14 The gastrointestinal system is essentially a muscular tube lined by a mucous membrane that exhibits regional variations, reflecting the changing functions of the system from mouth to anus. The mucous membrane is protective, secretory, absorptive or a combination of these in different parts of the tract (see Fig. 14.3). The muscle gives strength to the wall of the tract as well as moving the food along. Muscle is arranged somewhat differently in different areas of the tract. Because of its continuity with the external environment, the gastrointestinal system is a potential portal of entry for pathogenic organisms. As a result, the system incorporates a number of defence mechanisms which include prominent aggregations of lymphoid tissue, known as the gut-associated lymphoid system (GALT), distributed throughout the tract (see Ch. 11). FIG. 14.1 Parts of the gastrointestinal tract FIG. 14.2 Structure of the gastrointestinal tract Food is propelled along the gastrointestinal tract by two main mechanisms: voluntary muscular action in the oral cavity, pharynx and upper third of the oesophagus is succeeded by involuntary waves of smooth muscle contraction called peristalsis. Peristalsis and the secretory activity of the entire gastrointestinal system are modulated by the autonomic nervous system and a variety of hormones, some of which are secreted by neuroendocrine cells located within the gastrointestinal tract itself. These cells constitute a diffuse neuroendocrine system, with cells producing a variety of locally acting hormones found scattered along the whole length of the tract (see also Ch. 17). FIG. 14.3 Basic mucosal types in the gastrointestinal tract FIG. 14.4 Components of the wall of the gastrointestinal tract FIG. 14.5 Oesophagus FIG. 14.6 Oesophago-gastric junction FIG. 14.7 Stomach FIG. 14.8 Body of the stomach FIG. 14.9 Body of the stomach: structure of the gastric glands • Neuroendocrine cells, part of the diffuse neuroendocrine system, are also found in the base of the gastric glands. They secrete 5-HT (serotonin) and other hormones (see also Fig. 14.12).
Gastrointestinal tract
Introduction
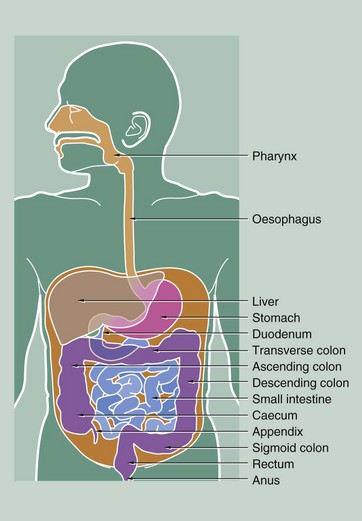
Ingestion and initial fragmentation of food occur in the oral cavity, resulting in the formation of a bolus of food. This is then conveyed to the oesophagus by the action of the tongue and pharyngeal muscles during swallowing. Secretion of saliva from major and minor salivary glands (see Ch. 13) aids fragmentation and lubricates the food for swallowing.
The oesophagus conducts food from the oral cavity to the stomach where fragmentation is completed and digestion begins. Initial digestion, accompanied by the intense muscular action of the stomach wall, converts the stomach contents to a semi-digested liquid called chyme. Chyme is squirted through a muscular sphincter, the pylorus, into the duodenum, the short first part of the small intestine. Digestive enzymes from a large exocrine gland, the pancreas, enter the duodenum together with bile from the liver via the common bile duct (see Ch. 15). Bile contains excretory products of liver metabolism, some of which act as emulsifying agents necessary for fat digestion. Duodenal contents pass along the rest of the small intestine where the process of digestion is completed and the main absorptive phase occurs. The middle segment of the small intestine is called the jejunum and the distal segment the ileum. There is no distinct anatomical boundary between these parts of the small bowel.
The liquid residue from the small intestine passes through the ileocaecal valve into the large intestine. Here, water is absorbed from the liquid residue, which becomes progressively more solid as it passes towards the anus. The capacious first part of the large intestine is called the caecum, from which projects a blind-ended sac, the appendix. The next part of the large intestine, the colon, is divided anatomically into ascending, transverse, descending and sigmoid segments, although histologically the segments are indistinguishable from one another. The terminal portion of the large intestine, the rectum, is a holding chamber for faeces prior to defaecation via the anal canal.
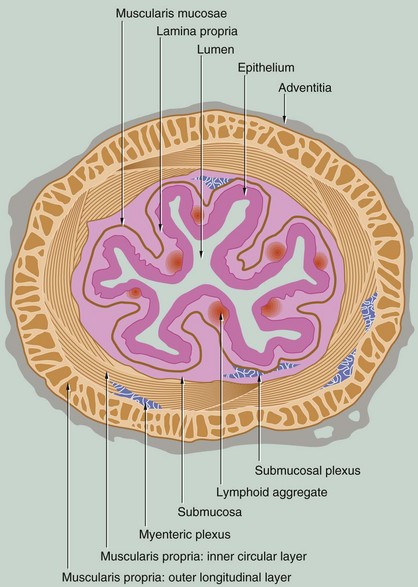
The structure of the gastrointestinal tract conforms to a general plan that is clearly evident from the oesophagus to the anus. The tract is essentially a muscular tube lined by a mucous membrane. There are minor variations in the arrangement of the muscular component in different parts of the gut, but much more striking are the marked changes in the structure and therefore function of the mucosa in the different regions of the tract.
The gastrointestinal tract has four distinct functional layers: mucosa, submucosa, muscularis propria and adventitia.
Autonomic regulation of certain glandular secretions and the smooth muscle of the gut and its blood vessels is mediated by the enteric nervous system, comprising postganglionic sympathetic fibres and ganglia and postganglionic fibres of the parasympathetic nervous system, supplied by the vagus nerve. Contraction of the smooth muscle of the bowel is initiated by pacemaker cells known as interstitial cells of Cajal, modulated by the autonomic nervous system, particularly the parasympathetic nervous system. As in other organs of the body, parasympathetic efferent fibres synapse with effector neurones in small ganglia located in or close to the organ involved. In the gastrointestinal tract, parasympathetic ganglia are concentrated in plexuses in the wall of the tract. In the submucosa, isolated or small clusters of parasympathetic ganglion cells give rise to postganglionic fibres which supply the mucosal glands and the smooth muscle of the muscularis mucosae. This submucosal plexus, Meissner plexus, also contains postganglionic sympathetic fibres arising from the superior mesenteric plexus. Larger clusters of parasympathetic ganglion cells are found between the two layers of the muscularis propria, the postganglionic fibres mainly supplying the surrounding smooth muscle. This plexus is known as the myenteric plexus or Auerbach plexus.
Glands are found throughout the tract at various levels in its wall. In some parts of the tract (i.e. stomach, small and large intestine), the mucosa is arranged into glands that secrete mucus for lubrication among other things. In the lower oesophagus and duodenum, glands penetrate the muscularis mucosae to lie in the submucosa. The pancreas and liver are large glands draining into the gastrointestinal lumen but lying entirely outside its wall (see Ch. 15).
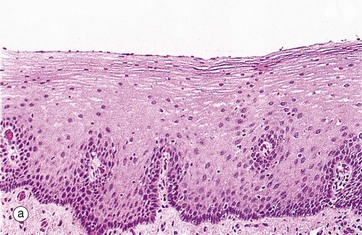
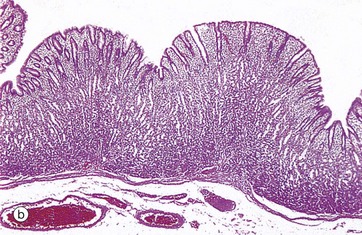
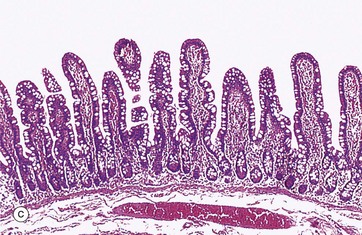
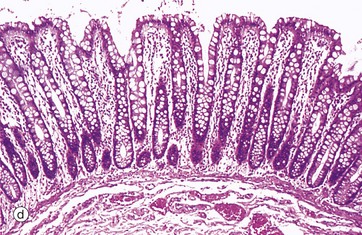
(a) Squamous mucosa, H&E (MP) (b) Gastric type secretory mucosa, H&E (LP) (c) Intestinal type absorptive mucosa, H&E (MP) (d) Colorectal type absorptive/protective mucosa, H&E (MP)
Four basic mucosal types are found lining the gastrointestinal tract and these can be classified according to their main function:
(a) Colon, H&E (HP) (b) Oesophagus, H&E (LP) (c) Colon, H&E (HP)
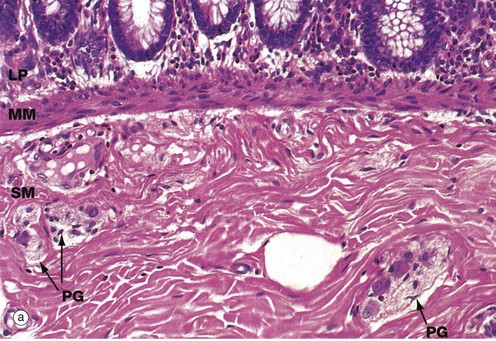
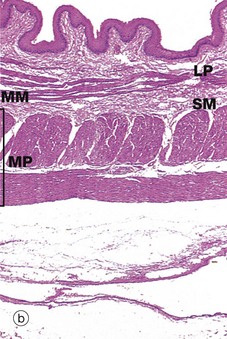
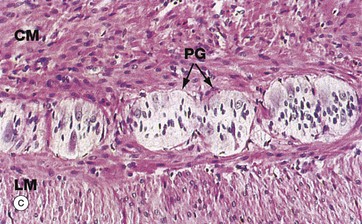
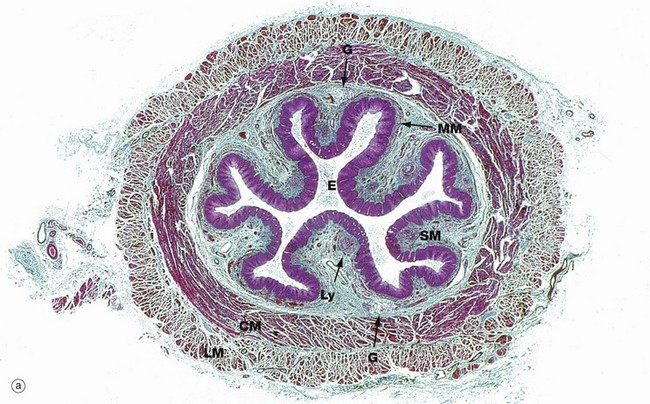
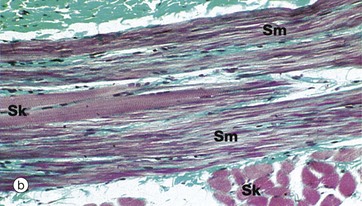
This series of micrographs illustrates the deeper layers of the wall of the gastrointestinal tract.
Micrograph (a) illustrates the muscularis mucosae MM, clearly demarcating the delicate lamina propria LP from the more robust underlying submucosa SM. This arrangement is typical of the whole of the gastrointestinal tract.
In most of the gut, the lamina propria consists of loose supporting tissue with a diffuse population of lymphocytes and plasma cells. The exception is the stomach which normally has few, if any, resident lymphoid cells. At intervals throughout the oesophagus, small and large bowels and appendix, prominent aggregates of lymphocytes with lymphoid follicles are found. There are also smaller numbers of eosinophils and histiocytes (see Fig. 4.21) to deal with any microorganisms breaching the intestinal epithelium until a specific immune response can be mounted. In the oesophagus, where the function of the mucosa is to protect against friction, the lamina propria is more collagenous than elsewhere and the muscularis mucosae is more prominent. The lamina propria is also typically rich in blood and lymphatic capillaries necessary to support the secretory and absorptive functions of the mucosa.
The muscularis mucosae consists of several layers of smooth muscle fibres, those in the deeper layers orientated parallel to the luminal surface. The more superficial fibres are oriented at right angles to the surface; in the small intestine, the fibres extend up into the villi (see Fig. 14.22). The activity of the muscularis mucosae keeps the mucosal surface and glands in a constant state of gentle agitation which expels secretions from the deep glandular crypts, prevents clogging and enhances contact between epithelium and luminal contents for absorption.
The submucosa consists of collagenous and adipose connective tissue that binds the mucosa to the main bulk of the muscular wall. The submucosa contains the larger blood vessels and lymphatics, as well as the nerves supplying the mucosa. Tiny parasympathetic ganglia PG are scattered throughout the submucosa, forming the submucosal (Meissner) plexus from which postganglionic fibres supply the muscularis mucosae.
The typical arrangement of the two layers of the muscular wall proper is seen in micrograph (b), which shows a longitudinal section of the oesophagus. The muscularis propria MP is made up of an outer longitudinal layer and a somewhat broader inner circular layer. There has been some artefactual separation of the layers in this micrograph, making them easier to visualise. The submucosa SM is separated from the lamina propria LP by the muscularis mucosae MM.
Micrograph (c) illustrates, at high magnification, the junction of outer longitudinal LM and inner circular CM layers of the muscularis propria in the large intestine. Between the layers, there are clumps of pale-stained parasympathetic ganglion cells of the myenteric (Auerbach) plexus. The two layers of the muscularis propria undergo synchronised rhythmic contractions that pass in peristaltic waves down the tract, propelling the contents distally. Peristalsis is initiated by the pacemaker cells, the interstitial cells of Cajal, but the level of activity is modulated by the autonomic nervous system, by locally produced gastrointestinal tract hormones and by other environmental factors. Parasympathetic activity enhances peristalsis while sympathetic activity slows gut motility.
(a) Masson trichrome stain (LP) (b) Masson trichrome stain (HP)
The oesophagus is a strong muscular tube that conveys food from the oropharynx to the stomach. The initiation of swallowing is a voluntary act involving the skeletal muscles of the oropharynx. This is then succeeded by a strong peristaltic reflex that conveys the bolus of food or fluid to the stomach. Food and fluid do not normally remain in the oesophagus for more than a few seconds and reflux is usually prevented by a physiological sphincter at the gastro-oesophageal junction (see textbox).
Below the diaphragm, the oesophagus passes a centimetre or so into the abdominal cavity before joining the stomach at an acute angle. Sphincter control appears to involve four complementary factors: diaphragmatic contraction, greater intra-abdominal pressure than intragastric pressure being exerted upon the abdominal part of the oesophagus, unidirectional peristalsis and maintenance of correct anatomical arrangements of the structures.
Micrograph (a) shows the lower third of the oesophagus. In the relaxed state, the oesophageal mucosa is deeply folded, an arrangement that allows marked distension during the passage of a food bolus. The lumen of the oesophagus is lined by a thick protective stratified squamous epithelium E (see Fig. 14.3). The underlying lamina propria is quite narrow and contains scattered lymphoid aggregates Ly. The muscularis mucosae MM is barely visible at this magnification.
The submucosa SM is quite loose with many elastin fibres, allowing for considerable distension during passage of a food bolus. The submucosa also contains small seromucous glands G, similar to salivary glands, which aid lubrication and are most prominent in the upper and lower thirds of the oesophagus.
The muscularis propria is thick, and inner circular CM and outer longitudinal LM layers of smooth muscle are clearly distinguishable. Since the first part of swallowing is under voluntary control, bundles of skeletal muscle predominate in the muscularis propria of the upper third of the oesophagus. In the middle third of the oesophagus, there is gradual transition from striated to smooth muscle and, in the lower oesophagus, the muscularis propria consists entirely of smooth muscle.
Micrograph (b) shows part of the muscularis propria of the upper oesophagus at high magnification in the area of transition from skeletal to smooth muscle fibres. A bundle of smooth muscle fibres Sm is seen, with two skeletal muscle fibres Sk in their midst. Other skeletal muscle fibres are seen in transverse section in the lower right of the micrograph. The cross-striations of the skeletal muscle are just visible at this magnification. The collagen of the endomysial supporting tissue stains green with this method.
H&E (LP)
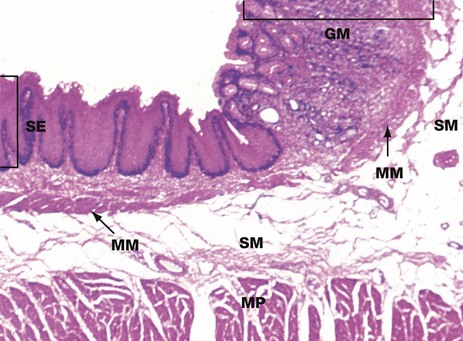
At the junction of the oesophagus with the stomach, the mucosa of the tract undergoes an abrupt transition from a protective stratified squamous epithelium SE to a tightly packed glandular secretory mucosa GM.
The muscularis mucosae MM is continuous across the junction, although it is less easily seen in the stomach where it lies immediately beneath the base of the gastric glands. The underlying submucosa SM and muscularis propria MP continue uninterrupted beneath the mucosal junction. The muscularis propria does not form a defined anatomical sphincter, but rather a physiological sphincter mechanism as described in Fig. 14.5.
Food passes from the oesophagus into the stomach, a distensible organ, where it may be retained for 2 hours or more. In the stomach, the food undergoes mechanical and chemical breakdown to form chyme. Solid foods are broken up by a strong muscular churning action while chemical breakdown is produced by gastric juices secreted by the glands of the stomach mucosa.
There is little absorption from the stomach except for water, alcohol and some drugs. Once chyme formation is completed, the pyloric sphincter relaxes and allows the liquid chyme to be squirted into the duodenum.
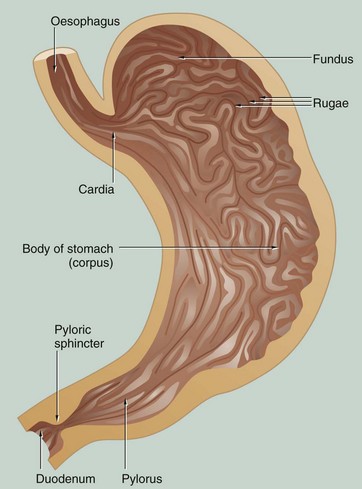
In the non-distended state, the stomach mucosa is thrown into prominent longitudinal folds called rugae that allow distension after eating. Anatomically, the stomach is divided into four regions: the cardia, fundus, body (corpus) and pylorus (pyloric antrum). The pylorus terminates in a strong muscular sphincter at the gastroduodenal junction.
The mucosa of the entire stomach has a tubular glandular form, but there are three distinctly different histological zones:
H&E (LP)
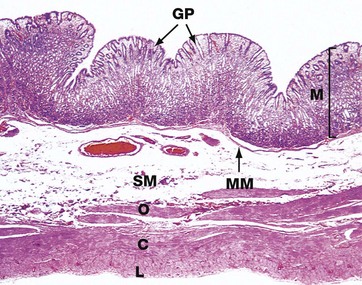
This micrograph illustrates the body of the stomach in the non-distended state. The mucosa M is thrown into prominent folds or rugae and consists of gastric glands that extend from the level of the muscularis mucosae MM to open into the stomach lumen via gastric pits or foveolae GP.
The muscularis propria comprises the usual inner circular C and outer longitudinal L layers, but the inner circular layer is reinforced by a further inner oblique layer O.
The submucosa SM is relatively loose and distensible and contains the larger blood vessels. The serosal layer, which covers the peritoneal surface, is thin and barely visible at this magnification.
The adipose tissue of the lesser and greater omentum is attached along the lesser and greater curvature of the stomach (not illustrated in this micrograph). Lymph nodes and large blood vessels lie within this omental fatty tissue.
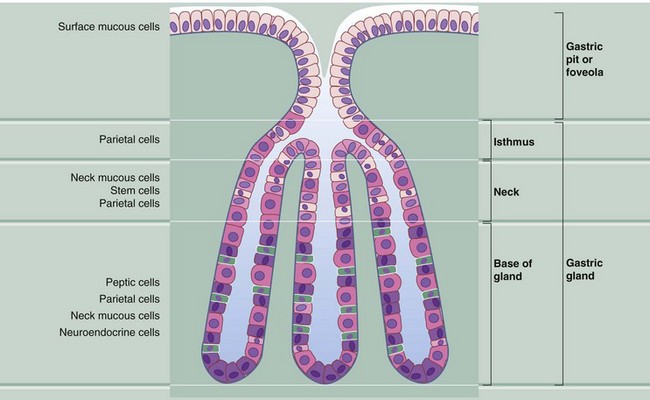
The mucosa of the fundus and body of the stomach consists of straight tubular glands that synthesise and secrete gastric juice. The gastric pits occupy about one-quarter of the thickness of the gastric mucosa and each has between one and seven gastric glands opening into it. Gastric juice is a watery secretion containing hydrochloric acid (pH 0.9–1.5) and the digestive enzyme pepsin, which hydrolyses proteins into polypeptide fragments. The stomach mucosa is protected from self-digestion by a thick surface covering of mucus, which is maintained at a higher pH than the gastric juice by the secretion of bicarbonate ions by the gastric surface mucous cells. The gastric glands contain a mixed population of cells:
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Gastrointestinal tract
