon in color, of intact skin or blister, indicating underlying soft tissue injury.
Risk Factors
- Risk factors include the following:
- Malnutrition/obesity.
- Immobility.
- Vascular insufficiency.
- Systemic illnesses/inflammatory states.
- Wet, macerated or dry, desiccated skin, both of which promote breakdown of the skin.
- Moisture from urinary or fecal incontinence and friction (pulling the patient across bed sheets).
- Shearing forces (patients sliding down a bed with the head elevated) can combine to damage tissue further.
- Malnutrition/obesity.
- Once the pressure on tissue exceeds intracapillary pressure (10 to 30 mm Hg), tissue ischemia can occur.
Prevention
- Relieve pressure by frequent position changes with scheduled repositioning of the patient while in bed, elevating heels off the bed and minimizing time in the seated position. Increasing patient mobility, exercise, massage, and/or physical therapy are also helpful.
- Keeping the skin dry, preventing friction, and avoiding shearing forces (lowering the head of the bed to <30 degrees) can assist in prevention and healing.
- Topical creams and lubricants can be helpful to treat dry skin, provide a skin barrier, and increase blood flow to the area of application (e.g., Extra Protective Cream).
- It is imperative to protect patients who are incontinent from being exposed to urine by frequently changing soiled garments and linens.
DIAGNOSIS
- The clinical diagnosis of pressure ulcers is relatively straightforward.
- The typical patient is elderly, but they also occur in patients with significant neurologic impairment and/or severe illness who spend considerable amounts of time sitting in a wheelchair or lying in bed.
- Typical locations include sacrum, ischial tuberosities, greater trochanters, lateral malleoli, and heels.
- Every ulcer should be staged and documented by a physician.
- It is worth noting that essentially all pressure ulcers are colonized with bacteria. Clinically significant wound infection may be suggested by erythema, warmth, swelling, tenderness, and purulent discharge.
- More deep-seated infections may present with symptoms and signs of cellulitis, osteomyelitis, and sepsis.
- Available testing modalities for osteomyelitis include plain radiography (limited sensitivity and specificity), MRI (high sensitivity but low specificity), CT, and nuclear imaging (operating characteristics very dependent on the clinical situation).
- Alternative or potentially coexistent conditions include venous insufficiency ulcers, arterial/ischemic ulcers, and diabetic neuropathic ulcers.
TREATMENT
- Treatment of pressure ulcers depends on the stage and severity of the ulcer. Providers should monitor closely for signs of infection as well as document the length, width, and presence of tunneling of the pressure ulcer using a validated scale for healing pressure ulcers. The pressure ulcer scale for healing (PUSH) tool is a research-validated tool and was developed by the NPUAP.22
- Adequate nutrition is critical for wound healing. Calorie, protein supplements, or both may be helpful adjuncts to promote healing of wounds.
- Recent data question the usefulness of vitamin C and zinc supplementation.
- Adequate pain control should be provided.
- A stage 1 ulcer is a warning that more serious tissue damage may follow if appropriate preventive measures are not instituted in a timely fashion. Preventive measures should be reviewed and intensified in this setting.
- A transparent film, adhesive, semipermeable polyurethane membrane can be used in stage 1 or 2 wounds to facilitate autolytic debridement.
- For stage 2 and 3 wounds, dressings and gels, such as hydrocolloids (e.g., DuoDERM, Tegasorb) and hydrogels (e.g., IntraSite, SoloSite), cover the wound bed facilitating autolytic debridement and provide a surface to which epithelial cells can migrate.
- Wet-to-dry dressings can be used for noninfected wounds. However, if not changed routinely, they simply remove migrating epithelial tissue and inhibit further healing.
- Topical enzymatic debridement agents with collagenase (e.g., Santyl ointment) and/or sharp mechanical debridement can be used to remove black eschar, with the goal of promoting granulating tissue, which promotes healing.
- Alginates (e.g., Kaltostat) are seaweed-derived, absorbent dressings. They form a gel-fiber matrix when in contact with fluid and can be helpful in moderate-to-heavy exudative stage 3 or 4 ulcers. Because they are nonadhesive, they can be easily removed but require a secondary dressing.
- Topical antibiotic creams are generally not used for routine wound care unless the area is infected. Polysporin, silver sulfadiazine, or mupirocin (the latter for methicillin-resistant Staphylococcus aureus) can be helpful in reducing bacterial counts.
- Systemic antibiotics should be used in cellulitis, deep-seated infections, and/or sepsis.
- Consultation with a general or plastic surgeon may be necessary to assist with wound closure. Options include debridement, flap procedures, or both.
SPECIAL CONSIDERATIONS
- In nonhealing wounds, bacterial or fungal infections should be considered; a stellate fungal rash may be present on the surrounding skin. This should be treated with an antifungal agent.
- Rarely, a temporary urinary catheter may need to be considered to improve healing in refractory cases.
- Support mattresses that use foam, air, or water can also assist in prevention or healing. Deep wounds into the muscle or bone (stage IV) or multiple nonhealing wounds may benefit from an air-fluidized bed or low-air-loss bed. However, their cost and size may be prohibitive.
- Weight distributing cushions for wheelchairs that use air, foam, and gel are also available and can be individualized for a patient’s specific needs. Donut-shaped devices should be avoided.
COMPLICATIONS
Osteomyelitis should be considered when bone is exposed or in nonhealing wounds that continue to drain or are exudative. Consultation for bone biopsy by a plastic surgeon or musculoskeletal radiologist should be considered for targeted antibiotic therapy. In chronic osteomyelitis, bone debridement may be necessary.
Malnutrition: Protein-Energy Undernutrition
GENERAL PRINCIPLES
- Weight loss due to decreased appetite or anorexia has a multitude of causes in the older adult and often is multifactorial. Causes may include but are not limited to the following:
- Therapeutic diets, such as a salt-restricted, low-cholesterol, or diabetic diets.
- Cachexia from advanced end-organ disease (e.g., congestive heart failure, chronic obstructive pulmonary disease [COPD]).
- Malabsorption.
- Cancer.
- Thyroid disease.
- Stress response from acute illness such as infection, trauma, or wounds.
- Chronic illness/inflammatory states, alcoholism, pain, anxiety, medications, decreased physical activity, loss of appetite, nonconducive environment, poor food preparation, consistency, and presentation, as well as poverty.
- Isolation, loneliness, depression, and cultural food preferences may also contribute.
- Difficulty with feeding due to hand and upper extremity disability, cognitive impairment, mental illness or psychosis, oral or dental disease, ill-fitting dentures, or excessive aerobic activity is not uncommon.
- Individuals living in nursing homes or in outpatient rehab are particularly at high risk.
- Therapeutic diets, such as a salt-restricted, low-cholesterol, or diabetic diets.
- The mnemonic MEALS ON WHEELS may be helpful to the clinician in identifying reversible causes for protein-energy malnutrition (Table 38-3).23
- Negative consequences of malnutrition include the following:
- Bone demineralization and fracture.
- Poor wound healing/chronic infections.
- Muscle wasting.
- Peripheral edema in the absence of cardiovascular disease.
- Cognitive and functional decline.
- Death. The risk of death in individuals residing in a long-term care facility who lose 5% of their bodyweight over the course of a month is 10 times higher than those gaining weight during a month.24,25
- Bone demineralization and fracture.
TABLE 38-3 Reversible Causes for Protein-Energy Malnutrition
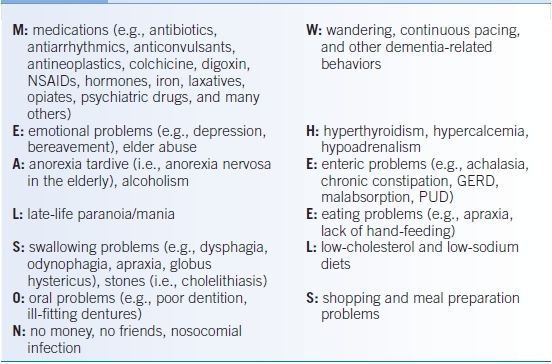
NSAIDs, nonsteroidal anti-inflammatory drugs; GERD, gastroesophageal reflux disease; PUD, peptic ulcer disease.
Modified from Morley J. Anorexia of aging: physiologic and pathologic. Am J Clin Nutr 1997;66:760–773.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


