IV. Histamine Receptor Antagonists. Histamine induces contraction of smooth muscles in the airways, increases the secretion of acid in the stomach, and stimulates release of neurotransmitters in the central nervous system (CNS). Histamine receptor antagonists bind to receptors on effector cell membranes, to the exclusion of agonist molecules, without themselves activating the receptor (histamine receptor antagonists do not inhibit release of histamine).
A. H1-Receptor Antagonists. H1-receptor antagonists are characterized as first-generation and second-generation receptor antagonists. First-generation drugs tend to produce sedation, whereas second-generation drugs are relatively nonsedating (Table 35-2). The selectivity of the second-generation antagonists for H1 receptors decreases CNS toxicity.
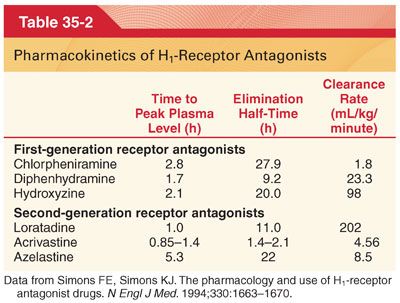
1. Pharmacokinetics. H1-receptor antagonists are well absorbed after oral administration, often reaching peak plasma concentrations within 2 hours (Table 35-3).
2. Clinical Uses
a. H1-receptor antagonists prevent and relieve the symptoms of allergic rhinoconjunctivitis (sneezing, nasal and ocular itching, rhinorrhea, tearing, and conjunctival erythema) but they are less effective for the nasal congestion characteristic of a delayed allergic reaction. First-generation H1-receptor antagonists have sedating effects that result in delayed reaction times.
b. Diphenhydramine is prescribed as a sedative, an antipruritic, and as an antiemetic (in combination with systemic or neuraxial opioids to control nausea and pruritus, there is the conceptual risk of depression of ventilation but diphenhydramine counteracts to some extent the opioid-induced decreases in the slope of the ventilatory response to CO2 and does not exacerbate the opioid-induced depression of the hypoxic ventilatory response during moderate hypercarbia).
c. Use of antihistamines in the acute treatment of anaphylactic reactions is directed at blocking further histamine-mediated vasodilation and resulting hemodynamic instability, as well as decreasing respiratory and other systemic complications. As such, the administration of H1-receptor antagonists plus the administration of epinephrine is indicated in the treatment of acute anaphylaxis. These drugs may also be administered prophylactically for anaphylactoid reactions to radiocontrast dyes.
3. Side Effects
a. First-generation H1 antagonists often have adverse effects on the CNS, including somnolence, diminished alertness, slowed reaction time, and impairment of cognitive function.
b. Tachycardia is common, and prolongation of the QTc interval on the electrocardiogram (ECG), heart block, and cardiac arrhythmias have occurred.
c. Second-generation H1 antagonists are unlikely to produce CNS side effects and enhancement of the effects of diazepam or alcohol is unlikely by second-generation drugs.
d. Antihistamine intoxication is similar to anticholinergic poisoning and may be associated with seizures and cardiac conduction abnormalities resembling tricyclic antidepressant overdose.
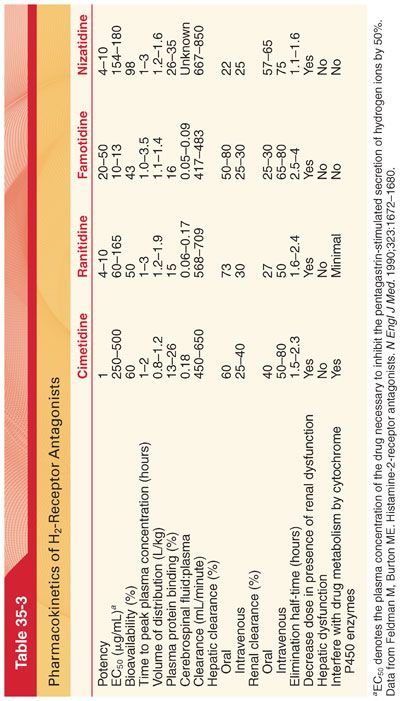
B. H2-Receptor Antagonists. Cimetidine, ranitidine, famotidine, and nizatidine are H2-receptor antagonists that produce selective and reversible inhibition of H2 receptor–mediated secretion of hydrogen ions by parietal cells.
1. Mechanism of Action. The histamine receptors on the basolateral membranes of acid-secreting gastric parietal cells are of the H2 type and thus are not blocked by conventional H1 antagonists.
a. The relative potencies of the four H2-receptor antagonists for inhibition of secretion of gastric hydrogen ions varies from 20- to 50-fold, with cimetidine as the least potent and famotidine the most potent (see Table 35-3).
b. The duration of inhibition ranges from approximately 6 hours for cimetidine to 10 hours for ranitidine, famotidine, and nizatidine.
2. Pharmacokinetics. The absorption of cimetidine, ranitidine, and famotidine is rapid after oral administration. Because of extensive first-pass hepatic metabolism, however, the bioavailability of these drugs is approximately 50% (see Table 35-3).
a. Hepatic dysfunction does not seem to significantly alter the pharmacokinetics of H2-receptor antagonists.
b. Increasing age must be considered when determining the dose of H2-receptor antagonists (cimetidine clearance decreases 75% between the ages of 20 years and 70 years.)
3. Clinical Uses
a. In the preoperative period, H2-receptor antagonists have been administered as chemoprophylaxis to increase the pH of gastric fluid before induction of anesthesia. However, the American Society of Anesthesiologists’ practice guidelines for preoperative fasting and the use of pharmacologic agent to reduce the risk of pulmonary aspiration state that the routine preoperative use of medications that block gastric acid secretion to decrease the risks of pulmonary aspiration in patients who have no apparent increased risk for pulmonary aspiration is not recommended.
b. When indicated though, H2-receptor antagonists have been advocated as useful drugs in the preoperative period to decrease the risk of acid pneumonitis if inhalation of acidic gastric fluid were to occur in the perioperative period (cimetidine, 300 mg orally, 1.5 to 2.0 hours before the induction of anesthesia, with or without a similar dose the preceding evening; famotidine given the evening before and the morning of surgery or on the morning of surgery).
c. H2-receptor antagonists, in contrast to antacids, have no influence on the pH of the gastric fluid that is already present in the stomach.
d. H2-receptor antagonists cross the placenta but do not adversely affect the fetus when administered before cesarean section.
e. Preoperative preparation of patients with allergic histories or patients undergoing procedures associated with an increased likelihood of allergic reactions (radiographic contrast dye administration) may include prophylactic oral administration of an H1-receptor antagonist (diphenhydramine, 0.5 to 1.0 mg/kg) and an H2-receptor antagonist (cimetidine, 4 mg/kg) every 6 hours in the 12 to 24 hours preceding the possible triggering event. A corticosteroid administered at least 24 hours earlier is commonly added to this regimen.
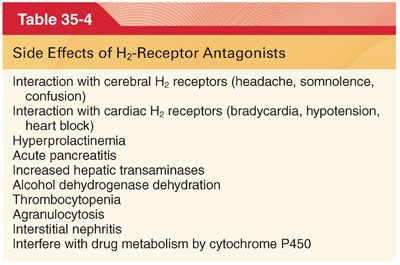
4. Side Effects (Table 35-4)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


