Follicular Lymphoma
Roberto N. Miranda, MD
Key Facts
Terminology
Follicular lymphoma (FL)
Etiology/Pathogenesis
Bcl-2 overexpression is present in most cases of FL
Results from t(14;18)(q32;q21)/IgH–BCL2
Other factors are involved in pathogenesis
Clinical Issues
Most cases of FL involving spleen are manifestation of systemic disease
FL in spleen is commonly diagnosed by splenectomy
Performed for cytopenias or abdominal pain/discomfort
Splenectomy is rarely performed for diagnostic purposes
FL is mostly clinically indolent disease
Microscopic Pathology
Common patterns of involvement
Miliary pattern growing along preexisting follicles
Nodular effacement of architecture
Neoplastic follicles are composed of centrocytes and centroblasts
Ancillary Tests
Immunophenotype
Monotypic Ig(+), CD19(+), CD20(+)
CD10(+) and Bcl-6(+) in most cases
Cytogenetics/molecular
t(14;18)(q32;q21)/BCL2-IgH in ˜ 80-90% of cases
Top Differential Diagnoses
Splenic marginal zone lymphoma (SMZL)
Mantle cell lymphoma (MCL)
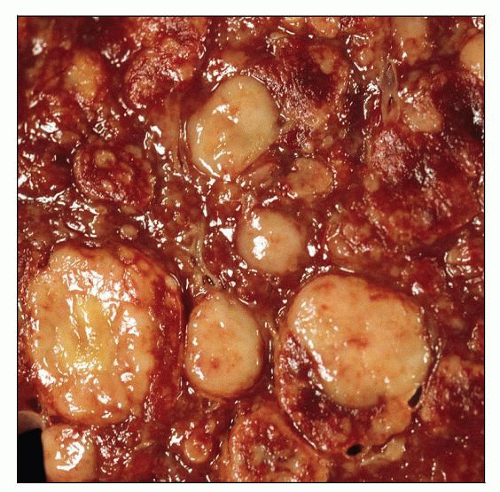
 Follicular lymphoma involving the spleen. The lymphoma has a diffuse micronodular pattern enhancing white pulp. This is the most common pattern of follicular lymphoma involving the spleen. |
TERMINOLOGY
Abbreviations
Follicular lymphoma (FL)
Synonyms
Follicular center cell lymphoma, grades 1-3 (REAL classification)
Follicular lymphoma, predominantly small cleaved cell, mixed small cleaved and large cell, or large cell (Working Formulation)
Centroblastic/centrocytic lymphoma (Kiel classification)
Nodular lymphoma, poorly differentiated, mixed, or histiocytic (Rappaport classification)
Definitions
Mature B-cell neoplasm composed of germinal (follicle) lymphocytes (centrocytes and centroblasts) in variable mixture
Histopathology usually shows follicular growth pattern; less frequently is purely diffuse
ETIOLOGY/PATHOGENESIS
Pathogenesis
Bcl-2 overexpression as result of t(14;18)(q32;q21)/IgH-BCL2 gene rearrangement
Bcl-2 inhibits programmed cell death, giving Bcl-2(+) lymphoma cells a survival advantage
Many other anti-apoptotic molecules (e.g., Bcl-x, Mcl-1, etc.)
IgH-BCL2 by itself is insufficient for lymphomagenesis
Other mechanisms are involved and needed for FL to develop
CLINICAL ISSUES
Epidemiology
Incidence
FL is 2nd most common lymphoma in Western hemisphere
FL rarely arises in spleen
Splenic involvement is usually manifestation of systemic disease
Age
Range: 30-83 years (median: 59 years)
Gender
M:F = 1:1.4
Site
Most cases of FL involving spleen are diagnosed by splenectomy
FL primarily affects lymph nodes, but also bone marrow, peripheral blood, and Waldeyer ring
FL involving extranodal sites usually reflects widespread nodal disease
Primary FL of spleen is rare
Presentation
Splenomegaly, abdominal pain, anemia, or thrombocytopenia
Usually associated with peripheral or abdominal lymphadenopathy with widespread disease
B-type symptoms in subset of patients
Laboratory Tests
˜ 30% peripheral blood lymphocytosis
Natural History
Splenectomy is not curative
May alleviate symptoms or cytopenias
Treatment
Prognosis
Usually considered an indolent lymphoma, but with frequent relapses
International Prognostic Index for Follicular Lymphoma (FLIPI) is predictor of outcome
5-year overall survival is 55-70%
Transformation to large B-cell lymphoma occurs
˜ 20% of patients with prolonged clinical follow-up
MACROSCOPIC FEATURES
General Features
Variable gross appearance
Diffuse/miliary growth pattern, predominantly involving preexisting white pulp
Single or multiple tumor masses of variable size also can be observed
Median weight: 1.1 kg (range: 0.5-2.7 kg)
MICROSCOPIC PATHOLOGY
Histologic Features
Miliary pattern growing along preexisting follicles is most common pattern
Usually associated with marginal zone pattern and less red pulp involvement
Some researchers have suggested that this pattern is a form of in situ follicular lymphoma
Associated with or without disseminated disease
Effacement of architecture is 2nd most common pattern
Follicles are packed and coalescent
Correlates with grossly visible tumor mass
Can display diffuse areas
Neoplastic follicles are composed of centrocytes and centroblasts
Variable cytologic predominance according to grade of tumor
Low grade (grades 1 and 2): Up to 15 centroblasts per high-power field on average
Grade 3: More than 15 centroblasts or immunoblasts per high-power field on average
Some high-grade cases have sparse centrocytes
Marginal zone pattern in ˜ 50% of cases
Lymphocytes acquire abundant, pale (monocytoid) cytoplasm
Typically present at periphery of neoplastic follicles
Splenic hilar lymph nodes also may show marginal zone pattern
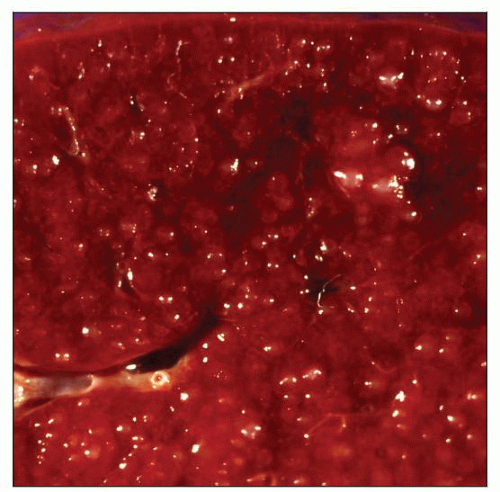
Red pulp infiltration as satellite aggregates
˜ 30% with diffuse red pulp involvement; mainly small FL lymphocytes
FL cells often appear smaller and less irregular than those in white pulp
Bone marrow biopsy specimen is involved by paratrabecular aggregates
Other patterns are often present, but rare without paratrabecular pattern
Cytologic Features
Fine needle aspiration performed uncommonly on spleen
Centrocytes and centroblasts are present in smears
Lymph Nodes
Hilar or peripheral lymph nodes usually show features similar to those in spleen
Usually follicular pattern is present
Marginal zone pattern in ˜ 10% cases
ANCILLARY TESTS
Immunohistochemistry
Positive for B-cell markers: CD19(+), CD20(+), CD79a(+), pax-5(+)
CD10(+) and Bcl-6(+) in most cases
Stronger in white pulp; weaker in red pulp or in interfollicular areas
Bcl-2 (variable [+]) in white and red pulp
Bcl-2 more frequently (+) in low-grade FL (65-90%) than in high-grade FL (50-80%)
Follicular dendritic meshworks usually present
CD21(+), CD23(+), CD35(+), &/or CNA.42(+)
T-cell antigens(−), Cyclin-D1(−)
Variable proliferation rate as determined with Ki-67
Low-grade FL usually has low proliferation rate (< 20%)
Flow Cytometry
Monotypic surface immunoglobulin(+)
Heavy chains: IgM(+) or IgG(+), and IgD(−)
IgD(+) in rim of occasional residual mantle zone lymphocytes
CD19(+), CD20(+), CD22(+), and CD79a(+)
Usually CD10(+)
Occasional downregulation of CD10 in peripheral blood and bone marrow
T-cell antigens(−)
Cytogenetics
t(14;18)(q32;q21) in ˜ 80-90%
Other cytogenetic abnormalities are found in ˜ 90% of FL and include
Losses of 1p, 6q, 10q, &/or 17p
Gains of 1, 6p, 7, 8, 12q, X, &/or 18q
In Situ Hybridization
BCL2-IgH gene rearrangements can be demonstrated in almost all cases using fusion probes and FISH
Probes used are quite large and cover relevant regions of chromosomes 14 and 18
BCL6 translocations in ˜ 10% of cases
Molecular Genetics
Monoclonal IgH gene rearrangements in 60-70% of cases
False-negative results are common
Result from presence of somatic hypermutation in IgH variable region genes
BCL2-IgH gene rearrangements can be demonstrated in ˜ 80% of cases
Most breakpoints in BCL2 on chromosome 18 occur on MBR (major breakpoint region)
Other minor breakpoints: Mcr (minor cluster region), icr (intermediate cluster region), etc.
PCR assays can sensitively detect most of these breakpoints
FISH assays, unlike PCR, can assess all breakpoints but are less sensitive
It is important to remember that
PCR can detect BCL2-IgH fusions sequences in people without evidence of FL
Frequency of (+) result correlates with increasing age
This finding suggests that other molecular mechanisms are required for lymphomagenesis
P53 gene mutations associated with transformation to high-grade lymphoma
DIFFERENTIAL DIAGNOSIS
Splenic Marginal Zone Lymphoma (SMZL)
Micronodular infiltrate of white pulp centered on preexisting follicles
Low-power magnification shows darker inner zone surrounded by paler marginal zone (biphasic pattern)
Residual germinal centers or mantle zones (−/+); usually not present
Red pulp involvement usually as small aggregates
Neoplastic cells are predominantly small with abundant pale cytoplasm, round nuclei, and small nucleoli
Scattered large cells always present
Plasmacytic differentiation is common; can be marked
Subset of cases associated with serum paraprotein; can be high level
Proposed variant of SMZL diffusely involves red pulp of spleen
Splenic hilar lymph nodes often show
Incomplete effacement with preservation of some sinuses
Marginal zone pattern that can colonize follicles and mimic FL
Peripheral blood lymphocytes characterized by unipolar cytoplasmic projections (villous lymphocytes)
Subset of patients can present with marked lymphocytosis (˜ 100 K)
Bone marrow shows intertrabecular and sometimes paratrabecular lymphoid aggregates
Sinusoidal pattern of involvement in ˜ 33-50% of patients
Immunophenotype
IgM(+), IgD(+/−), CD19(+), CD20(bright [+]), CD22(bright [+])
CD11c(+), FMC7(+), CD5(−/+), CD10(−), Bcl-6(−)
Mantle Cell Lymphoma (MCL)
Micronodular infiltrate of white pulp
Small nodules or aggregates throughout red pulp
Lymphocytes are uniform, intermediate in size, usually with irregular nuclear contours
Immunophenotype
IgM(+), IgD(+), CD5(+), CD19(+), CD20(+), Cyclin-D1(+)
CD10(−), CD23([-/+] dim), CD43([+/-], dim), Bcl-6(−)
Detection of t(11;14)(q13;q32)/CCND1-IgH is very helpful
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree