Fenestration or Enucleation of Hepatic Cystic Disease
Purvi Y. Parikh
DEFINITION
Fenestration is defined as the removal of the free wall of a hepatic cystic lesion with the intent of forming a permanent communication between the residual cyst cavity and the peritoneal cavity. Thus, the procedure allows for any secreted fluid subsequently produced by the cyst lining to be absorbed by the peritoneum.
Enucleation involves removal of the cyst in toto without spillage of contents; the intent is to use the capsule of the cyst as a resection plane to preserve hepatic parenchyma.
DIFFERENTIAL DIAGNOSIS
Common cystic lesions range from the single, simple, small liver cyst to polycystic liver disease.
More uncommon lesions are mesenchymal hamartomas, biliary hamartomas, and ciliated foregut hepatic cysts.
Parasitic infection of the hepatic cyst must be ruled out prior to proceeding with surgery. Serology and characteristic imaging features make this determination straightforward.
Biliary cystadenomas/cystadenocarcinomas that have malignant potential require enucleation rather than fenestration. The identification of bile in the cyst is the most important factor in identifying cysts with malignant potential that warrant the increased morbidity of enucleation.
PATIENT HISTORY AND PHYSICAL FINDINGS
Most simple hepatic cysts are asymptomatic and detected as an incidental finding during imaging of the abdomen.
Simple hepatic cysts are congenital lesions, which are progressive dilatations of biliary microhamartomas known as von Meyenburg’s complexes. Such cysts are lined by flattened biliary epithelium without a separation from adjacent hepatic parenchyma. They do not communicate with the biliary tree. These cysts contain serous fluid, which is continuously excreted by thin lining of epithelial cells.
The prevalence of hepatic cysts is 16% to 18%. Females are affected more frequently than males.
The frequency increases with age, with the peak incidence between ages 50 and 60 years.
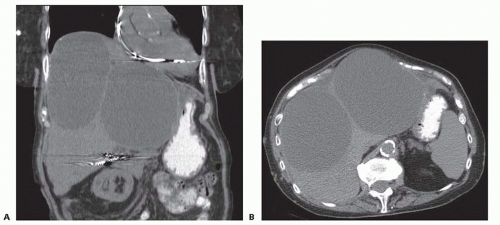
Large cysts may exert a mass effect and cause upper abdominal discomfort and early satiety (FIG 1).
Symptoms are more common with right-sided cysts.
Ultrasound-guided percutaneous cyst aspiration has minimal role in treatment of symptomatic cysts, as the recurrence rate is high and as rapid as 2 weeks.
If symptoms persist after needle aspiration, the cyst is not the likely cause and other diagnoses should be investigated.
Alternatively, if symptoms resolve after aspiration and return with recurrence of the cyst, definitive treatment of the cyst is indicated.
Indications for intervention include pain, jaundice, infection, and hemorrhage. Occasionally, compression results in portal hypertension and indicates resection is appropriate.
Most cysts that are incidentally identified do not warrant resection, provided the cyst lacks features of malignant potential. These features include septations; heterogenous attenuation; and a thickened, enhancing cyst wall.
Complications are rare but include intracystic hemorrhage, biliary obstruction due to compression, cyst rupture, and cyst torsion. Bacterial infection leading to symptoms is occasionally observed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Because most hepatic cysts are asymptomatic, they are most frequently detected on imaging of the abdomen obtained for other indications.
Laboratory tests of liver enzymes (aspartate aminotransferase [AST], alanine aminotransferase [ALT], bilirubin, alkaline phosphatase) and tumor markers (carcinoembryonic antigen [CEA], carbohydrate antigen 19-9 [CA 19-9]) and serologies (hydatid)
Ultrasound scanning demonstrates a rounded, anechoic intrahepatic mass with good thorough transmission and an imperceptible wall.
Computed tomography shows a benign hepatic cyst as a homogenous lesion of low attenuation with no enhancement of the wall or content following administration of contrast.
Magnetic resonance scanning diagnostic criteria are a homogenous lesion with low attenuation in T1 weighted images and a very high-signal intensity on T2 weighted images.
Importantly, neuroendocrine and sarcoma hepatic metastases occasionally appear cystic.
TECHNIQUES
FENESTRATION
Preoperative Planning
Prior to operation, the patient should be counseled regarding the pros and cons of laparoscopic versus open surgery.
Although the risk of infection after liver surgery is low, antibiotic prophylaxis significantly reduces the risk of postoperative infection.
Laparoscopic Fenestration
Laparoscopic cyst fenestration has evolved to be the firstline surgical approach for symptomatic cysts.
Port placement. A three-port laparoscopic technique is used (FIG 2): camera (30 or 45 degree), grasper for the cyst wall, and cutting instrument (cautery, Harmonic scalpel, or scissors). One of the ports should be 10 mm for clip application.
Grasping of cyst. The cyst can be elevated with a grasper once it has been punctured through the exposed wall immediately adjacent to the liver parenchyma by insertion of a cutting instrument. The contents are drained and sent for analysis (FIG 3).
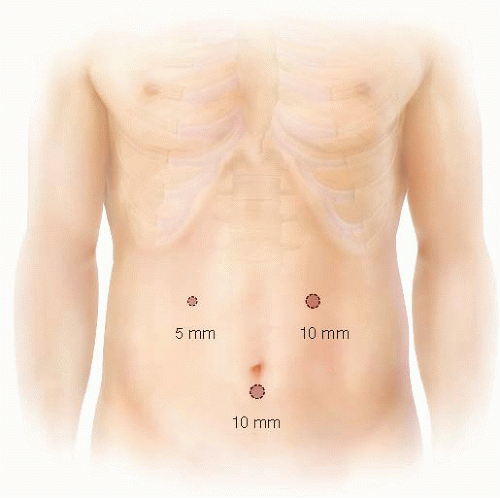
FIG 2 • Trocar placement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access