Eye Disorders
INTRODUCTION
Vision, the most complex sense, has been the focus of significant medical and surgical innovations. Disorders that affect the eye can lead to vision loss or impairment; routine ophthalmic examinations and early treatment can help prevent it.
REVIEW OF ANATOMY
The visual system consists mainly of the eyeball, optic nerves, extraocular muscles, cranial nerves, blood vessels, orbital fat, and lacrimal system, which are all housed within the bony orbit, and the eyelid, which covers the eye, moistens it, and protects it from injury.
The orbit (also called the socket) encloses the eye in a protective recess in the skull. Its seven bones—frontal, sphenoid, zygomatic, maxillary, palatine, ethmoid, and lacrimal—form a cone. The apex of this cone points toward the brain, and the cone’s base forms the orbital rim.
Extraocular muscles hold the eyes in place and control their movement, as described below:
superior rectus: elevates the eye upward; adducts and rotates the eye inward
inferior rectus: depresses the eye downward; adducts and rotates the eye outward
lateral rectus: abducts or turns the eye outward (laterally)
medial rectus: adducts or turns the eye inward (medially)
superior oblique: rotates the eye inward; abducts and depresses the eye
inferior oblique: rotates the eye outward; abducts and elevates the eye
The actions of these muscles are mutually antagonistic: As one contracts, its opposing muscle relaxes.
Eye structure and activity change with age. The eyes set deeper in their sockets and the eyelids lose their elasticity, allowing the orbital fat to protrude forward. Eyelids appear more saggy and wrinkled.
OCULAR LAYERS
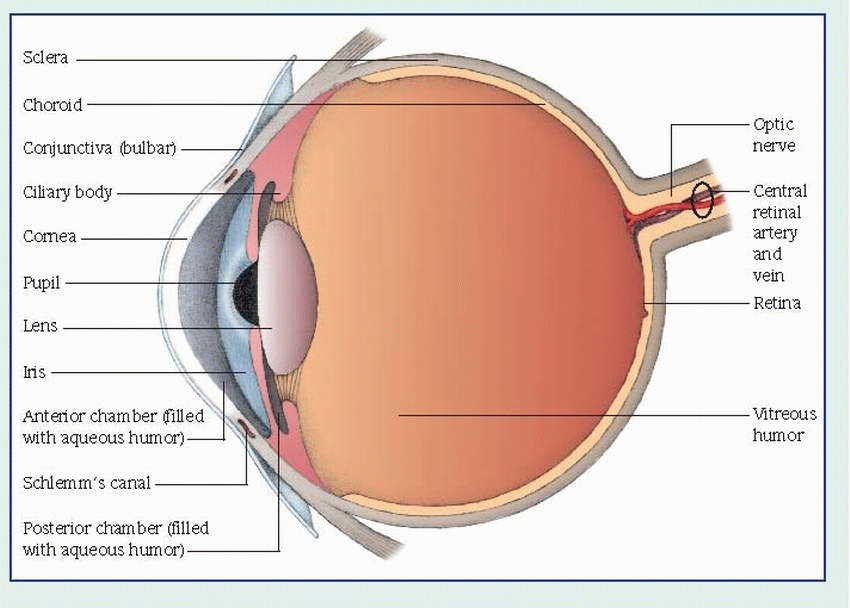
The eye has three structural layers: the sclera and cornea, the uveal tract, and the retina. (See Cross section of the eye.)
The sclera is the dense, white, fibrous outer protective coat of the eye. It meets the cornea at the limbus (corneoscleral junction) anteriorly and the dural sheath of the optic nerve posteriorly. The lamina cribrosa is a sievelike structure composed of a few strands of scleral tissue through which the optic nerve bundles pass. The sclera is covered by the episclera, a thin layer of fine elastic tissue.
In older adults, lens changes occur typically with formation of a cataract. The vitreous body liquefies and pulls away from the retina, generating floating vitreous debris and peripheral vitreous detachments.
The cornea is the transparent, avascular, dome-shaped layer of the eye that’s continuous with the sclera. The cornea consists of five layers: the epithelium, which contains sensory nerves; Bowman’s membrane, the basement membrane for the epithelial cells; the stroma, or supporting tissue (90% of the corneal structure); Descemet’s membrane, containing many elastic fibers; and the endothelium, a single layer of cells that acts as a pump to maintain proper dehydration or detumescence of the cornea. Aqueous humor bathes the posterior surface of the cornea, providing it with nutrients, and maintaining intraocular pressure (IOP) by volume and rate of outflow. The anterior cornea is kept moist by the tear film.
Dry eye syndrome is more common in the elderly. Certain medications, such as histamines, some antidepressants, and antihypertensives, as well as systemic conditions (such as menopause, diabetes, and thyroid disorders), can exacerbate dry eyes, which may result in decreased vision, eye redness, and discomfort.
The middle layer of the eye, the uveal tract, is pigmented and vascular. It consists of the iris and the ciliary body in the anterior portion and the choroid in the posterior portion. In the center of the iris is the pupil. The sphincter and dilator muscles control the amount of light that enters the eye by changing the size of the pupil.
It is believed that atrophy of the dilator muscle fibers and increased rigidity of the blood vessels of the iris reduces pupil size, decreasing the amount of light that reaches the retina. Consequently, higher levels of illumination may be needed to improve uncorrected visual acuity in the older adult.
The angle formed by the anterior iris surface and the posterior corneal structures contains many minute collecting channels of the trabecular meshwork. Aqueous humor drains through these channels into an encircling venous system called the canal of Schlemm.
The ciliary body, which extends from the root of the iris to the peripheral retina, produces aqueous humor and controls lens accommodation through its action on the zonular fibers. The choroid, the largest part of the uveal tract, is made up of blood vessels bound
externally by the suprachoroid and internally by the retina.
externally by the suprachoroid and internally by the retina.
The retina is the innermost coat of the eye. It receives visual images in the form of light and converts the images into neural impulses. The photoreceptor cells (rods and cones) are the light-sensitive cells. These and other retina cell types are interconnected by synapses and organized in layers that transmit the neural signals to the brain. Although both rods and cones are light receptors, they respond to light differently. Rods, scattered throughout the retina, respond to low levels of light and detect moving objects; cones, located in the fovea centralis, function best in brighter light and perceive finer details.
Three types of cones contain different visual pigments and react to specific light wavelengths: one type reacts to red light, one to green, and one to blue-violet. The eye mixes these colors into various shades.
Many elderly patients lose their ability to discriminate blue-greens, and white objects appear yellowish; these patients may also have difficulty discriminating among pastels, violets, and yellow-greens. The retinal pigmented epithelium (RPE) layer, which is just posterior to the photoreceptors, has multiple support functions, including phagocytosis of photoreceptor segments, vitamin A metabolism, and regulation of molecule transport to the retina.
THE LENS AND ACCOMMODATION
The lens of the eye is biconvex, avascular, and transparent; the lens capsule is a semipermeable membrane that encloses the lens and allows water and nutrients to reach the lens cells. The lens changes shape (accommodation) for near and far vision. For near vision, the ciliary body contracts and relaxes the zonules, the lens becomes spherical, the pupil constricts, and the eyes converge; for far vision, the ciliary body relaxes, the zonules tighten, the lens becomes flatter, the eyes straighten, and the pupils dilate. The lens refines the refraction necessary to focus a clear image on the retina.
The vitreous body, which is 99% water and a small amount of insoluble protein, constitutes two thirds of the eye’s volume. This transparent, gelatinous body gives the eye its shape and contributes to the refraction of light rays. The vitreous is firmly attached to the peripheral retina near the ciliary body (anteriorly) and to the optic disk (posteriorly). The vitreous face contacts the lens; the vitreous gel rests against the retina.
LACRIMAL APPARATUS AND EYELIDS
The lacrimal apparatus consists of the lacrimal glands, upper and lower canaliculi, lacrimal sac, and nasolacrimal duct. The main gland, located in a shallow fossa beneath the superior temporal orbital rim, secretes reflex tears. Small lacrimal glands throughout the conjunctiva are responsible for basal tear production. Multiple sebaceous glands in the eyelids produce an oily secretion that prevents tears from evaporating. With every blink, the eyelids direct the flow to the inner canthus, where the tears pool and then drain through a tiny opening called the punctum. The tears then pass through the canaliculi and lacrimal sac and down the nasolacrimal duct, which opens into the nasal cavity. The integrity of the lacriminal system is critical for moisturizing and also removing excess tears from the corneal surface.
The eyelids (palpebrae) consist of tarsal plates that are composed of dense connective tissue. The orbital septum—the fascia behind the orbicularis oculi muscle—acts as a barrier between the lids and the orbit. The levator palpebrae muscle elevates the upper lid. The eyelids contain three types of glands:
glands of Zeis—modified sebaceous glands connected to the follicles of the eyelashes
meibomian glands—sebaceous glands in the tarsal plates that secrete an oily substance as a tear film component (About 25 of these glands are found in the upper lid and about 20 in the lower lid.)
Moll’s glands—ordinary sweat glands
The conjunctiva is the thin mucous membrane that lines the eyelids (palpebral conjunctiva), folds over at the fornix, and covers the surface of the eyeball (bulbar conjunctiva). The conjunctiva produces mucin, another component of the tear film. The ophthalmic, lacrimal, and multiple anastomoses of facial arteries supply blood to the lids. The space between the open lids is the palpebral fissure; the juncture of the upper and lower lids is the canthus. The junction near the nose is called the nasal, medial, or inner canthus; the junction on the temporal side, the lateral or external canthus.
OPTIC NERVE
The optic nerve is composed of the nerve fibers (axons) that originate in the retina and synapse at the lateral geniculate nucleus in the brain. Approximately 1 million nerve axons are contained in the optic nerve. The nerve from each eye exits the eye posteriorly and courses through the orbit to the optic canal. Both nerves meet at the optic chiasm, located intracranally near the pituitary gland. In the optic chiasm, part of the nerve fibers from one eye cross to the other side, and vice versa. From the synapse at the lateral geniculate nucleus, nerves carry the visual information to the visual cortex, located in the majority of the occipital lobe of the brain. Some axons from the optic nerve synapse at other parts of the brain to regulate pupil responses, eye movements, and the sleep-wake cycle.
Age-related vision changes are usually first noticed during the fifth decade of life and may include the inability to focus, narrowing of the visual field, reduced peripheral vision, and loss of iris elasticity producing decreased response to light and dark. In addition, as people age, production of any of the three tear film components may decrease, causing dry eyes.
DEPTH PERCEPTION
In normal binocular vision, a perceived image is projected onto the two foveae. Impulses then travel along the optic pathways to the occipital cortex, which perceives a single image. However, the cortex receives two images—each from a slightly different angle—giving the images perspective and providing depth perception.
VISION TESTING
Several tests assess visual acuity and identify visual defects:
Ishihara’s test determines color blindness by using a series of plates composed of a colored background, with a letter, number, or pattern of a contrasting color located in the center of each plate. The patient with deficient color perception can’t perceive the differences in color or, consequently, the designs formed by the color contrasts.
The Snellen chart or other eye charts evaluate visual acuity. Such charts use progressively smaller letters or symbols to determine central vision on a numerical scale. A person with
normal acuity should be able to read the letters or recognize the symbols on the 20/20 line of the eye chart at a distance of 20′.
SUBJECTIVE TESTING
Several tests accomplish subjective testing of the eyes.
B-mode ultrasonography delineates retinal tumors, detachments, and vitreous hemorrhages—even in the presence of opacities of the cornea and lens. A handheld B-scanner has simplified ultrasonic examination of the eye, making it possible to perform such studies in the ophthalmologist’s office.
The cover-uncover test assesses eye muscle misalignment or tendency toward misalignment. In this test, the patient stares at a small, fixed object—first from a distance of 20′ (6.1 m) and then from 1′ (0.3 m). The examiner covers the patient’s eyes one at a time, noting any movement of the uncovered eye and the direction of any deviation. In extropria the eyes are naturally deviated outward. In the cover-uncover test, the eyes recover by moving inward to focus. The reverse is true in esotropia.
Duction test checks eye movement in all directions of gaze. While one eye is covered, the other eye follows a moving light. This test detects weakness of rotation due to muscle paralysis or structural dysfunction.
Fluorescein angiography evaluates the blood vessels in the choroid and retina after I.V. injection of fluorescein dye; images of the dyeenhanced vasculature are recorded by rapidsequence photographs of the fundus.
Goldmann’s applanation, Tonopen tonometry, and pneumonotometry all measure intraocular pressure (IOP). After instilling a local anesthetic in the patient’s eye, the examiner touches the Tonopen tonometer tip of the surface of the cornea. The IOP reading is displayed and measured in mm Hg. Applanation tonometry gauges the force required to flatten a small area of central cornea, and is the most accurate method of measuring IOP. For this test, a patient must be seated at a slit lamp and the cornea stained with fluorescein dye before the prism of the applanation tonometer touches the cornea and the examiner adjusts the controls until the two lines form an “S.”
Gonioscopy allows for direct visualization of the anterior chamber angle.
The Maddox rod test assesses muscle dysfunction; it’s especially useful in disclosing and measuring heterophoria (the tendency of the eyes to deviate). It can reveal horizontal, vertical and, especially, torsional deviations.
Ophthalmoscopy—direct ophthalmoscopy or binocular indirect ophthalmoscopy allows examination of the interior of the eye after the pupil has been dilated with a mydriatic. A light source and lenses are used by the examiner to focus on the posterior ocular structures (such as the retina and optic nerve).
Refraction tests may be performed with or without cycloplegics. In cycloplegic refraction, eyedrops weaken the accommodative power of the ciliary muscle. Lenses placed in front of the eye direct light rays onto the retina, thus focusing the image so that it can be transmitted along the visual pathway. A retinoscope may be used in the same way by directing a beam of light through the pupil onto the retina; the light’s shadow is neutralized by placing the appropriate lens in front of the eye.
Slit-lamp biomicroscopic examination allows a well-illuminated examination of the eyelids and the anterior segment of the eyeball using a specialized microscope.
Visual field tests assess the function of the retina, the optic nerve, and the optic pathways by recording the responses of the patient to light impulses directed to various areas of the visual field.
EYELID AND LACRIMAL DUCTS
Blepharitis
A common inflammation, blepharitis produces a red-rimmed appearance of the margins of the eyelids. It’s frequently chronic and bilateral and can affect both upper and lower lids. Seborrheic blepharitis is characterized by formation of waxy scales on the eyelashes and eyelid margins, and symptoms of burning and foreignbody sensation. Staphylococcal (ulcerative) blepharitis is characterized by formation of dry scales along the inflamed lid margins, which also have ulcerated areas and may be associated with keratoconjunctivitis sicca (KCS), a dry-eye syndrome. Both types may coexist. Blepharitis tends to recur and become chronic. It can be controlled if treatment begins before onset of ocular involvement.
CAUSES AND INCIDENCE
Seborrheic blepharitis may be seen in conjunction with seborrhea of the scalp, eyebrows, and ears. It’s common in elderly people and in
people with red hair. Staphylococcal blepharitis is associated with Staphylococcus aureus infection and is more common in females than in males. Allergies and eyelash infestations with lice are less-common causes of blepharitis. Blepharitis may also be associated with repeated styes and chalazion.
people with red hair. Staphylococcal blepharitis is associated with Staphylococcus aureus infection and is more common in females than in males. Allergies and eyelash infestations with lice are less-common causes of blepharitis. Blepharitis may also be associated with repeated styes and chalazion.
COMPLICATIONS
Keratitis
Conjunctivitis
Dry eyes
SIGNS AND SYMPTOMS
Clinical features of blepharitis include itching, burning, foreign-body sensation, and sticky, crusted eyelids on waking. This constant irritation results in unconscious rubbing of the eyes (causing reddened rims) or continual blinking. Other signs include waxy scales in seborrheic blepharitis; and flaky scales on lashes, loss of lashes, and ulcerated areas on lid margins in ulcerative blepharitis.
DIAGNOSIS
Diagnosis depends on patient history and characteristic symptoms. In staphylococcal blepharitis, culture of ulcerated lid margin shows S. aureus.
TREATMENT
The goals of therapy are to control the disease and its underlying causes, maintain vision, and avoid secondary complications. Treatment depends on the type of blepharitis:
blepharitis resulting from pediculosis— removal of nits (with forceps) or application of ophthalmic physostigmine or other ointment as an insecticide (This may cause pupil constriction and, possibly, headache, conjunctival irritation, and blurred vision from the film of ointment on the cornea.)
seborrheic blepharitis—daily lid hygiene (using a mild shampoo on a damp applicator stick or a washcloth) and hot compresses to remove scales from the lid margins; also, frequent shampooing of the scalp and eyebrows
staphylococcal blepharitis—warm compresses and an antibiotic, such as tetracycline or erythromycin eye ointment, may be used. For some patients, systemic antibiotics are indicated
SPECIAL CONSIDERATIONS
Instruct the patient to gently remove scales from the lid margins daily, with an applicator stick or a clean washcloth.
Teach the patient the following method for applying warm compresses: First, run warm water into a clean bowl. Then, immerse a clean cloth in the water and wring it out. Place the warm cloth against the closed eyelid (be careful not to burn the skin). Hold the compress in place until it cools. Continue this procedure for 15 minutes.
Antibiotic ophthalmic ointment should be applied after 15-minute application of warm compresses.
Treatment for seborrheic blepharitis also requires attention to the face and scalp.
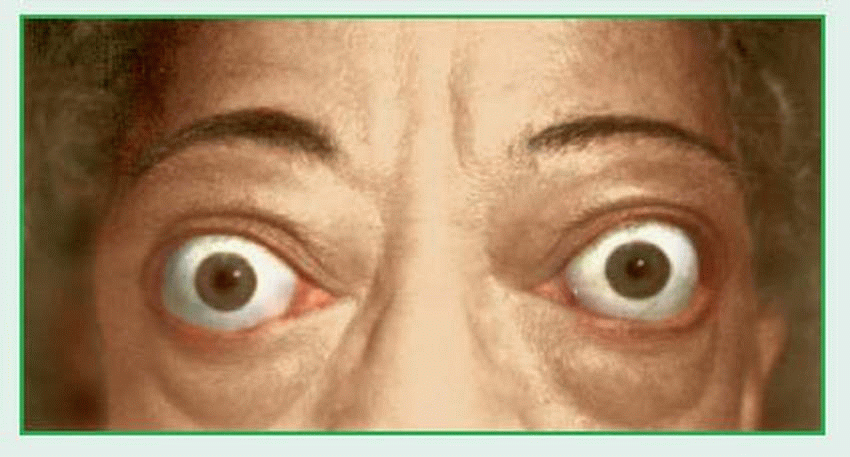
Exophthalmos
Exophthalmos (also called proptosis) is the unilateral or bilateral bulging or protrusion of the eyeballs or their apparent forward displacement (with lid retraction). The prognosis depends on the underlying cause.
CAUSES AND INCIDENCE
Exophthalmos commonly results from hyperthyroidism, particularly ophthalmic Graves’ disease, in which the eyeballs are displaced forward and the lids retract. Unilateral exophthalmos may also result from trauma (such as fracture of the ethmoid bone, which allows air from the sinus to enter the orbital tissue, displacing soft tissue and the eyeball forward). Exophthalmos may also stem from hemorrhage, varicosities, thrombosis, and edema, all of which similarly displace one or both eyeballs forward.
Other systemic and ocular causes include:
infection—orbital cellulitis, panophthalmitis, and infection of the lacrimal gland or orbital tissues
parasitic cysts—in surrounding tissue
tumors and neoplastic diseases—in children, rhabdomyosarcomas, leukemia, gliomas of the optic nerve, dermoid cysts, teratomas, metastatic neuroblastomas, and lymphoma; in adults, lacrimal gland tumors, mucoceles, cavernous hemangioma, meningiomas, metastatic carcinomas, and lymphoma
SIGNS AND SYMPTOMS
The obvious effect is a bulging eyeball, commonly with diplopia, due to eyeball misalignment or extraocular muscle dysfunction. (See Recognizing exophthalmos, page 600.) A rim of the sclera may be visible below the upper lid as lid retraction occurs. Other symptoms depend on the cause: pain may accompany
traumatic exophthalmos; a tumor may produce conjunctival hyperemia or chemosis; retraction of the upper lid predisposes to exposure keratitis. If exophthalmos is associated with cavernous sinus thrombosis, the patient may exhibit paresis of the muscles supplied by cranial nerves III, IV, and VI; limited ocular movement; and a septic-type (high) fever.
traumatic exophthalmos; a tumor may produce conjunctival hyperemia or chemosis; retraction of the upper lid predisposes to exposure keratitis. If exophthalmos is associated with cavernous sinus thrombosis, the patient may exhibit paresis of the muscles supplied by cranial nerves III, IV, and VI; limited ocular movement; and a septic-type (high) fever.
DIAGNOSIS
Exophthalmos is usually obvious on physical examination; exophthalmometer readings confirm diagnosis by showing the degree of anterior projection and asymmetry between the eyes (normal bar readings range from 12 to 20 mm). The following diagnostic measures identify the cause:
Computed tomography scan or magnetic resonance imaging detects swollen extraocular muscles or lesions within the orbit.
Culture of discharge determines the infecting organism; sensitivity testing indicates appropriate antibiotic therapy.
Biopsy of orbital tissue may be necessary if initial treatment fails.
TREATMENT
Eye trauma may require cold compresses for the first 24 hours, followed by warm compresses, and prophylactic antibiotic therapy. After edema subsides, surgery may be necessary in a small percentage of cases. It is important to counsel patients with acute orbital fractures not to blow their nose, to avoid air entering the orbit, which may cause acute exophthalmos. Eye infection requires treatment with broad-spectrum antibiotics during the 24 hours preceding positive identification of the organism, followed by specific antibiotics. A patient with exophthalmos resulting from an orbital tumor may initially benefit from antibiotic or corticosteroid therapy. Eventually, surgical exploration of the orbit and excision of the tumor, enucleation, or exenteration may be necessary. Radiation and chemotherapy may be used when primary orbital tumors can’t be fully excised as encapsulated lesions, such as in rhabdomyosarcoma lesions.
Treatment for Graves’ disease may include antithyroid drug therapy or partial or total thyroidectomy to control hyperthyroidism; initial high doses of systemic corticosteroids, such as prednisone, for optic neuropathy and, if lid retraction is severe, protective lubricants.
Surgery may include orbital decompression (removal of any of the orbital walls) if vision is threatened, followed by muscle surgery and then lid surgery (eyelid retraction repair).
SPECIAL CONSIDERATIONS
♦ It is critical to protect the exposed cornea with lubricants to prevent corneal drying until the disease stabilizes or is corrected by surgery.
Ptosis
Ptosis (drooping of the upper eyelid) may be congenital or acquired, unilateral or bilateral, and constant or intermittent. Severe ptosis usually responds well to treatment; slight ptosis may require no treatment at all.
CAUSES AND INCIDENCE
Congenital ptosis is transmitted as an autosomal dominant trait or results from a congenital anomaly in which the levator muscles of the
eyelids fail to develop. This condition is usually unilateral.
eyelids fail to develop. This condition is usually unilateral.
Acquired ptosis may result from any of the following:
advanced age (involutional ptosis, the most common form, usually seen in older patients)
mechanical factors that make the eyelid heavy, such as swelling caused by a foreign body on the palpebral surface of the eyelid or by edema, inflammation produced by a tumor or pseudotumor, or an extra fatty fold
myogenic factors, such as muscular dystrophy or myasthenia gravis (in which the defect appears to be in humoral transmission at the myoneural junction)
neurogenic (paralytic) factors from interference in innervation of the eyelid by the oculomotor nerve (cranial nerve III), most commonly due to trauma, diabetes, or carotid aneurysm (Ptosis due to oculomotor nerve damage produces a fixed, dilated pupil, divergent strabismus, and slight depression of the eyeball.)
nutritional factors, such as thiamine deficiency in chronic alcoholism, hyperemesis gravidarum, and other malnutrition-producing states
Risk factors for ptosis include aging, diabetes, stroke, Horner’s syndrome, myasthenia gravis, and cancer that affects nerve or muscle response.
In myasthenia gravis, ptosis results from fatigue and characteristically appears in the evening but is relieved by rest.
The child with unilateral ptosis that covers the pupil can develop an amblyopic eye from disuse or lack of eye stimulation. In bilateral ptosis, the child may elevate his brow in an attempt to compensate, wrinkling his forehead in an effort to raise the upper lid. Additionally, the child may tip his head backward to see.
COMPLICATION
♦ Lazy eye in children (amblyopia)
SIGNS AND SYMPTOMS
An infant with congenital ptosis has a smooth, flat upper eyelid, without the eyelid fold normally caused by the pull of the levator muscle; associated weakness of the superior rectus muscle isn’t uncommon.
DIAGNOSIS
Examination includes measurement of the position of the upper eyelid margin relative to the pupil, degree of eyelid excusion, presence or absence of lagophthalmos, Bell’s phenomenon, and eyelid crease. Diagnosis may also include these tests to determine any underlying cause:
digital subtraction angiography or magnetic resonance imaging—aneurysm
glucose tolerance test—diabetes
ophthalmologic examination—foreign bodies
patient history—chronic alcoholism
Tensilon test—myasthenia gravis (in acquired ptosis with no history of trauma)
TREATMENT
Slight ptosis that doesn’t produce deformity or loss of vision requires no treatment. Severe ptosis that interferes with vision or is cosmetically undesirable usually necessitates reattachment of a stretched levator aponeurosis. Surgery to correct congenital ptosis is usually performed at age 3 or 4, but it may be done earlier if amblyopia is a concern. The surgical approach depends on the degree of ptosis. If surgery is contraindicated, special glasses with an attached suspended crutch on the frames may elevate the eyelid.
Effective treatment for ptosis also requires treatment for any underlying cause. For example, in patients with myasthenia gravis, neostigmine or steroids may be prescribed to increase the effect of acetylcholine and aid transmission of nerve impulses to muscles.
SPECIAL CONSIDERATIONS
♦ After surgery to correct ptosis, watch for blood on the pressure patch. (Some surgical procedures may not require a patch.) Apply ointment to the sutures as prescribed.
♦ Emphasize to the patient and his family the need to prevent accidental trauma to the surgical site until healing is complete (6 weeks). Suture line damage can precipitate recurrence of ptosis.
Orbital cellulitis
Orbital cellulitis is an acute infection of the orbital tissues and eyelids that doesn’t involve the eyeball. With treatment, the prognosis is good; if untreated, the infection may spread intracranially to the cavernous sinus or the meninges, where it can be life-threatening.
CAUSES AND INCIDENCE
Orbital cellulitis may result from bacterial, fungal, or parasitic infection. It can develop from direct inoculation, via the bloodstream,
or spread from adjacent structures (e.g., the sinuses or eyelids). Periorbital tissues may be inoculated as a result of surgery, foreign body trauma, and even animal or insect bites.
or spread from adjacent structures (e.g., the sinuses or eyelids). Periorbital tissues may be inoculated as a result of surgery, foreign body trauma, and even animal or insect bites.
The most common patho gens in children are Haemophilus influenzae, Streptococcus pneumoniae, and Staphylococcus aureus. Inyoung children, infection spreads from adjacent sinuses (especially the ethmoid air cells) and accounts for the majority of postseptal cellulitis cases. The incidence has decreased because of the use of the H. influenzae b (Hib) vaccine.
Immunosuppressed patients are also susceptible.
COMPLICATIONS
Cavernous sinus thrombosis
Hearing loss
Septicemia
Meningitis
Optic nerve damage
SIGNS AND SYMPTOMS
Orbital cellulitis generally produces unilateral eyelid edema, reddened eyelids, and matted lashes. Although the eyeball is initially unaffected, proptosis develops later (because of edematous tissues within the bony confines of the orbit). Other indications include extreme orbital pain, impaired eye movement, chemosis, purulent discharge from indurated areas, decreased vision, and an afferent pupillary defect. The severity of associated systemic symptoms (chills, fever, and malaise) varies according to the cause.
Complications include posterior extension, causing cavernous sinus thrombosis, panophthalmitis, meningitis, or brain abscess and, rarely, atrophy and subsequent loss of vision secondary to optic neuritis.
DIAGNOSIS
Typical clinical features establish diagnosis. Computed tomography scan or magnetic resonance imaging of the sinuses and orbit tissues will determine if the cause of the cellulitis is preseptal or if deeper structures are involved, or if a tumor is the cause of swelling. Usually the patient will also be febrile with this type of infection. Wound culture and sensitivity testing determine the causative organism and specific antibiotic therapy. Other tests include white blood cell count and ophthalmologic examination.
TREATMENT
Prompt treatment is necessary to prevent complications. Primary treatment consists of antibiotic therapy. Systemic antibiotics (I.V. or oral) and eyedrops or ointment will be ordered. Supportive therapy consists of fluids; warm, moist compresses; and bed rest. The patient should be monitored closely. If during the initial 48 to 72 hours of treatment no improvement is seen, adjustment of antibiotics guided by drug sensitivity should be considered. If an orbital abscess is present, surgical incision and drainage may be necessary.
SPECIAL CONSIDERATIONS
Monitor vital signs at least every 4 hours, and maintain fluid and electrolyte balance.
Have the patient instill antibiotic eyedrops frequently during the day and apply ointment at night.
Apply compresses every 3 to 4 hours to localize inflammation and relieve discomfort. Teach the patient to apply these compresses. Give pain medication, as ordered, after assessing pain level.
Before discharge, stress the importance of completing prescribed antibiotic therapy. To prevent orbital cellulitis, tell the patient to maintain good general hygiene and to carefully clean abrasions and cuts that occur near the orbit.
Ensure patient has appropriate follow-up.
♦ Use Hib vaccination to prevent Haemophilus infection in children.
♦ Treat sinus and dental infections early to decrease spread to the eye.
Dacryocystitis
Dacryocystitis is an infection of the lacrimal sac. It can be acute, chronic, or congenital. In infants, dacryocystitis results from congenital atresia of the nasolacrimal duct; in adults, it results from an obstruction (dacryostenosis) of the nasolacrimal duct (most common in women older than age 40).
CAUSES AND INCIDENCE
Atresia of the nasolacrimal ducts results from failure of canalization or, in the first few months of life, from blockage when the membrane that separates the lower part of the nasolacrimal duct and the inferior nasal meatus fails to open spontaneously before tear secretion. Bony obstruction of the duct may also occur.
In acute dacryocystitis, Staphylococcus aureus and, occasionally, beta-hemolytic streptococci are the cause. In chronic dacryocystitis, Streptococcus pneumoniae or, sometimes, a fungus— such as Actinomyces or Candida albicans—is the causative organism. Primary lumps and secondary tumors from sinuses, nose, and orbits have also been reported as causes.
COMPLICATION
♦ Orbital cellulitis
SIGNS AND SYMPTOMS
The hallmark of both the acute and chronic forms of dacryocystitis is constant tearing. Other symptoms of dacryocystitis include inflammation and tenderness over the nasolacrimal sac; pressure over this area may fail to produce purulent discharge from the punctum. Acute dacryocystitis is painful for the patient.
DIAGNOSIS
Clinical features and a physical examination suggest dacryocystitis. Culture of the discharged material demonstrates Staphylococcus aureus and, occasionally, beta-hemolytic streptococci in acute dacryocystitis, and Streptococcus pneumoniae or C. albicans in the chronic form. The white blood cell count may be elevated in the acute form; in the chronic form, it’s generally normal. An X-ray after injection of a radiopaque medium (dacryocystography) locates the atresia in infants.
TREATMENT
Treatment for acute dacryocystitis consists of warm compresses, topical and systemic antibiotic therapy and, occasionally, incision and drainage. Chronic dacryocystitis may eventually require dacryocystorhinostomy. Laser-assisted endoscopic dacryocystorhinostomy and balloon dilatation or probing of the nasolacrimal system may also be used.
Therapy for nasolacrimal duct obstruction in an infant consists of careful massage of the area over the lacrimal sac four times a day for 6 to 9 months. If this fails to open the duct, dilation of the punctum and probing of the duct are necessary.
SPECIAL CONSIDERATIONS
Check the patient history for possible allergy to antibiotics before administration. Emphasize the importance of precise compliance with the prescribed antibiotic regimen.
Tell the adult patient what to expect after surgery. He’ll have ice compresses over the surgical site and will have bruising and swelling.
Monitor blood loss by counting dressings used to collect the blood.
Apply ice compresses postoperatively. A small adhesive bandage may be placed over the suture line to protect it from damage.
Chalazion
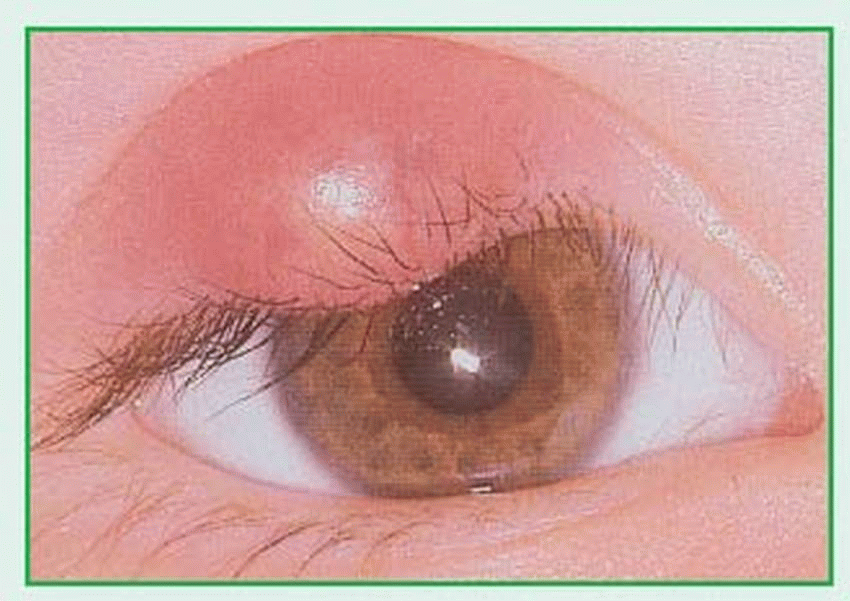
A chalazion is a chronic granulomatous inflammation of a meibomian gland or gland of Zeis in the upper or lower eyelid. (There are approximately 100 of these glands located near the eyelashes.) This common eye disorder is characterized by localized swelling within the tarsal plate, or it may break through the conjunctival or skin side. Mild irritation and blurred vision usually develop slowly over several weeks. (See Recognizing chalazion.) A chalazion may become large enough to press on the eyeball, causing astigmatism. A large chalazion seldom subsides spontaneously. It’s generally benign and chronic, and can occur at any age. In some patients, it’s apt to recur.
CAUSES AND INCIDENCE
Obstruction of the meibomian (sebaceous) gland duct causes a chalazion.
SIGNS AND SYMPTOMS
A chalazion occurs as a painless, hard lump that usually points toward the conjunctival side of the eyelid. Eversion of the lid reveals a red or red-yellow elevated area on the conjunctival surface. Otherwise, it’s seen as an indurated bump under the skin of the upper eyelid.
DIAGNOSIS
Diagnosis requires visual examination and palpation of the eyelid, revealing a small bump or nodule. Persistently recurrent chalazions, especially in an adult, necessitate biopsy to rule out sebaceous cell carcinoma.
TREATMENT
Initial treatment consists of application of warm compresses for 10 to 15 minutes at least four times a day to open the lumen of the gland, soften the hardened oils blocking the duct, and promote drainage and healing. If such therapy fails, or if the chalazion presses on the eyeball or causes a severe cosmetic problem, steroid injection or incision and curettage under local anesthetic may be necessary. After such surgery, a pressure eye patch applied for 4 to 6 hours controls bleeding and swelling. After removal of the patch, treatment again consists of warm compresses. Antibiotic eyedrops are occasionally prescribed before and after cyst removal, but otherwise are of little value.
SPECIAL CONSIDERATIONS
Instruct the patient how to properly apply warm compresses: Tell him to take special care to avoid burning the skin, to always use a clean cloth, and to discard used compresses. Also tell him to start applying warm compresses at the first sign of lid irritation to increase the blood supply and keep the lumen open.
Teach the patient how to instill antibiotic eyedrops.
Stye
A localized, purulent staphylococcal infection, a stye (or hordeolum) can occur externally (in the lumen of the smaller glands of Zeis or in Moll’s glands) or internally (in the larger meibomian gland). A stye can occur at any age. Generally, styes are self-limiting and respond well to hot, moist compresses. More than one may occur at the same time. If untreated, a stye can eventually lead to cellulitis of the eyelid. Styes can also develop into a chalazion if gland ducts are fully blocked.
CAUSES AND INCIDENCE
Skin bacteria that enter eyelash hair follicles and cause inflammation can result in stye formation. Risk factors include blepharitis, diabetes and other chronic debilitating illnesses, and seborrhea.
COMPLICATION
♦ Cellulitis of the eyelid
SIGNS AND SYMPTOMS
Typically, a stye produces redness, swelling, and pain. An abscess frequently forms at the lid margin, with an eyelash pointing outward from its center. (See Recognizing a stye.)
DIAGNOSIS
Visual examination generally confirms this infection. Culture of purulent material from the abscess usually reveals a staphylococcal organism.
TREATMENT
Treatment consists of warm compresses applied for 10 to 15 minutes, four times a day for 3 to 4 days, to facilitate drainage of the abscess, to relieve pain and inflammation, and to promote suppuration. Drug therapy includes a topical sulfonamide or antibiotic eyedrops or ointment and, occasionally, a systemic antibiotic for secondary eyelid cellulitis. If conservative treatment fails, incision and drainage may be necessary.
SPECIAL CONSIDERATIONS
Instruct the patient to use a clean cloth for each application of warm compresses and to dispose of it or launder it separately.
Warn against squeezing the stye; this spreads the infection and may cause cellulitis.
Teach the patient or his family members the proper technique for instilling eyedrops or ointments into the cul-de-sac of the lower eyelid.