http://evolve.elsevier.com/Edmunds/NP/
Eye Agents
A great many products are available for the eye. Drugs selected for inclusion here are those seen most commonly, and only one representative drug has been chosen for many categories. The drugs featured in this chapter have a wide variety of diagnostic and therapeutic uses. The two eye diseases most commonly seen in primary care that are treated medically are infectious conjunctivitis and seasonal allergic conjunctivitis. Most eye conditions require referral to an ophthalmologist.
Therapeutic Overview of Eye Agents
Anatomy, Physiology, and Pathophysiology
The eye is protected by the tear film, which covers the cornea and conjunctiva, up to the lid margins; it provides moisture, lubrication, oxygen, and protective chemicals, including cytokines. Tears are regularly distributed over the lens by blinking of the eyelid. Tears drain through the puncta at the lid margins (Figure 14-1), into the lacrimal ducts and sac, then to the nasolacrimal duct and to the nose. Medications in the tears may be systemically absorbed through the nasal and pharyngeal mucosa.
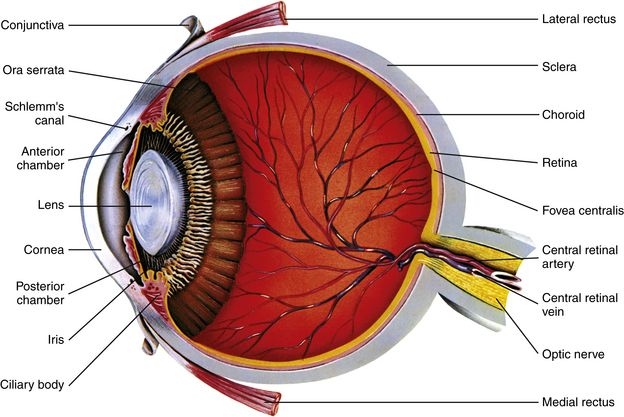
FIGURE 14-1 Lacrimal apparatus.
Tears drain through the puncta at the lid margins, into the lacrimal ducts and sac, then to the nasolacrimal duct and to the nose. (From Thibodeau GA, Patton KT: Anatomy & physiology, ed 7, St Louis, 2010, Mosby.)
Figure 14-2 shows the internal anatomy of the eye. The conjunctiva covers the inside of the eyelids and the cornea. Aqueous humor is produced by the ciliary body. Excess humor drains through the canals of Schlemm in the trabecular meshwork.
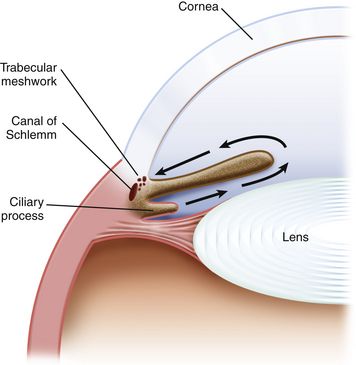
FIGURE 14-2 Internal anatomy of the eye. (From Cote, Lerman, Todres: A Practice of Anethesia for Infants and Children, ed 4, Philadelphia, 2009, Saunders.)
In glaucoma, the intraocular pressure (IOP) is too high, causing injury and death of nerve cells. Reducing the IOP can arrest the progression of the disease. Open-angle glaucoma involves no mechanical obstruction to outflow. In narrow-angle glaucoma, the iris mechanically obstructs outflow.
Disease Process
Conjunctivitis is the most common eye disease. Conjunctivitis can be caused by bacteria, virus, or allergy.
Bacterial Conjunctivitis: Bacterial conjunctivitis is most often caused by Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Pseudomonas species, and Moraxella species. Gram-negative infections are less common than gram-positive infections. Haemophilus is common in children. Chlamydial infection is an important cause of blindness. Bacterial conjunctivitis is often accompanied by large amounts of purulent discharge. Some minor pain may occur, but no changes in vision have been reported. Bacterial conjunctivitis is spread through contact.
Viral Conjunctivitis: Viral conjunctivitis is by far the most common cause of conjunctivitis. It is usually caused by adenovirus type 3, which is commonly called pink eye in children, and is extremely contagious; it is spread by touching infected secretions. Duration is from several days to 3 weeks or longer. The eye can be very painful, and pharyngitis, fever, malaise, and preauricular adenopathy may be associated. The conjunctiva is red with large amounts of clear discharge.
Herpes zoster conjunctivitis usually affects one eye. It is usually accompanied by a vesicular rash distributed along the ophthalmic division of the trigeminal cranial nerve.
Allergic Conjunctivitis: Allergic conjunctivitis is a common problem for patients with allergies. It is often seasonal but may occur year round with allergies to dust or mold. It presents with itching and tearing and is characterized by “cobblestone” papillae on the upper tarsal conjunctiva.
Glaucoma: Glaucoma is another condition that is managed by the ophthalmologist. It is common for a patient to be on two or more medications for glaucoma. The primary care provider must be aware of the possible systemic side effects of eye drops and potential drug interactions.
Other Eye Problems
Treatment Principles
Cardinal Points of Treatment
Effective treatment demands accurate diagnosis. Primary care providers collect pertinent information and begin the process of diagnosis. However, many problems require referral to a specialist for care. See Table 14-1 for evaluation and management of potentially serious eye problems.
Ophthalmic solutions are absorbed systemically, and this may pose secondary problems. In general, any adverse reaction that a medication may cause when taken orally can occur when the medication is given as an eye drop. Patient factors that increase systemic absorption include lax eyelids and hyperemic or diseased eyes. Absorption is more of a problem in infants and in the elderly than in other individuals. The formulation affects absorption by determining the amount of time the medication stays in contact with the conjunctiva. Ointments are more completely absorbed than suspensions, and suspensions are more completely absorbed than solutions. Minimize systemic absorption of ophthalmic drops by compressing the lacrimal sac for 3 to 5 minutes after instillation. This retards the passage of drops to other areas of absorption.
Eye drops must be used properly to be effective. One drop of medication is all the eye can retain. Using two drops is wasteful. If more than one drop is used, wait 5 minutes before applying the second drop. Do not use eyecups because of the risk of contamination. See the section on patient education for instructions on how to administer eye medication.
Bacterial Conjunctivitis: Topical ocular antiinfectives are used to treat external bacterial infections of the eye and its adnexa, such as conjunctivitis, corneal ulcer, dacryocystitis, and hordeolum. The usual course of treatment is 3 to 5 days, but treatment may be extended to 7 days. Generally treat both eyes if the patient has infectious conjunctivitis. Most antibiotics are effective; the least expensive broad-spectrum agent is usually the preferred treatment. Sulfacetamide sodium, instilled three or four times a day, usually is considered for first-line treatment. If the patient is allergic to sulfa, select another medication that is active against gram-positive bacteria, such as erythromycin. Neosporin is limited by the frequency of allergy to neomycin. The use of topical fluoroquinolones is discouraged by some writers. Gonococcal and chlamydial conjunctivitis are usually treated with systemic antibiotics. See Chapter 58.
Allergic Conjunctivitis: Any allergic rhinitis should be treated appropriately first, unless the ocular symptoms are severe. Systemic antihistamines may be useful. Intranasal corticosteroid sprays are also effective. If ocular symptoms persist after allergies are adequately controlled, consider local treatment. First-line treatment is a topical histamine, receptor antagonist, or a nonsteroidal antiinflammatory agent. Topical mast cell stabilizers have a slower onset of action but are good for long-term treatment. Optical nonsteroidal antiinflammatory drugs are less effective than the antihistamines. Topical ophthalmic decongestants are not drugs of choice because of their short duration of action and adverse effects, including burning, stinging, and rebound hyperemia. Systemic antihistamines may be useful. Severe allergic conjunctivitis may require topical corticosteroids, as a last resort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 Anesthetics generally are used only by ophthalmologists. If a patient is using them, he must use great care to avoid injuring the eye.
Anesthetics generally are used only by ophthalmologists. If a patient is using them, he must use great care to avoid injuring the eye.
 Prolonged use of topical antibiotics may result in overgrowth of nonsusceptible organisms, including fungi. Ophthalmic ointments may retard corneal wound healing.
Prolonged use of topical antibiotics may result in overgrowth of nonsusceptible organisms, including fungi. Ophthalmic ointments may retard corneal wound healing. Primary care providers should not prescribe steroid eye drops. Steroids should be ordered only after an ophthalmologist has examined the eye with a slit lamp.
Primary care providers should not prescribe steroid eye drops. Steroids should be ordered only after an ophthalmologist has examined the eye with a slit lamp.