Extramammary Paget Disease
Maria Angelica Selim, MD
Russell Ball, MD
Key Facts
Terminology
Intraepidermal adenocarcinoma (primary or secondary) with frequent extension into adnexal structures; rarely invasive
Clinical Issues
Often, clinically misdiagnosed as inflammatory process (dermatitis)
Moist, red, eczematous-appearing plaque
Prognosis worse if nodules visible, elevated CEA levels, > 1 mm dermal invasion, lymph node metastasis, underlying malignancy
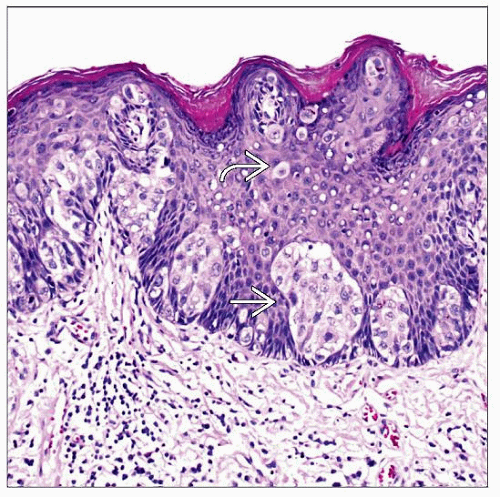
Microscopic Pathology
Nests &/or single cells and, less commonly, glands confined to basal and parabasal or higher layers
Associated proliferative epidermal lesions in 1/3
Invasive component in up to 48% of primary EMPD
Ancillary Tests
Primary and secondary EMPD: CAM5.2, CEA, EMA positive and ER, PR, MART-1/Melan-A, tyrosinase, MITF, and HMB-45 negative; rarely S100(+)
Primary: CK7, GCDFP-15, MUC1, MUC5 positive
Secondary anorectal: CK20, CDX-2, MUC2 positive
Secondary urothelial: CK7, CK20, and uroplakin-3 positive
Secondary cervical: p16 positive
Top Differential Diagnoses
Squamous cell carcinoma
Melanoma
Clear cell papulosis
Sebaceous carcinoma
 Extramammary Paget disease often presents as a scaly, erythematous plaque, mimicking an inflammatory process. (Courtesy L. Edwards, MD.) |
TERMINOLOGY
Abbreviations
Extramammary Paget disease (EMPD)
Synonyms
Mammary Paget disease (MPD)
Definitions
Primary (85%)
Intraepidermal adenocarcinoma with frequent extension into adnexal structures; rarely invasive
No underlying malignancy
Secondary (15%)
Intraepidermal adenocarcinoma associated with underlying (extracutaneous) malignancy (cervical, anorectal, urinary)
ETIOLOGY/PATHOGENESIS
Theories Regarding Cell of Origin
Pluripotential epidermal or adnexal stem cells
Clear cells of Toker
Traditionally accepted as origin of mammary Paget disease (CK7 positive and CK20 negative cells present at opening of lactiferous ducts)
Recently identified as normal constituent of vulvar, perineal, and perianal skin at ostia/opening of anogenital mammary-like glands
Greater frequency of Toker cells in areas of extramammary Paget disease
Bartholin gland
Apocrine glands
Anogenital mammary-like glands
CLINICAL ISSUES
Epidemiology
Incidence
Rare (˜ 2% of vulvar neoplasms)
Most common vulvar adnexal malignancy (primary EMPD)
Age
Typically after 4th decade, peak at ˜ 65 years
Ethnicity
Caucasians
Site
Anogenital skin
Labia majora > labia minora > clitoris
Presentation
Moist, red, eczematous-appearing plaque
Often pruritic
Rarely hyperpigmented
May be ulcerated
Multifocal extent may be clinically apparent
Clinically, may mimic inflammatory process (dermatitis), seborrheic keratosis, pigmented condyloma, or pigmented vulvar intraepithelial neoplasia
Treatment
Wide local excision
Lymph node dissection, if invasive component > 1 mm
Surgical treatment challenging due to
Visual assessment of gross margins often misleading
Appearance at frozen section often deceptive
Margin status not particularly accurate to predict recurrence as tumor often multifocal (skip lesions)
Topical bleomycin, 5-fluorouracil, carbon dioxide laser, imiquimod, or systemic retinoids if recurrent in situ disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree