b. The larynx serves as the organ of phonation, plays an important role in coughing, and in airway protection from aspiration.
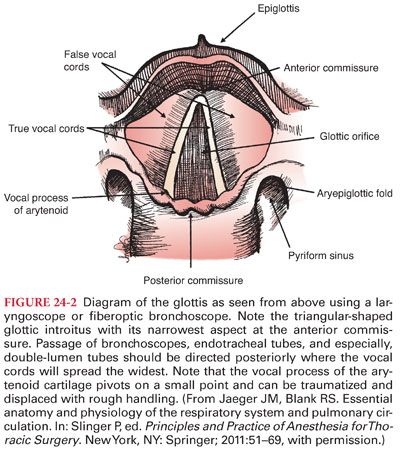
c. The paired vocal cords attach posteriorly to the vocal process of each arytenoid and anteriorly meet at the junction of the thyroepiglottic ligament of the anterior portion of the thyroid cartilage. The triangular opening formed by the vocal ligaments is the glottis with its apex anteriorly (Fig. 24-2).
B. Pharyngeal Innervation. Innervation of the pharynx is supplied via sensory and motor branches of the glossopharyngeal nerve (CN IX) and vagus nerve (CN X) (external and internal branches of the superior laryngeal nerves, recurrent laryngeal nerves).
C. Tracheal and Bronchial Structure
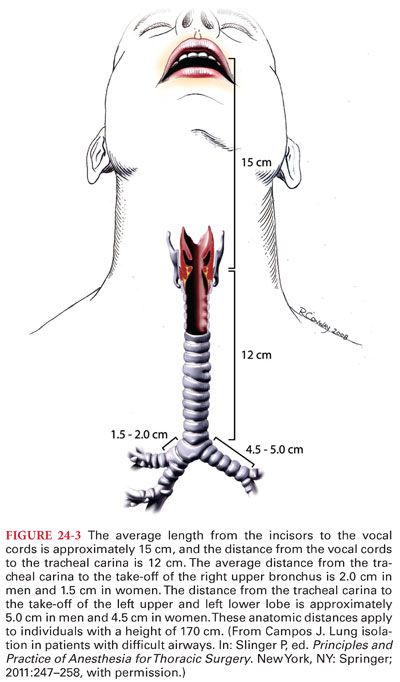
1. The trachea originates at the cricoid cartilage (at the level of vertebra C6) and extends approximately 10 to 12 cm (females) and 12 to 14 cm (males) to terminate in a bifurcation (carina) at the T4/5 vertebral level (2nd intercostal space, the angle of Louis) (Fig. 24-3).
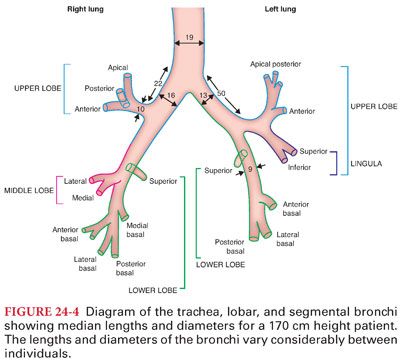
2. The right main bronchus is wider (16 vs. 13 mm), shorter (1.5 to 2.5 vs. 4.5 to 5 cm) and more vertical than the left (Fig. 24-4).
D. Respiratory Airways and Alveoli. The airways continue to divide into smaller diameter conduits until one arrives at the bronchioles with diameters less than 0.8 mm. The immune defenses of the lung are extremely important because of the direct exposure of this organ to the external environment via the airways. Exaggerated inflammatory response and the activity of these cells and others may be harmful to the lung; acute respiratory distress syndrome (ARDS) and emphysema are examples.
III. Pulmonary Circulation
A. Blood flow through the pulmonary circulation is normally equal to the blood flow through the systemic circulation (a major exception being intracardiac shunting when it exceeds systemic circulation).
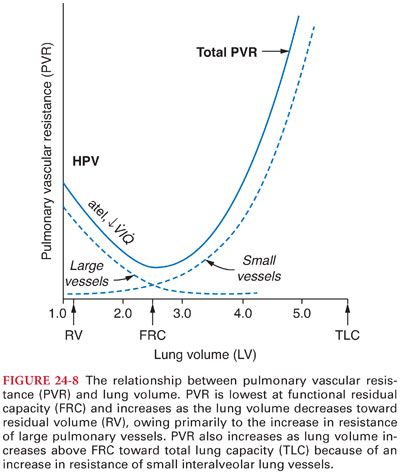
B. Pressures in the pulmonary circulation are normally lower than the systemic circulation because the pulmonary vascular resistance (PVR) is lower than the systemic resistance (approximately one-sixth of systemic resistance).
C. Only one-third of the bronchial circulation returns to the systemic venous system; the remainder drains into the pulmonary veins and this constitutes the largest portion of the normal extrapulmonary venoarterial shunt. This bronchial shunt is less than 1% of the cardiac output in healthy individuals but may increase to 10% in bronchiectasis, emphysema, and some congenital cardiac conditions.
IV. Thorax and Muscles of Respiration. The bony thorax is composed of the 12 ribs, the sternum anteriorly, and the thoracic vertebral column posteriorly. The caudal end of the thorax is formed by the diaphragm, and the cranial end of the thorax is the thoracic inlet, within the ring formed by the first ribs, containing the trachea, esophagus, and the neurovascular supply to the head and arms. Bulk movement of air into and out of the lungs occurs as a result of changes in intrathoracic pressure created by rhythmic changes in the volume of the thorax. Expansion of the chest cavity occurs when three respiratory muscle groups (diaphragm, intercostal, and accessory) work in concert.
A. Inspiration
1. The diaphragm is unique in that its muscle fibers radiate from a central tendinous structure to insert peripherally on the ventrolateral aspect of the first three lumbar vertebrae, the aponeurotic arcuate ligaments, the xiphoid process, and the upper margins of the lower six ribs.
2. Contraction of the diaphragm causes a large caudal displacement of the central tendon resulting in a longitudinal expansion of the chest cavity.
3. The fall in pleural pressure and accompanying lung expansion produce an increase in abdominal pressure and outward movement of the abdominal wall. The supine and Trendelenburg positions or surgical retractors can significantly interfere with this abdominal motion especially in the morbidly obese, necessitating controlled ventilation under anesthesia.
B. Expiration is a passive process in quiet breathing and is largely the response to relaxation of the inspiratory muscles and the balance of forces generated by the elastic recoil of the lungs and chest wall.
1. When high levels of ventilation are required as in exercise or if airway resistance increases (as in exacerbations of asthma or COPD), the expiratory phase becomes an active process with forceful contraction of the rectus abdominis, the transverse abdominis, and the internal and external oblique muscles.
2. Innervation of the abdominal musculature is from thoracic nerves 7 through 12 and the first lumbar nerve.
V. Respiratory Mechanical Function. The basics of mechanical function of the respiratory system are the interaction of two opposing springs: the chest wall, which at rest is trying to expand, and the lungs, which at rest are trying to contract. The lungs and chest wall move together as a unit (made possible by the enclosed, air-tight thoracic cavity where the outer surface of the lungs and its visceral pleura are in close proximity to the parietal pleura, covering the inner surface of the chest wall and the mediastinal structures). The volume of gas contained in the lungs at this resting point is termed functional residual capacity (FRC). For a healthy young adult male, total lung capacity (TLC) will be approximately 6 to 6.5 L and FRC will be 2.5 to 3 L. The oxygen contained in the FRC (500 to 600 mL) is the only reservoir of oxygen in the body. Pathologic conditions such as the introduction of air or blood into the intrapleural space (pneumothorax, empyema, pleural effusion, bronchopleural fistula) can rapidly disrupt this lung–chest wall interaction, leading to a compromise in respiratory function but also interfere with cardiovascular function.
A. Lung Volumes and Spirometry
1. By convention, the static and dynamic subdivisions of gas contained within the lung are given a common nomenclature of volumes and capacities (Table 24-1) (Fig. 24-5).
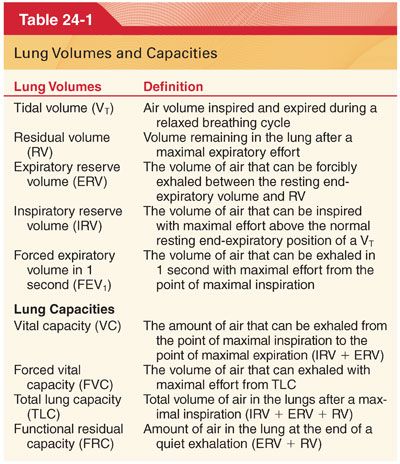
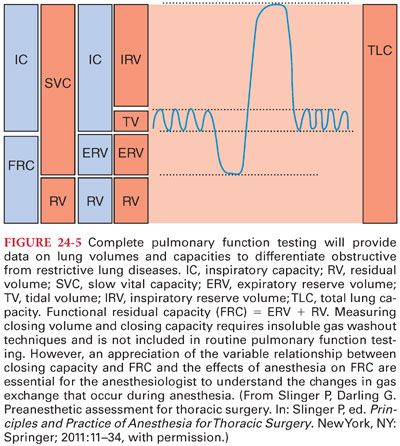
2. Volumes are most commonly measured by spirometry (Figs. 24-6 and 24-7) and capacities are then calculated as the sum of specific volumes.
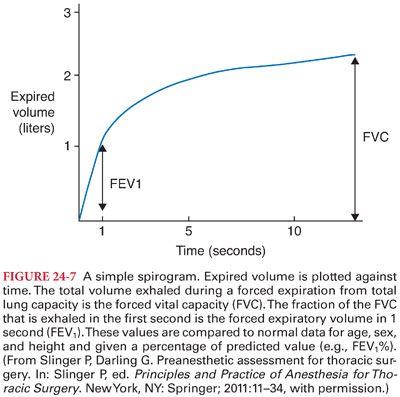
3. Complete pulmonary function testing in the laboratory will commonly report measurements of volume ratios, flows, lung resistance, and lung diffusion capacity for carbon monoxide (DLCO).
B. Closing Capacity and Closing Volume
1. The key to understanding the complex changes that develop in the respiratory system during anesthesia is to appreciate the relationship between FRC and closing capacity (CC). CC is the sum of closing volume (CV) and RV.
2. CV is the lung volume below which small airways begin to close (or at least cease to contribute expiratory gas) during expiration.
3. When an alveolar unit falls below its CC, even for a brief period during one respiratory cycle, the concentration of oxygen (PAO2) in that unit falls slightly. This results in the increase of venoarterial admixture (“shunt”) and decrease in arterial oxygen tension (PAO2) seen in the elderly and during general anesthesia.
a. When a region of the lung is kept below its CC, the loss in volume will eventually lead to atelectasis as the gas trapped in the alveoli is absorbed.
b. An important goal in the perioperative period is restoring the balance between FRC and CC. Because CC cannot be changed, this involves improving FRC by a variety of techniques to improve the mechanical advantage of the chest wall (adequate reversal of neuromuscular blockers, upright positioning, regional analgesia, and possibly the use of positive end-expiratory pressure [PEEP] or continuous positive airway pressure [CPAP]).
c. When positive pressure is applied during expiration to the airway of a patient who is having positive pressure ventilation, this applied airway pressure is referred to as PEEP. When a patient is breathing spontaneously, an applied airway pressure is referred to as CPAP.
C. Compliance is the change in lung volume for a given change in airway pressure. It is the reciprocal of “elastance.” Monitoring changes in respiratory compliance is extremely important in ventilated patients as an early warning of changes in the lung or chest–abdominal wall complex that may negatively affect gas exchange.
D. Resistance in the respiratory system is important because, in the perioperative period, complications such as bronchospasm or secretions in an endotracheal tube or partial circuit obstruction will present primarily as increased resistance.
E. Work of breathing is commonly used to denote the ongoing energy expenditure required by the respiratory system. During normal quiet breathing, expiration is passive and does not require work.
1. The oxygen requirement for the work of breathing is less than 2% of the normal basal oxygen consumption (3 to 4 mL/kg/minute).
2. In patients with COPD due to the mechanical inefficiency of the respiratory system, increasing the minute ventilation to 20 L per minute may increase the oxygen consumption of the muscles of respiration to levels of 200 mL per minute.
F. Respiratory fatigue may occur at any point from the central nervous system (CNS) to the muscles of respiration (diaphragm is possibly the most fatigue-resistant skeletal muscle and can sustain resistive loads of up to 40% of maximal indefinitely).
1. Because the oxygen supply requirement for the diaphragm is high in proportion to its mass, it is susceptible to hypoxia either due to decreased oxygen content of the arterial blood or due to decreased cardiac output.
2. The diaphragm can be rested for a short period by mechanical ventilation but histologic evidence of muscle fiber atrophy can be seen after as little as 18 hours of mechanical ventilation and clinical evidence of weakness is seen within days.
VI. Distribution of Ventilation
A. Pulmonary circulation is composed of the pulmonary circulation from the main pulmonary artery and the smaller bronchial circulation arising from the aorta. The pulmonary circulation dominates, by volume, and serves to deliver the mixed venous blood to the alveolar capillaries to facilitate gas exchange and to act as a large, low-resistance reservoir for the entire cardiac output from the right ventricle. The bronchial circulation serves to provide nutritional support to the airways and their associated pulmonary blood vessels.
B. Pulmonary Hemodynamics
1. Despite receiving all of the cardiac output from the right ventricle, the pulmonary vasculature maintains a relatively low pulmonary blood pressure. The normal adult mean pulmonary artery pressure (PPA) is 9 to 16 mm Hg with systolic PPA of 18 to 25 mm Hg.
2. PVR can change as a result of numerous factors (hypoxia, acidosis, mitral valve stenosis or regurgitation, left ventricular failure, primary pulmonary hypertension, or pulmonary emboli).
C. Distribution of Perfusion. There is a gradient of distribution of perfusion of the lung that is similar but not identical to the gradient of distribution of ventilation, with increased perfusion of regions in the central and lower regions compared to the upper regions (Fig. 24-8). Gravity, posture, and alveolar pressure will also have effects on the distribution of pulmonary blood flow.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


