Extranodal Marginal Zone B-cell Lymphoma (MALT Lymphoma)
Pei Lin, MD
Key Facts
Etiology/Pathogenesis
Infectious agents are implicated in pathogenesis of MALT lymphomas at specific sites
Helicobacter pylori: Stomach
Campylobacter jejuni: Intestine
Chlamydia psittaci: Ocular adnexa
Borrelia burgdorferi: Skin
Autoimmune diseases are implicated in pathogenesis of MALT lymphomas at specific sites
Sjögren syndrome: Salivary glands and lung
Hashimoto thyroiditis: Thyroid gland
Microscopic Pathology
MALT lymphomas share common features
Marginal zone pattern surrounding reactive follicles
Heterogeneous cell population
± lymphoepithelial lesions
Ancillary Tests
CD20(+), CD22(+), CD79a(+), pax-5(+)
Monotypic Ig(+), Bcl-2(+), CD43(+/-), Ki-67 low
Recurrent translocations identified in 30-40% of MALT lymphomas
4 common translocations
IAP2-MALT1/t(11;18)(q21;q21)
IgH-MALT1/t(14;18)(q32;q21)
FOXP1-IgH/t(3;14)(p14.1;q32)
BCL10-IgH/t(1;14)(p22;q32)
Top Differential Diagnoses
Reactive hyperplasia
Mantle cell lymphoma
Follicular lymphoma
Plasmacytoma
TERMINOLOGY
Abbreviations
Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma)
Synonyms
Low-grade B-cell lymphoma of MALT
MALToma
Definitions
Low-grade B-cell lymphoma arising at extranodal sites, presumably in marginal zone of reactive follicles
ETIOLOGY/PATHOGENESIS
Infectious Agents
Implicated in pathogenesis of MALT lymphomas
Helicobacter pylori
Gastric marginal zone lymphoma
Campylobacter jejuni
Immunoproliferative small intestinal disease; also known as α heavy chain disease
Chlamydia psittaci
Ocular adnexal marginal zone lymphoma
Borrelia burgdorferi
Cutaneous marginal zone lymphoma
More common in Europe
Autoimmune Disorders
2 autoimmune diseases have been implicated in pathogenesis of MALT lymphomas
Sjögren syndrome
MALT lymphomas of parotid gland and lung
Hashimoto thyroiditis
Thyroid MALT lymphoma
Chromosomal Translocations
Identified in 30-40% of MALT lymphomas
Result in NF-κB pathway activation resulting in enhanced cell survival and proliferation and impaired apoptosis
MALT Lymphomas Without Chromosomal Translocations
Possible role for antigen drive
Chronic antigen stimulation via infection or autoimmune disease
Leads to accumulation of extranodal lymphoid tissue
Polyclonal B-cell population evolves to oligoclonal and then monoclonal B-cell population
No central role for NF-κB activation
CLINICAL ISSUES
Epidemiology
Incidence
7-8% of all B-cell non-Hodgkin lymphomas
Age
Median: 61 years
Gender
Female predominance
Presentation
Subset of patients are asymptomatic
Symptoms are related to organ involved
Stomach: Anemia, weight loss, and pain are common
Lung: ± cough and dyspnea
Mass and related symptoms in other locations
Treatment
Prognosis
Stomach MALT lymphoma
Lymphoma can regress after eradication of H. pylori by antibiotics; true in ˜ 75% of cases
t(11;18)(q21;q21) is associated with resistance to antibiotics
< 10% of cases transform to diffuse large B-cell lymphoma
5-year overall survival is ˜ 90%
25-35% relapse rate in stomach or other extranodal sites
Other sites of MALT lymphoma
Disseminated disease is more common
Higher relapse rate
IMAGE FINDINGS
Radiographic Findings
Single or multiple masses
Lung(s) involved by MALT lymphoma ± consolidation
Endoscopic Findings
Gastric or intestinal MALT lymphoma: ± mass, ulcer, or bleeding
MICROSCOPIC PATHOLOGY
Histologic Features
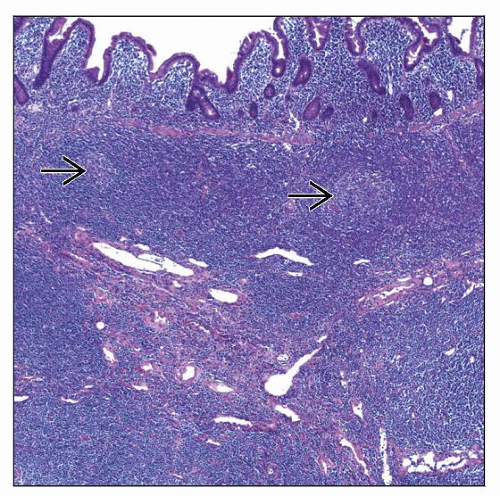
Diffuse or nodular pattern of growth
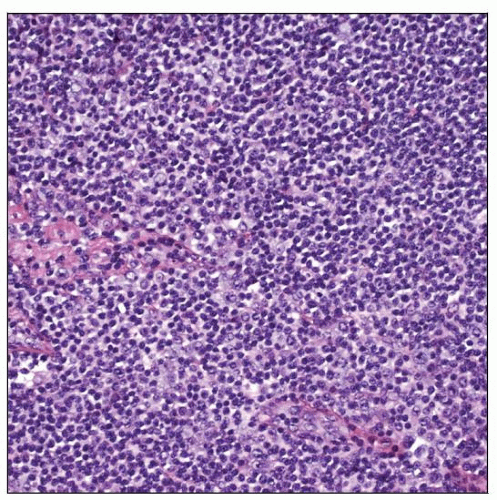
Expansion of marginal zone by cytologically heterogeneous cell population
Predominantly centrocyte-like cells with small irregular nuclei
Monocytoid appearance with distinct rim of clear cytoplasm
Scattered large cells (centroblasts or immunoblasts) are present; up to 10% of all cells
± plasmacytoid differentiation; ± Dutcher bodies
Hyperplastic lymphoid follicles are common
± colonized by lymphoma imparting nodular pattern
Lymphoepithelial lesions are common in epithelial tissues involved by MALT lymphoma
Infiltration and distortion of epithelial structures by 3 or more neoplastic lymphoid cells
Epithelial degeneration and glandular structure destruction
Most prominent in thyroid and parotid glands
Transformation to diffuse large B-cell lymphoma
Large cells form sheets or large clusters of > 20 cells
May coexist with MALT lymphoma at initial presentation
Multifocal disease
˜ 25% of patients have > 1 extranodal site of involvement
Cytologic Features
FNA smears show polymorphous cell population
Small round or irregular lymphocytes, variable numbers of large cells &/or plasma cells
Lymph Nodes
Involvement is indistinguishable from nodal marginal zone B-cell lymphoma
Usually lymph nodes draining primary site of disease are involved
Distant lymph nodes involved in < 10% of patients
Bone Marrow
10-20% of patients with MALT lymphoma have bone marrow disease at staging
Paratrabecular &/or nonparatrabecular aggregates
Follicular dendritic cells commonly present in aggregates
Sinusoidal pattern highly unusual
Skin
Most common B-cell lymphoma of skin
Follicular colonization can be prominent; these lesions closely mimic follicular lymphoma
Ocular Adnexal Region
Includes orbital soft tissue, conjunctiva, and lacrimal gland
MALT is most common type of lymphoma at this location
Lung
Lymphoepithelial lesions common in MALT lymphoma and lymphocytic interstitial pneumonitis
Circumscribed mass supports diagnosis of MALT lymphoma
Salivary Gland
Arises in background of myoepithelial sialadenitis (MESA)
Lymphoepithelial lesions (epithelial-myoepithelial islands) common in MALT lymphoma and MESA
Concentric zones of pale cells around ducts are helpful clue for MALT lymphoma
Thyroid Gland
Arises in background of Hashimoto thyroiditis
Lymphoepithelial lesions common in both MALT lymphoma and Hashimoto thyroiditis
Lymphoma cells within follicles tend to be centrocyte-like cells
Lymphoma cells outside follicles often are extremely plasmacytic
Breast
Lymphoepithelial lesions are uncommon at this site
Can arise in or be disseminated to breast
Other MALT Lymphoma Sites
Very wide range of body sites can be involved
Dura, soft tissues, thymus, gallbladder, kidney, bladder
ANCILLARY TESTS
Immunohistochemistry
CD19(+), CD20(+), CD22(+), CD79a(+), pax-5(+)
IgM(+) > IgA(+) > IgG(+)
Monotypic Ig light chain(+); best seen in plasmacytoid cells
Bcl-2(+), CD43(+/-), Bcl-10(+/-)
Ki-67(MIB-1) is low; high in residual reactive germinal centers
IgD(-) but demonstrates intact follicular IgD(+) mantle zones
CD21 highlights follicular dendritic cell (FDC) meshworks in follicles
Meshworks are disrupted by follicular colonization
Cytokeratin(-); useful for highlighting lymphoepithelial lesions
CD10(-), Bcl-6(-), Cyclin-D1(-)
T-cell antigens(-), EBV-LMP1(-)
Flow Cytometry
Monotypic surface Ig light chain(+)
FMC7(+), CD11c(+/-), CD23(-/+), CD25(-), CD103(-)
Cytogenetics
Recurrent translocations have been identified in 30-40% of MALT lymphomas
Generally specific for MALT lymphomas; translocations are mutually exclusive
4 common translocations; additional translocations recently described but not fully characterized
Frequency of translocations shows geographic variation; also correlates with site of MALT lymphoma
API2-MALT1/t(11;18)(q21;q21)
Most common in stomach, lung, and intestine
IgH-MALT1/t(14;18)(q32;q21)
Most common in ocular adnexa, skin, salivary glands, and liver
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree