Fibroepithelial Neoplasms
FIBROADENOMATOID MASTOPATHY (SCLEROSING LOBULAR HYPERPLASIA)
This benign proliferative lesion usually presents as a localized tumor with a mean diameter of 4 cm, but asymptomatic lesions have been detected by mammography (1,2). The most frequent mammographic finding is a well-defined mass. Microcalcifications are not commonly present. The imaging characteristics are not sufficiently specific to distinguish sclerosing lobular hyperplasia from a fibroadenoma. Patients range from ages 14 to 46 with a mean age of about 32 years (1,2).
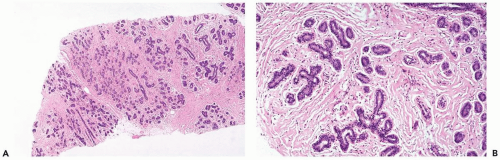
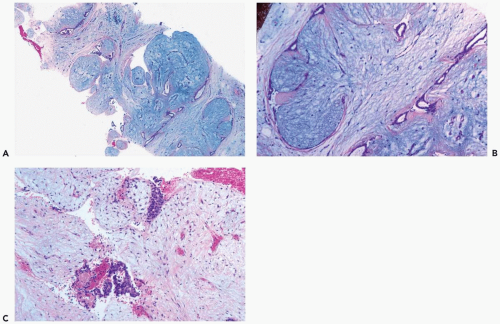
Microscopic examination reveals enlarged lobules composed of an increased number of intralobular glands (Fig. 7.1). The intralobular stroma is collagenized, and there is variable sclerosis of the interlobular stroma. Individual lobules and groups of lobules sometimes have the appearance of miniature fibroadenomas with a prominent glandular component (Fig. 7.2). Secretory activity is variably present or absent, and calcifications are not formed. Fibroadenomatoid mastopathy is found in breast tissue surrounding about 50% of fibroadenomas or phyllodes tumor (1) and in most patients who have a phyllodes tumor. Because the fibroadenoma or phyllodes tumor produces a dominant mass, associated sclerosing lobular hyperplasia may be overlooked.
FIBROADENOMA
These benign tumors arise from the epithelium and stroma of terminal duct-lobular units. They account for about one-fifth of all benign masses and approximately 10% of breast lesions in postmenopausal patients. Dupont et al. (3) found that an increased relative risk for subsequent breast carcinoma was dependent on the presence of proliferative changes in the fibroadenoma (complex fibroadenoma) itself or in the surrounding breast, and a family history of breast carcinoma.
The age distribution of fibroadenomas ranges from childhood to more than 70 years, with a mean age of about 30 and a median around 25 years (4). The most frequent presenting symptom is a self-detected painless, firm, well-circumscribed solitary tumor. A growing proportion of fibroadenomas are nonpalpable tumors that are detected by mammography. Multiple fibroadenomas occur in about 15% of patients, with equal proportions found synchronously and metachronously in the same or opposite breast. An uncommon syndrome occurring in adolescence is the metachronous and synchronous development of multiple fibroadenomas, usually in both breasts (5). The intervening breast tissue often manifests extensive fibroadenomatoid hyperplasia.
Patients who received cyclosporin A for immunosuppression after organ transplantation are reported to be predisposed to develop fibroadenomas (6,7,8). The tumors are typically bilateral and multiple. The duration of cyclosporin A treatment prior to detection of the fibroadenomas is generally more than a year with a mean interval in one study of 4.4±1.7 years (range 1.7 to 7.1 years) (8). When compared to fibroadenomas found in control women who did not undergo transplantation or cyclosporin A treatment, cyclosporin A related tumors were significantly larger and had a lower longitudinal to anterior-posterior ratio (8).
Coarse calcifications are not uncommon in fibroadenomas after the menopause (Fig. 7.3). In one series, only 10% of fibroadenomas measured more than 4.0 cm (4). Tumors larger than 4 cm are significantly more frequent in patients age 20 or younger than in older patients (4). Fibroadenomas that involve most or all of the breast, often referred to as adolescent giant fibroadenomas, develop as solitary or multiple tumors shortly after puberty (5).
More than 90% of fibroadenomas are of the adult type, with the remainder fulfilling criteria for other unusual types of fibroadenoma. Tubular adenoma or adenofibroma is a variant of fibroadenoma composed of closely approximated round or oval glandular structures consisting of a
single layer of epithelium supported by myoepithelial cells (9). Foci with the adenofibroma pattern can be encountered within an otherwise ordinary fibroadenoma. Other so-called adenomas are unrelated to the fibroadenoma category. Apocrine adenoma is a localized nodular focus of prominent papillary and cystic apocrine metaplasia (10) (see Chapter 4). Nodular foci of sclerosing adenosis with apocrine metaplasia have been variously termed apocrine adenoma and apocrine adenosis. Ductal adenoma (11) and pleomorphic adenoma (12) are variants of intraductal papilloma or adenomyoepithelioma.
single layer of epithelium supported by myoepithelial cells (9). Foci with the adenofibroma pattern can be encountered within an otherwise ordinary fibroadenoma. Other so-called adenomas are unrelated to the fibroadenoma category. Apocrine adenoma is a localized nodular focus of prominent papillary and cystic apocrine metaplasia (10) (see Chapter 4). Nodular foci of sclerosing adenosis with apocrine metaplasia have been variously termed apocrine adenoma and apocrine adenosis. Ductal adenoma (11) and pleomorphic adenoma (12) are variants of intraductal papilloma or adenomyoepithelioma.
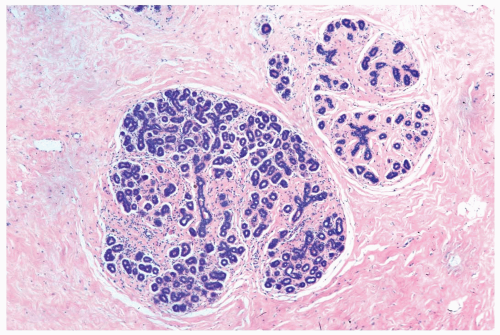
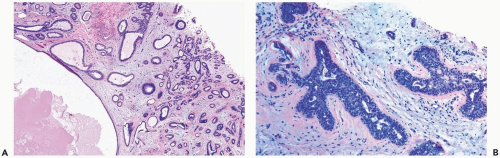
The histologic hallmark of a fibroadenoma is concurrent proliferation of glandular and stromal elements. The majority of adult fibroadenomas have growth patterns that have been referred to as intracanalicular and pericanalicular (Fig. 7.4). The former pattern is produced when the stroma compresses ducts into elongated linear branching structures with slit-shaped lumina. When the ducts are not compressed by the stroma, the architecture is described as having a pericanalicular pattern. These structural features are of no known prognostic or clinical significance, and some tumors have both components. A fibroadenoma with a prominent intracanalicular pattern may be mistaken for a benign phyllodes tumor, especially in a needle core biopsy specimen.
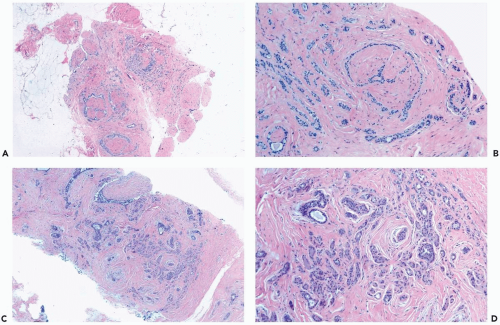
The appearance of the stroma varies from one fibroadenoma to another, but it is relatively homogeneous in any given lesion. The average fibroadenoma in adults has evenly distributed similar proportions of epithelium and stroma throughout the tumor. The density of stromal cellularity is not related to tumor size. Fibroadenomas from women less than age 20 tend to have more proliferative epithelium and more cellular stroma as a group than tumors from women older than 45 years. (Fig. 7.5). Mitotic figures are very unusual in fibroadenomatous stroma.
Uncommon types of stroma encountered in fibroadenomas include smooth muscle metaplasia, usually derived from myoid metaplasia of myoepithelial cells in sclerosing adenosis or myofibroblasts in the fibroadenoma (13) and adipose differentiation (14). Giant cells, sometimes with multiple hyperchromatic nuclei, are found in the stroma of fibroadenomas as well as in cystosarcomas (15) and in other benign tumors (16). These cells do not influence the clinical course of the lesion. A tumor that has the structural features of a fibroadenoma should not be classified as a cystosarcoma solely because the stroma contains a few multinucleated giant cells. Osteochondroid metaplasia is very uncommon and almost always occurs in fibroadenomas from postmenopausal women (17). The stroma of a fibroadenoma can undergo marked myxoid change, and, in extreme cases, the needle core biopsy specimen from such a tumor could be mistaken for mucinous carcinoma (Fig. 7.6).
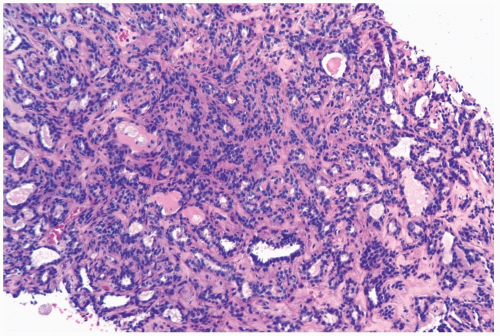
Squamous metaplasia, cysts, duct hyperplasia, adenosis, and apocrine metaplasia (Fig. 7.7) can develop in the epithelial component of a fibroadenoma. Sclerosing adenosis in a fibroadenoma can be mistaken for infiltrating
carcinoma (Fig. 7.8), and it can develop calcifications (Fig. 7.9). Fibroadenomas with adenosis, papillary apocrine hyperplasia, cysts, or epithelial calcifications have been designated “complex” (3). A review of 396 fibroadenomas from a single institution revealed “complex histologic features” in 40.4% of the tumors. These patients tended to be older than women whose fibroadenomas were not complex (18). Marked epithelial hyperplasia can be encountered in a complex fibroadenoma (Fig. 7.10). These proliferative changes are not dependent on exposure to exogenous hormones (19). Estrogen receptor activity is largely localized in the epithelium of fibroadenomas when examined by immunohistochemistry, whereas progesterone receptor is reportedly localized in the stroma as well as in the epithelium (20,21). Secretory hyperplasia sometimes occurs diffusely in fibroadenomas during pregnancy. Fibroadenomas with secretory hyperplasia should be distinguished from the tumor commonly referred to as lactating adenoma, which is a compact aggregate of lobules exhibiting secretory hyperplasia. Ultrasonography of lactating adenomas reveals one or more hypoechoic, well-defined masses (22).
carcinoma (Fig. 7.8), and it can develop calcifications (Fig. 7.9). Fibroadenomas with adenosis, papillary apocrine hyperplasia, cysts, or epithelial calcifications have been designated “complex” (3). A review of 396 fibroadenomas from a single institution revealed “complex histologic features” in 40.4% of the tumors. These patients tended to be older than women whose fibroadenomas were not complex (18). Marked epithelial hyperplasia can be encountered in a complex fibroadenoma (Fig. 7.10). These proliferative changes are not dependent on exposure to exogenous hormones (19). Estrogen receptor activity is largely localized in the epithelium of fibroadenomas when examined by immunohistochemistry, whereas progesterone receptor is reportedly localized in the stroma as well as in the epithelium (20,21). Secretory hyperplasia sometimes occurs diffusely in fibroadenomas during pregnancy. Fibroadenomas with secretory hyperplasia should be distinguished from the tumor commonly referred to as lactating adenoma, which is a compact aggregate of lobules exhibiting secretory hyperplasia. Ultrasonography of lactating adenomas reveals one or more hypoechoic, well-defined masses (22).
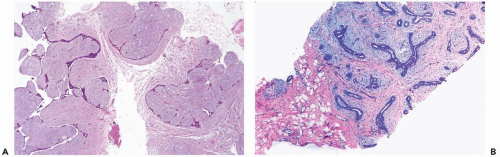
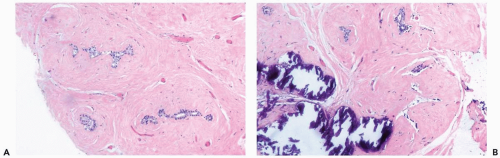 Figure 7.3 Fibroadenoma with sclerosis and calcification. A, B. This needle core biopsy specimen is from a nonpalpable, calcified lesion in a 74-year-old woman. |
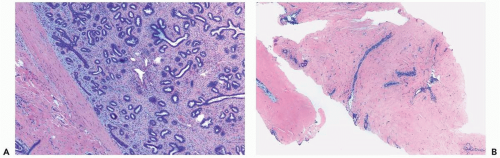
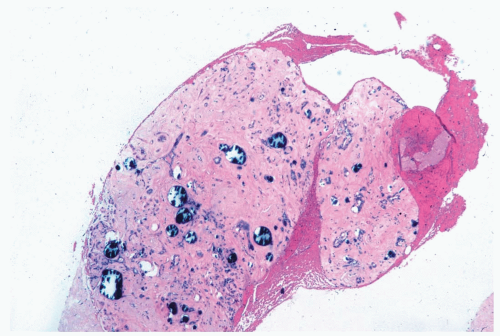 Figure 7.9 Complex fibroadenoma with sclerosing adenosis and calcifications. The needle core biopsy specimen contained this tissue fragment. The excised tumor was a very sclerotic fibroadenoma. |
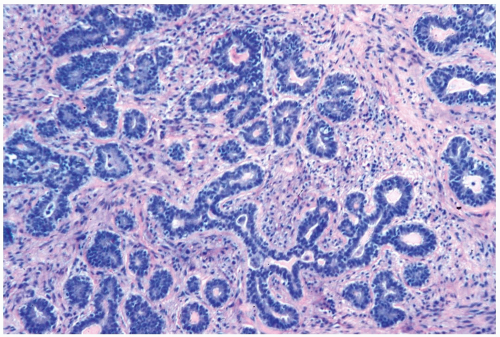 Figure 7.11 Juvenile fibroadenoma. The lesion features a balanced proliferation of glands and stroma. |
Juvenile fibroadenomas account for about 4% of all fibroadenomas with the majority of the patients under age 20 (23). Tumors with the histologic features of juvenile fibroadenoma have been found in adult women as old as age 72 (24




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree