A. Anatomy
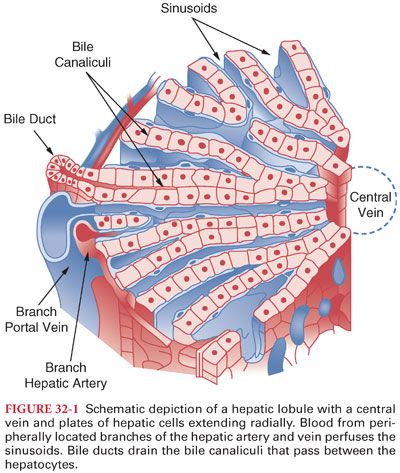
1. The liver is divided into four lobes consisting of 50,000 to 100,000 individual hepatic lobules (Fig. 32-1).
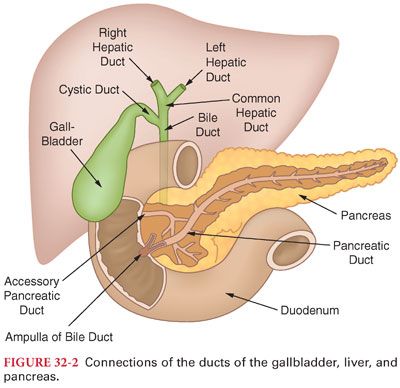
2. Each hepatocyte is also located adjacent to bile canaliculi, which coalesce to form the common hepatic duct. This duct and the cystic duct from the gallbladder join to form the common bile duct, which enters the duodenum at a site surrounded by the sphincter of Oddi (Fig. 32-2).
3. Hepatic lobules are lined by macrophages, which phagocytize 99% or more of bacteria in the portal venous blood (crucial because the portal venous blood drains the gastrointestinal tract and usually contains colon bacteria).
B. Hepatic Blood Flow
1. The liver receives a dual afferent blood supply from the hepatic artery and portal veins (Fig. 32-3).
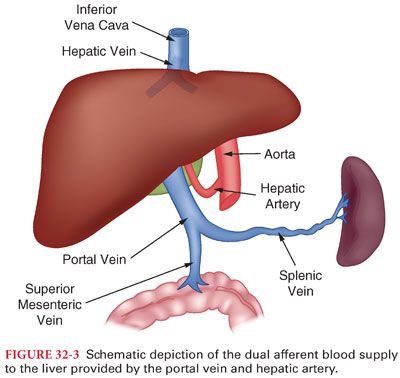
2. Total hepatic blood flow is approximately 1,450 mL per minute or approximately 29% of the cardiac output (portal vein provides 75% of the total flow but only 50% to 55% of the hepatic oxygen supply, and the hepatic artery provides only 25% of total hepatic blood flow but provides 45% to 50% of the hepatic oxygen requirements).
3. Hepatic artery blood flow maintains nutrition of connective tissues and walls of bile ducts (loss of hepatic artery blood flow can be fatal because of ensuing necrosis of vital liver structures).
C. Control of Hepatic Blood Flow
1. Portal vein blood flow, combined with the resistance to portal vein blood flow within the liver, determines portal venous pressure (normally 7 to 10 mm Hg).
2. Sympathetic nervous system innervation is from T3 to T11 and is mediated via α-adrenergic receptors (principally responsible for resistance and compliance of hepatic venules).
3. Fibrotic constriction characteristic of hepatic cirrhosis (most often due to chronic alcohol abuse and hepatitis C) can increase resistance to portal vein blood flow as evidenced by portal venous pressures of 20 to 30 mm Hg (portal hypertension).
a. The resulting increased resistance to portal vein blood flow may result in development of shunts (varices) to allow blood flow to bypass the hepatocytes.
b. Ascites results when increased portal venous pressures cause transudation of protein-rich fluid through the outer surface of the liver capsule and gastrointestinal tract into the abdominal cavity.
c. Hepatic artery blood flow is influenced by arteriolar tone that reflects local and intrinsic mechanisms (autoregulation). A decrease in portal vein blood flow is accompanied by an increase in hepatic artery blood flow by as much as 100%.
d. Surgical stimulation may decrease hepatic blood flow, independent of the anesthetic drug administered. The greatest decreases in hepatic blood flow occur during intraabdominal operations, presumably due to mechanical interference of blood flow produced by retraction in the operative area, as well as the release of vasoconstricting substances such as catecholamines.
D. Reservoir Function. The liver normally contains approximately 500 mL of blood or approximately 10% of the total blood volume (may accommodate as much as 1 L of extra blood with increased venous pressure).
1. As such, the liver acts as a storage site when blood volume is excessive, as in congestive heart failure, and is capable of supplying extra blood when hypovolemia occurs.
2. The liver is the single most important source of additional blood during strenuous exercise or acute hemorrhage.
E. Bile Secretion (see Fig. 32-2). Hepatocytes continually form bile (500 mL daily) and then secrete it into bile canaliculi, which empty into progressively larger ducts ultimately reaching the common bile duct. The most potent stimulus for emptying the gallbladder is the presence of fat in the duodenum, which evokes the release of the hormone cholecystokinin by the duodenal mucosa (this hormone causes selective contraction of the gallbladder smooth muscle).
1. Bile salts combine with lipids in the duodenum to form water-soluble complexes (micelles) that facilitate gastrointestinal absorption of fats (triglycerides) and fat-soluble vitamins (vitamin K is necessary for activation of several clotting factors).
2. Bilirubin. After approximately 120 days, the cell membranes of erythrocytes rupture and the released hemoglobin is converted to bilirubin in reticuloendothelial cells (Fig. 32-4).
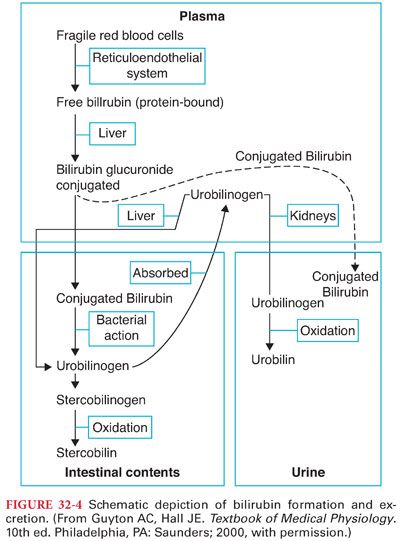
a. Jaundice is the yellowish tint of body tissues that accompanies accumulation of bilirubin in extracellular fluid. Skin color usually begins to change when the plasma concentration of bilirubin increases to approximately three times normal.
b. The most common types of jaundice are hemolytic jaundice, due to increased destruction of erythrocytes, and obstructive jaundice, due to obstruction of bile ducts.
F. Cholesterol is an important component of cell walls and is transported from the periphery to the liver as high-density lipoproteins (HDL). Once cholesterol has reached the liver, it can be excreted in the bile in association with bile acids (may precipitate as gallstones).
G. Metabolic Functions. Metabolism of carbohydrates, lipids, and proteins depends on normal hepatic function. Degradation of certain hormones (catecholamines and corticosteroids), as well as drugs, is an important function of the liver. Hepatocytes are the principal site for synthesis of all the coagulation factors with the exception of von Willebrand factor and factor VIIIC. Because the half-life of clotting factors produced in the liver is short, coagulation is particularly sensitive to acute hepatocellular damage.
1. Carbohydrates. Regulation of blood glucose concentration is an important metabolic function of the liver (when hyperglycemia is present, glycogen is deposited in the liver, and when hypoglycemia occurs, glycogenolysis provides glucose).
2. Lipids. The liver is responsible for β-oxidation of fatty acids and formation of acetoacetic acid. Synthesis of fats from carbohydrates and proteins also occurs in the liver.
3. Proteins
a. The most important liver functions in protein metabolism are oxidative deamination of amino acids, formation of urea for removal of ammonia, formation of plasma proteins and coagulation factors, and interconversions (transfer of one amino group to another amino acid) among different amino acids.
b. Albumin formed in the liver is critically important for maintaining plasma oncotic pressure as well as providing an essential transport role (half-time for albumin is about 21 days such that plasma albumin concentrations are unlikely to be significantly altered in acute hepatic failure).
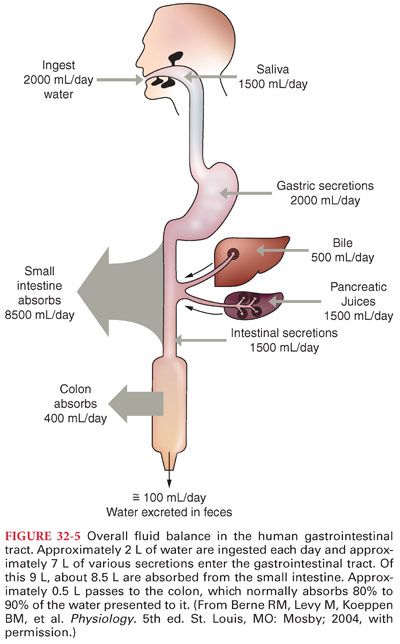
II. Gastrointestinal Tract. The primary function of the gastrointestinal tract is to provide the body with a continual supply of water, electrolytes, and nutrients. Overall, approximately 9 L of fluid and secretions enters the gastrointestinal tract daily, and all but approximately 100 mL is absorbed by the small intestine and colon (Fig. 32-5). The pH of gastrointestinal secretions varies widely (Table 32-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


