Extranodal NK-/T-cell Lymphoma, Nasal Type
L. Jeffrey Medeiros, MD
Key Facts
Etiology/Pathogenesis
EBV is constant finding, present in clonal episomal form, and is likely involved in pathogenesis
Clinical Issues
Nasal or extranasal
Microscopic Pathology
Cytologic spectrum of nasal-type extranodal NK/T-cell lymphoma is wide
Small cell neoplasms can be misinterpreted as chronic inflammation
Necrosis and superimposed acute and chronic inflammation can lead to incorrect diagnosis
Angiocentricity and angiodestruction are helpful findings but are not constant
Most likely to be absent in small biopsy specimens
Ancillary Tests
Approximately 2/3 of tumors are of NK cell lineage: CD2(+), cyt CD3-∈(+), CD56(+/-), CD5(-), CD8(-), TCR gene rearrangements(-)
Approximately 1/3 of tumors are of cytotoxic T-cell lineage: CD2(+), CD3(+), CD5(+), CD8(+/-), TCR-β(+), TCR gene rearrangements(+)
All tumors are positive for cytotoxic proteins and EBV (best shown by in situ hybridization for EBER)
Top Differential Diagnoses
Cytotoxic EBV-peripheral T-cell lymphoma, not otherwise specified
B-cell lymphomas involving upper aerodigestive tract (usually diffuse large B-cell lymphoma)
Wegener granulomatosis
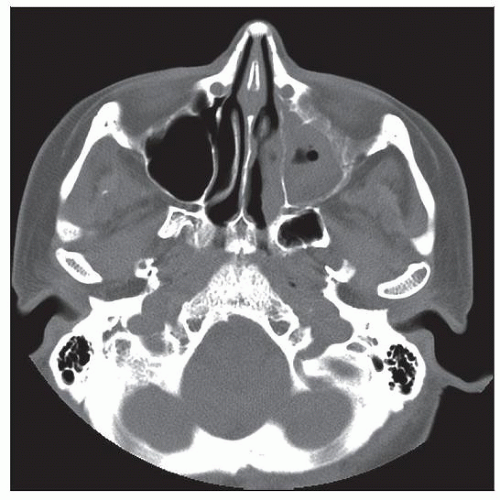 CT scan shows an almost completely opacified maxillary sinus and thickening of mucosa in the nasopharynx. This patient was shown to have extranodal NK/T-cell lymphoma, nasal type. |
TERMINOLOGY
Synonyms
Polymorphic reticulosis
Malignant midline reticulosis
Angiocentric T-cell lymphoma
Angiocentric immunoproliferative lesion
Term is not completely synonymous but includes nasal-type extranodal NK/T-cell lymphoma
Definitions
Predominantly extranodal lymphoma of either natural killer-cell (NK) or T-cell lineage
Characterized by necrosis, cytotoxic immunophenotype, and Epstein-Barr virus (EBV) infection
Vascular destruction is common
ETIOLOGY/PATHOGENESIS
Infectious Agents
EBV is consistently present in these neoplasms, suggesting its involvement in pathogenesis
EBV is usually type A
Epidemiology
Disease is common in Asia and in Native Americans of Central and South America
Disease is rare in United States, but its incidence has risen since 1992
CLINICAL ISSUES
Presentation
Mass that is nasal or extranasal
Nasal cases are usually defined as a neoplasm involving upper aerodigestive tract
Nasal cavity, nasopharynx, paranasal sinuses, palate
Patients suffer from obstruction, epistaxis, or midline destructive lesion
These neoplasms can disseminate
Extranasal cases are defined as neoplasm involving any site but without nasal involvement
Skin is most common extranasal site
Other sites: Testis, gastrointestinal tract, kidney, salivary glands
Primary involvement of lymph nodes is rare but has been reported
Bone marrow obtained as part of staging can be involved
Natural History
Extranodal nasal-type NK/T-cell lymphoma can disseminate
Regional lymph node involvement is not uncommon
Bone marrow involvement and leukemic phase can occur
These neoplasms can disseminate to virtually any anatomic site
Treatment
Options, risks, complications
Chemotherapy and radiation therapy are usually employed for nasal cases
Platelet-derived growth factor α overexpression shown by gene expression studies suggests role for imatinib
Prognosis
Patients with nasal-type extranodal NK/T-cell lymphoma, in general, have poor prognosis
Patients with extranasal tumors have poorest prognosis
Factors associated with poorer prognosis for nasal cases include
High International Prognostic Index (IPI) or Korean NK/T-cell Prognostic Score
Elevated C-reactive protein, anemia (< 11g/dL), or thrombocytopenia (< normal)
Large cells > 40%
Ki-67 (proliferation rate) > 50%
Korean NK/T Prognostic Score is based on
B symptoms, stage, serum LDH, and regional lymph nodes
IMAGE FINDINGS
General Features
Location
Nasal: Imaging studies show mass that can distort midline, displace adjacent organs, and destroy bone
Extranasal: Imaging studies usually show mass
MICROSCOPIC PATHOLOGY
Histologic Features
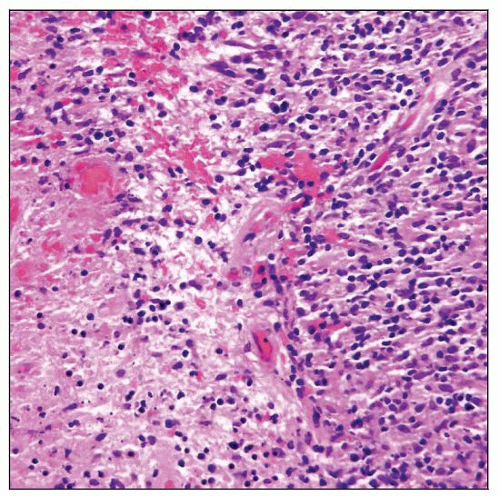
Nasal-type NK/T lymphoma has diffuse pattern; commonly associated with coagulative necrosis
Cell size is variable, ranging from small to large
Mitotic figures are usually identified; common in large tumors
In touch imprints, neoplastic cells can have azurophilic cytoplasmic granules
Angiocentricity and angiodestruction are common but not invariable
Less common in small biopsy specimens
Ulcer and superimposed inflammation are common at mucosal sites
Overlying epithelium at mucosal sites can show pseudoepitheliomatous hyperplasia
Erythrophagocytosis can complicate clinical course; can be fatal
Lymph node
Nasal-type NK/T preferentially involves paracortex ± medulla
Bone marrow
Staging bone marrow is involved in ˜ 10-20% of patients
Commonly an interstitial infiltrate without discrete aggregates
In situ hybridization for EBER helpful to detect disease
Cytologic Features
Nasal-type NK/T-cell lymphoma is uncommonly assessed by fine needle aspiration
Superimposed inflammation can make recognition of the disease challenging
ANCILLARY TESTS
Immunohistochemistry
NK-cell lineage in ˜ 65-75% of cases
CD2(+), cytoplasmic CD3-∈(+), CD56(+/-), CD94(+) cytotoxic markers (TIA, GZM-B, perforin)(+)
Both T and NK cells express epsilon chain of CD3 (CD3-∈)
CD4(-), CD5(-), CD8(-), TCR-β (BF1)(-)
True T-cell lineage in approximately 25-35% of cases
CD2(+), CD3-∈(+), CD5(+), CD8(+/-), TCR-β (BF1)(+), CD56(-/+), cytotoxic markers(+)
Both NK- and T-cell neoplasms are positive for Epstein-Barr virus
Can be shown by variety of molecular methods (Southern blotting, in situ hybridization)
In situ hybridization for EBV small-encoded RNA (EBER) is convenient and sensitive
Southern blot studies have shown that EBV is present in clonal episomal form
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree