Gastrostomy
John Daniel Hunter III
John Roland Porterfield Jr.
DEFINITION
A gastrostomy tube (G-tube) is a transcutaneous tube that is positioned in the lumen of the stomach. The primary functions of the G-tube are enteral access for nutrition and gastric decompression. They can be temporary or permanent depending on the patient’s underlying pathology and clinical needs.
A G-tube can be placed with an open, laparoscopic, endoscopic, or image-guided percutaneous approach.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history and physical exam should focus on the indication for enteral access, hemodynamic stability of the patient, current functional status of the gastrointestinal (GI) tract, and previous GI or upper abdominal surgeries.
Indications for G-tube include feeding access and gastric decompression. They also play a role as an additional method of gastropexy following antireflux procedures or to prevent gastric torsion.
Patients who are hemodynamically unstable should not undergo elective G-tube placement. In these scenarios, gastric access can be maintained through a nasogastric route.
Assessing the status of the GI tract is essential for operative planning and patient benefit.
If the G-tube is to be used for feeding, the patient should have a functional GI tract distal to the stomach and without evidence of mechanical bowel obstruction, adynamic ileus, GI ischemia, or peritonitis.
Safe access to the stomach via the oropharynx and esophagus needs to be verified prior to proceeding with percutaneous endoscopic gastrostomy (PEG) tube placement. If this route is obstructed or otherwise unsafe, an open, laparoscopic, or image-guided percutaneous technique should be used.
In patients with esophageal pathology that may necessitate an esophagectomy, a G-tube should be avoided because the stomach may be used as a conduit for reconstruction following esophagectomy. In this scenario, a feeding jejunostomy is our preferred route of enteral nutrition.
A thorough surgical history is imperative prior to G-tube placement. Patients with a history of previous upper abdominal or gastric surgery will be at higher risk for inadvertent colon or small bowel injury during PEG tube placement. An extensive abdominal surgical history may prohibit safe laparoscopic or endoscopic G-tube placement and thus an open technique may be the safest route.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Specific imaging or other diagnostic studies are generally unnecessary for G-tube placement. However, it is often the case that patients have had a plethora of upper abdominal imaging for other reasons that may provide valuable information or clues to previous unknown surgical procedures or unexpected anatomic findings.
For PEG tube placement, it is important to look for structures, particularly the liver and transverse colon, which may be resting anterior to the stomach along the line of the proposed G-tube tract. In patients with increased risk of abdominal adhesions (i.e., previous operations, history of peritonitis) and radiographic evidence of abdominal structures lying between the abdominal wall and stomach, PEG placement should be avoided in favor of a laparoscopic or an open approach.
SURGICAL MANAGEMENT
Preoperative Planning
The patient should be NPO for a minimum of 6 hours prior to the procedure.
Antibiotics should be given within 30 minutes of incision to reduce the incidence of abdominal wall infection around the tube site. First-generation cephalosporins are our preference when not contraindicated by a patient’s known allergies.
For patients undergoing a PEG tube placement, the patients should be provided an antiseptic mouth rinse to reduce oral flora being carried into the abdominal wall soft tissues.
Positioning
For endoscopic or surgical G-tube placement, the patient should be positioned supine.
For laparoscopic placement, the patient should be supine with the right arm tucked to allow adequate room for the surgeon and assistant to both work comfortably on the right side.
TECHNIQUES
PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TUBE PLACEMENT
Equipment
There are several PEG kits available. These vary depending on technique (push or pull) and tube size (20 French [Fr] or 28 Fr). Most of these kits come with everything needed for placement, including prep and sterile drapes. We use the Bard Ponsky PEG kit, 20 Fr.
A standard adult or pediatric endoscope is required, preferably with an external display so that both operating surgeons can see the endoscopic view.
Endoscopy and Tube Site Selection by Transillumination
With an endoscopist at the patient’s head and surgeon scrubbed at the patient’s abdomen, the room lights are dimmed and the endoscopist introduces the endoscope into the stomach.
A quick look around the entire stomach is performed to rule out occult gastric pathology.
The endoscopist should fully insufflate the stomach.
The endoscopist should advance the polypectomy snare to the end of the scope then withdraw 2 cm so that it is ready for the ensuing steps.
Transillumination will allow the surgeon to locate the appropriate place on the abdominal wall for the G-tube to be placed. This is done by retracting the scope into the body of the stomach several centimeters distal to the gastroesophageal junction and then directing it toward the anterior stomach.
Some endoscopic light sources offer a transilluminate feature that temporarily increases the light intensity to enhance visualization through the abdominal wall by the surgeon.
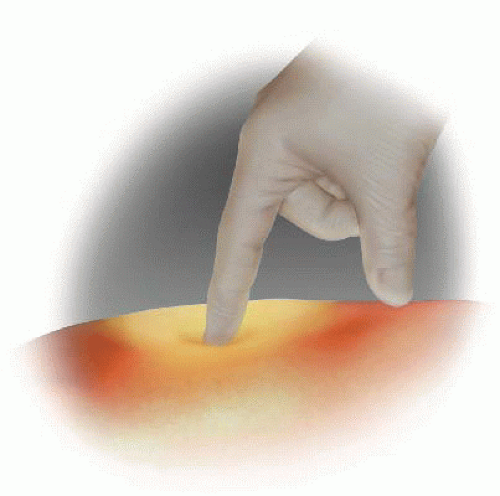
Palpation is sometimes required to compress the tissue between the stomach and skin to better reveal the light.
It is often necessary to darken the room to visualize the light.
Carefully palpate multiple areas and choose the spot with the brightest area of transillumination (FIG 1).
Ensure that the sight is at least 2 to 3 cm from the left costal margin for patient comfort.
Mark the spot with a marking pen or press the needleless tip of a Luer lock syringe into the skin to leave an indentation mark.
Insertion of a fine 25-gauge or 27-gauge needle, as used for infusion of local anesthesia, may be used to best identify the perfect placement position and tube track.
Optional Technique for Site Selection
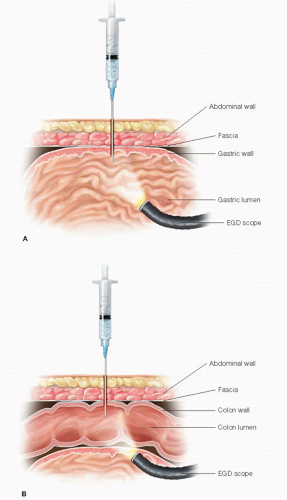
For additional assurance that there is no intervening bowel between the tube site chosen by transillumination and the stomach, the following technique can be used.1
Using a 10-mL syringe with several milliliters of saline and a small-gauge needle, advance the needle perpendicularly through the abdominal wall at the spot previously chosen, keeping the plunger drawn back.
Watch the saline in the syringe for air bubbles. If the initial presentation of bubbles is seen at the same time the endoscopist sees the needle from inside the stomach, you can safely assume you have not passed through any bowel before entering the stomach.
If you see bubbles before the endoscopist sees the needle from inside the stomach, you may be passing through bowel and thus should choose another point of entry and repeat (FIG 2).
During this process, it is important to limit the force applied to the abdominal wall as this may compress a portion of an unexpected piece of bowel lying along the proposed track.
Tube Placement
Infiltrate the site chosen with local anesthetic and make an approximately 0.5-cm skin incision with a no. 11 blade.
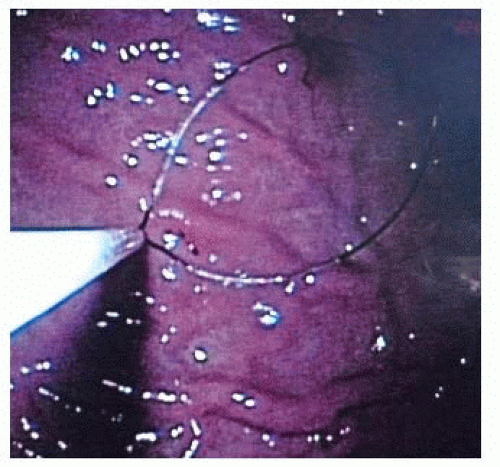
The endoscopist should advance the previously positioned polypectomy snare and center the loop over the area of the mucosa that was identified during abdominal wall site selection. This type of synchronization and planning not only facilitates a timely procedure but also avoids visceral movement once the best site is selected (FIG 3).
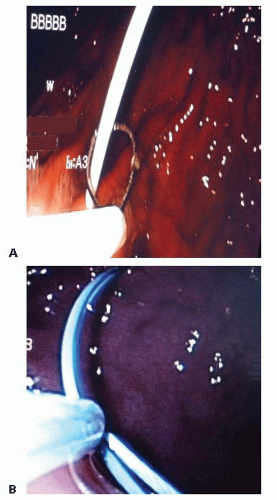
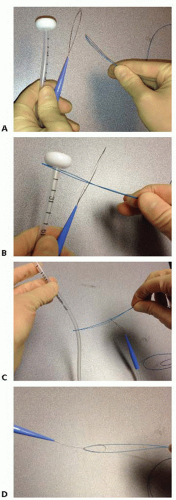
The needle with the angiocath is then placed through the abdominal wall at the designated site and advanced into the stomach under direct visualization into the loop created by the polypectomy snare. The needle is then removed while the angiocath is left in place (FIG 4A).
The snare is left loose.
The looped wire or the stiffer guidewire (see “Push Technique”) is advanced through the angiocath.
After several centimeters are passed through the snare, the snare loop is tightened around the wire (FIG 4B).
The scope is then completely withdrawn while the polypectomy snare is held snug around the wire, pulling the wire through the abdominal wall. This leaves the wire passing through the abdominal wall via the angiocath, into the stomach, through the esophagus, and out of the mouth.
At this point, there are two techniques available— “push” and “pull”—that can be chosen based on available supplies and surgeon’s preference.
Pull Technique
The looped wire that was pulled through the stomach to the mouth is connected to the looped wire at the tapered external end of the PEG tube (FIG 5).
The surgeon then pulls the suture from the abdominal wall end, advancing the PEG tube through the esophagus into the stomach. The endoscopist should follow the tube down to visualize from within the stomach. To save time, the polypectomy snare can be cinched around half of the button of the PEG tube to allow the scope to easily follow the tube while it is being pulled by the surgeon (FIG 6).
When the tapered end of the PEG tube begins to come through the abdominal wall, additional force directed perpendicular to the abdominal wall is required to pull the tube through (FIG 7).
The tube should be pulled until the button is resting loosely against the gastric mucosa.
The endoscopist should confirm position of the button to rule out bleeding while the surgeon notes the thickness of the abdominal wall when securing the bolster.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree