Gastrointestinal tract – physiology and drug absorption
Marianne Ashford
Chapter contents
Physiological factors influencing oral drug absorption
Physiology of the gastrointestinal tract
Transit of pharmaceuticals in the gastrointestinal tract
Mucus and the unstirred water layer
Key points
Introduction
The factors that influence the rate and extent of absorption depend upon the route of administration. As stated in Chapter 18, the intravenous route offers direct access to the systemic circulation and the total dose administered via this route is available in the plasma for distribution into other body tissues and the site(s) of action of the drug. Other routes will require an absorption step before the drug reaches the systemic circulation. Factors affecting this absorption will depend on the physiology of the administration site(s) and the membrane barriers present at those site(s) that the drug needs to cross in order to reach the systemic circulation. A summary of some of the properties of each route of administration is given in Chapter 1.
The gastrointestinal tract is discussed in detail in this chapter and a detailed description of the physiology of some of the other more important routes of administration is given in the relevant chapters of Part 5 of this book. The oral route of delivery is by far the most popular, with over 80% of medicines being given by mouth, mainly because it is natural and convenient for the patient and because it is relatively easy to manufacture oral dosage forms. Oral dosage forms do not need to be sterilized, are compact, and can be produced cheaply in large quantities by automated machines. This chapter and the next will therefore be confined to discussing the biopharmaceutical factors (that is, physiological, dosage form and drug factors) that influence oral drug absorption.
Physiological factors influencing oral drug absorption
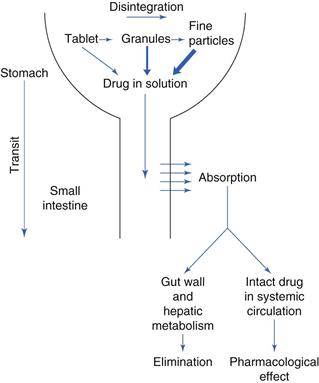
The gastrointestinal tract is complex. Figure 19.1 outlines some of the main structures involved in and key physiological parameters that affect oral drug absorption. In order to gain an insight into the numerous factors that can potentially influence the rate and extent of drug absorption into the systemic circulation, a schematic illustration of the steps involved in the release and absorption of a drug from a tablet dosage form is presented in Figure 19.2. It can be seen from this that the rate and extent of appearance of intact drug in the systemic circulation depend on a succession of kinetic processes.
The slowest step in this series, which is the rate-limiting step, controls the overall rate and extent of appearance of intact drug in the systemic circulation. The rate-limiting step will vary from drug to drug. For a drug which has a very poor aqueous solubility, the rate at which it dissolves in the gastrointestinal fluids is often the slowest step and the bioavailability of that drug is said to be dissolution-rate limited. In contrast, for a drug that has a high aqueous solubility, its dissolution will be rapid and the rate at which the drug crosses the gastrointestinal membrane may be the rate-limiting step termed permeability limited.
Other potential rate-limiting steps include the rate of drug release from the dosage form (this can be by design, in the case of controlled-release dosage forms), the rate at which the stomach empties the drug into the small intestine, the rate at which the drug is metabolized by enzymes in the intestinal mucosal cells during its passage through them into the mesenteric blood vessels, and the rate of metabolism of drug during its initial passage through the liver, often termed the ‘first-pass’ effect.
Physiology of the gastrointestinal tract
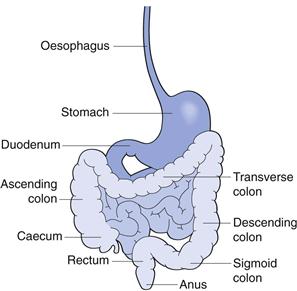
The gastrointestinal tract is a muscular tube, approximately 6 m in length with varying diameters. It stretches from the mouth to the anus and consists of four main anatomical areas; the oesophagus, the stomach, the small intestine and the large intestine or colon. The luminal surface of the tube is not smooth but very rough, thereby increasing the surface area for absorption.
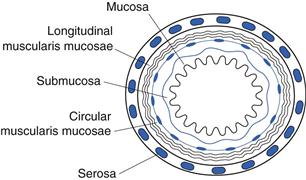
The wall of the gastrointestinal tract is essentially similar in structure along its length, consisting of four principal histological layers (Fig. 19.3):
The majority of the gastrointestinal epithelium is covered by a layer of mucus. This is a viscoelastic translucent aqueous gel that is secreted throughout the gastrointestinal tract, acting as a protective layer and a mechanical barrier. Mucus is a constantly changing mix of many secretions and exfoliated epithelial cells. It has a large water component (~95%). Its other primary components, which are responsible for its physical and functional properties, are large glycoproteins called mucins. Mucins consist of a protein backbone approximately 800 amino acids long and oligosaccharide side chains that are typically up to 18 residues in length.
The mucous layer ranges in thickness from 5 µm to 500 µm along the length of the gastrointestinal tract, with average values of around 80 µm. The layer is thought to be continuous in the stomach and duodenum but may not be so in the rest of the small and large intestines.
Mucus is constantly being removed from the luminal surface of the gastrointestinal tract through abrasion and acidic and/or enzymatic breakdown, and it is continually replaced from beneath. Turnover time has been estimated at 4–5 hours but this may well be an underestimate and is liable to vary along the length of the tract.
Oesophagus
The mouth is the point of entry for most drugs (so-called peroral – via the mouth – administration). At this point contact with the oral mucosa is usually brief. Linking the oral cavity to the stomach is the oesophagus. The oesophagus is composed of a thick muscular layer approximately 250 mm long and 20 mm in diameter. It joins the stomach at the gastrooesophageal junction, or cardiac orifice, as it is sometimes known.
The oesophagus, apart from the lowest 20 mm which is similar to the gastric mucosa, contains a well-differentiated squamous epithelium of non-proliferative cells. Epithelial cell function is mainly protective: simple mucous glands secrete mucus into the narrow lumen to lubricate food and protect the lower part of the oesophagus from gastric acid. The pH of the oesophageal lumen is usually between 5 and 6.
Materials are moved down the oesophagus by the act of swallowing. After swallowing, a single peristaltic wave of contraction, its amplitude linked to the size of the material being swallowed, passes down the length of the oesophagus at the rate of 20–60 mm per second, speeding up as it progresses. When swallowing is repeated in quick succession, the subsequent swallows interrupt the initial peristaltic wave and only the final wave proceeds down the length of the oesophagus to the gastrointestinal junction, carrying material within the lumen with it. Secondary peristaltic waves occur involuntarily in response to any distension of the oesophagus and serve to move sticky lumps of material or refluxed material to the stomach. In the upright position, the transit of materials through the oesophagus is assisted by gravity. The oesophageal transit of dosage forms is extremely rapid, usually of the order of 10–14 seconds.
Stomach
The next part of the gastrointestinal tract to be encountered by both food and pharmaceuticals is the stomach. The two major functions of the stomach are:
Another, perhaps less obvious, function of the stomach is its protective role in reducing the risk of noxious agents reaching the intestine.
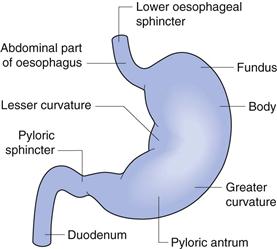
The stomach is the most dilated part of the gastrointestinal tract and is situated between the lower end of the oesophagus and the small intestine. Its opening to the duodenum is controlled by the pyloric sphincter. The stomach can be divided into four anatomical regions (Fig. 19.4); the fundus, the body, the antrum and the pylorus.
The stomach has a capacity of approximately 1.5 L, although under fasting conditions it usually contains no more than 50 mL of fluid, which are mostly gastric secretions. These include:
Contrary to popular belief, very little drug absorption occurs in the stomach owing to its small surface area compared to the small intestine. The rate of gastric emptying can be a controlling factor in the onset of drug absorption from the major absorptive site, the small intestine. Gastric emptying will be discussed under gastrointestinal transit later in this chapter.
Small intestine
The small intestine is the longest (4–5 m) and most convoluted part of the gastrointestinal tract, extending from the pyloric sphincter of the stomach to the ileocaecal junction where it joins the large intestine. It is approximately 25 to 30 mm in diameter. Its main functions are:
The small intestine is divided into the duodenum, which is 200–300 mm in length, the jejunum, which is approximately 2 m in length, and the ileum, which is approximately 3 m in length.
The wall of the small intestine has a rich network of both blood and lymphatic vessels. The gastrointestinal circulation is the largest systemic regional vasculature and nearly a third of the cardiac output flows through the gastrointestinal viscera. The blood vessels of the small intestine receive blood from the superior mesenteric artery via branched arterioles. The blood leaving the small intestine flows into the hepatic portal vein that carries it via the liver to the systemic circulation. Drugs that are metabolized by the liver are degraded before they reach the systemic circulation; this is termed hepatic presystemic clearance or first-pass metabolism.
The wall of the small intestine also contains lacteals, which contain lymph and are part of the lymphatic system. The lymphatic system is important in the absorption of fats from the gastrointestinal tract. In the ileum there are areas of aggregated lymphoid tissue close to the epithelial surface which are known as Peyer’s patches (named after the 17th century Swiss anatomist Johann Peyer). These cells play a key role in the immune response as they transport macromolecules and are involved in antigen uptake.
The surface area of the small intestine is increased enormously, by about 600 times that of a simple cylinder, to approximately 200 m2 in an adult, by several adaptations which make the small intestine such a good absorption site:
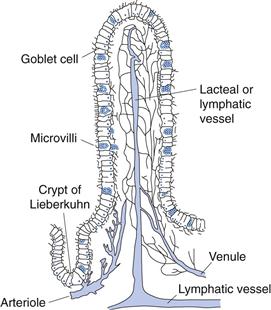
• Villi – these have been described as finger-like projections into the lumen (approximately 0.5–1.5 mm in length and 0.1 mm in diameter). They are well supplied with blood vessels. Each villus contains an arteriole, a venule and a blind-ending lymphatic vessel (lacteal). The structure of a villus is shown in Figure 19.5.
The luminal pH of the small intestine increases to between 6 and 7.5. Sources of secretions that produce these pH values in the small intestine are:
Colon
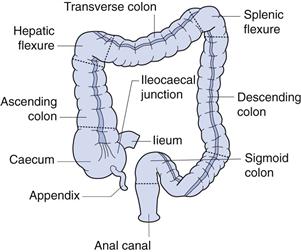
The colon is the final major part of the gastrointestinal tract. It stretches from the ileocaecal junction to the anus and makes up approximately the last 1.5 m of the 6 m of the gastrointestinal tract. It is composed of the caecum (~85 mm in length), the ascending colon (~200 mm), the hepatic flexure, the transverse colon (usually greater than 450 mm), the splenic flexure, the descending colon (~300 mm), the sigmoid colon (~400 mm) and the rectum, as shown in Figure 19.6. The ascending and descending colons are relatively fixed, as they are attached via the flexures and the caecum. The transverse and sigmoid colons are much more flexible.
The colon, unlike the small intestine, has no specialized villi. However, the microvilli of the absorptive epithelial cells, the presence of crypts and the irregularly folded mucosae serve to increase the surface area of the colon by 10–15 times that of a simple cylinder. The surface area nevertheless remains approximately l/30th that of the small intestine.
The main functions of the colon are:
The colon is permanently colonized by an extensive number (about 1012 per gram of contents) and variety of bacteria. This large bacterial mass is capable of several metabolic reactions, including hydrolysis of fatty acid esters and the reduction of inactive conjugated drugs to their active form. The bacteria rely upon undigested polysaccharides in the diet and the carbohydrate components of secretions such as mucus for their carbon and energy sources. They degrade the polysaccharides to produce short-chain fatty acids (acetic, proprionic and butyric acids), which lower the luminal pH, and the gases hydrogen, carbon dioxide and methane. Thus, the pH of the caecum is around 6–6.5. This increases to around 7–7.5 towards the distal parts of the colon.
Recently there has been much interest in the exploitation of the enzymes produced by these bacteria with respect to targeted drug delivery to this region of the gastrointestinal tract.
Transit of pharmaceuticals in the gastrointestinal tract
As the oral route is the one by which the majority of pharmaceuticals are administered, it is important to know how these materials behave during their passage through the gastrointestinal tract. It is known that the small intestine is the major site of drug absorption, and thus the time a drug is present in this part of the gastrointestinal tract is extremely important. If sustained- or controlled-release drug delivery systems are being designed, it is important to consider factors that will affect their behaviour and, in particular, their transit times through certain regions of the gastrointestinal tract.
In general, most dosage forms, when taken in an upright position, transit through the oesophagus quickly, usually in less than 15 seconds. Transit through the oesophagus is dependent upon both the dosage form and posture.
Tablets/capsules taken in the supine (lying down) position, especially if taken without water, are liable to lodge in the oesophagus. Adhesion to the oesophageal wall can occur as a result of partial dehydration at the site of contact and the formation of a gel between the formulation and the oesophagus. The chances of adhesion will depend on the shape, size and type of formulation. Transit of liquids, for example, has always been observed to be rapid, and in general faster than that of solids. A delay in reaching the stomach may well delay a drug’s onset of action or cause damage or irritation to the oesophageal wall, e.g. potassium chloride tablets.