Follicular Dendritic Cell Sarcoma
Sa A. Wang, MD
Key Facts
Terminology
Neoplastic proliferation of follicular dendritic cells
Clinical Issues
Presents as slow-growing, painless mass
Lymph nodes
Extranodal sites; Waldeyer ring common
Most cases behave like low- to intermediate-grade soft tissue sarcoma
Local excision, frequent recurrence
Insensitive to chemotherapy
Subset of cases are clinically aggressive
Microscopic Pathology
Spindled to ovoid cells forming fascicles, storiform arrays, whorls, diffuse sheets, or vague nodules
Morphologic variants
Spindled/typical, epithelioid
Inflammatory pseudotumor-like variant
High-grade features correlate with aggressive clinical course
Ancillary Tests
Immunophenotype
Variable expression of CD21, CD23, CD35, CXCL13, clusterin, or EGFR
Electron microscopy
Well-formed desmosomes
Top Differential Diagnoses
Interdigitating dendritic cell sarcoma
Langerhans cell histiocytosis/sarcoma
Inflammatory myofibroblastic tumor
Diffuse large B-cell lymphoma
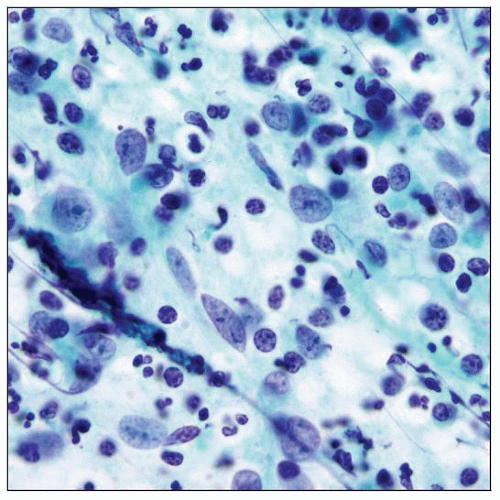
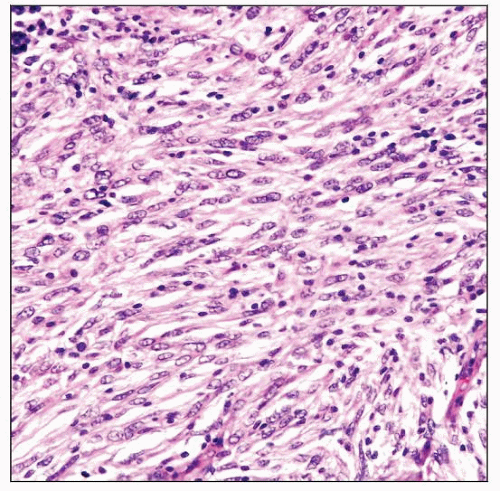 Lymph node involved by follicular dendritic cell (FDC) sarcoma. The neoplastic cells have indistinct cell borders, a moderate amount of eosinophilic cytoplasm, and oval or elongated bland nuclei. |
TERMINOLOGY
Abbreviations
Follicular dendritic cell (FDC) sarcoma
Synonyms
FDC tumor
Dendritic reticulum cell sarcoma
Definitions
Neoplastic proliferation of follicular dendritic cells
Immunophenotype supports FDC lineage
ETIOLOGY/PATHOGENESIS
Normal FDCs
Localized to B-cell areas in primary and secondary lymphoid follicles
Form a meshwork via cell to cell attachments and desmosomes
Do not migrate
Trap and present antigens to B cells that are involved in B-cell proliferation and differentiation
Store antigen on cell surface as immune complexes
Closely related to bone marrow stromal progenitors
Have features of myofibroblasts
Etiology of FDC Sarcoma
Unknown in most cases
Small subset of cases of FDC sarcoma are associated with Castleman disease (CD)
Hyaline-vascular variant
FDC “dysplasia” has been reported in hyaline-vascular CD
Inflammatory pseudotumor-like variant of FDC sarcoma
Consistently associated with Epstein-Barr virus (EBV)
EBV is present in monoclonal form
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Adults; median age: 40-50 years
Gender
Overall, no gender preference
Inflammatory pseudotumor-like variant shows female predominance
Ethnicity
No known predisposition
Presentation
Often presents as slow-growing, painless mass
Lymph nodes
Cervical lymphadenopathy is most common
Other lymph node groups: Axillary, mediastinal, mesenteric, and retroperitoneal may or may not present
Extranodal sites
Waldeyer ring is most common, such as tonsil, oral cavity
Gastrointestinal tract
Soft tissue, skin
Thyroid, breast, mediastinum
Liver and spleen
Inflammatory pseudotumor-like variant FDC sarcoma
Often arises in intraabdominal sites: Liver, spleen, and peripancreatic area
Systemic symptoms
Uncommon in most patients with FDC sarcoma
Systemic symptoms are common in patients with inflammatory pseudotumor-like variant
Weight loss and fever
Paraneoplastic pemphigus can occur rarely
Treatment
Most patients are treated by complete surgical excision
With or without adjuvant radiotherapy or chemotherapy
Various chemotherapy regimens have been used with limited success
Adjuvant radiotherapy may prolong disease-free survival
Prognosis
Most cases behave like low- to intermediate-grade soft tissue sarcoma
Local recurrences occur in > 50% of patients
Metastases occur in ˜ 25% of patients
Lymph nodes, lung, liver
10-20% of patients ultimately die of the disease after many years
Poor prognostic indicators
Large tumor size (> 6 cm)
Intraabdominal location
Often in liver, spleen, or peripancreatic or retroperitoneal lymph nodes
Inflammatory pseudotumor-like variant of FDC sarcoma is more indolent
High-grade histologic features
IMAGE FINDINGS
General Features
FDC sarcoma cannot be distinguished from other malignant processes by imaging
CT and MR
Mass lesion, expansile
± invasion of surrounding structures
Positron emission tomography (PET) shows abnormal radiotracer uptake
MACROSCOPIC FEATURES
Size
Mean: 5 cm; range: 1-21 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Typical histologic features
Spindled to ovoid cells forming fascicles, storiform arrays, whorls, diffuse sheets, or nodules
Often admixed with small lymphocytes
Lymphocytes often aggregate around blood vessels
Many cases have low-grade cytologic features
Epithelioid variant
Oval or round nuclei and moderate amount of cytoplasm
Myxoid stroma often present
Neoplastic cells can show clear or eosinophilic (oncocytic) changes
Histologic features of high-grade FDC sarcoma
Significant cytologic atypia
Mitotic figures numerous; up to > 30/10 high-power fields
Coagulative necrosis(+)
Inflammatory pseudotumor-like variant of FDC sarcoma
Well demarcated from surrounding parenchyma
Admixture of lymphocytes, plasma cells, and histiocytes
Striking histologic resemblance to inflammatory pseudotumor or inflammatory myofibroblastic tumor
Some cases can resemble classical Hodgkin lymphoma with HRS-like cells
Center of tumor often shows hemorrhage and necrosis
Blood vessels frequently show fibrinoid deposits in walls
FDC sarcoma associated with hyaline-vascular variant of Castleman disease (CD)
Often see coexistent changes of hyaline-vascular CD
± regressed (involuted) germinal centers with hyalinization
Thick and hyalinized blood vessel walls
Vascular proliferation in interfollicular areas
Effaced lymph node sinuses
Proliferation of FDC
In large sheets, nodular or confluent
Often CXCL13(+)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree