Evaluation and Repair of Common Facial Injuries
Eduardo D. Rodriguez
with the assistance of
Gerhard S. Mundinger
Craniofacial trauma occurs in broad demographic and severity spectra, and is frequently associated with multisystem trauma. Multidisciplinary cooperation between trauma surgeons, orthopedists, neurosurgeons, oral surgeons, ophthalmologists, otolaryngologists, and plastic surgeons is central to facilitating timely and effective reconstruction. Every facial injury results in damage to soft tissue, with many involving injury to both soft tissue and bone. While well-trained general surgeons can easily manage most soft-tissue injuries with fundamental wound care, common bony injuries and injuries to complex structures are best managed by surgeons with craniofacial expertise. Although there are few true facial emergencies, the advantages and superior aesthetic results of prompt, definitive anatomical reconstruction of facial bone and soft-tissue injuries has been historically underemphasized. As the face is vital for communication, perception, nutrition, and interpersonal relationships, appropriate management of craniofacial trauma is thus essential for maintenance of patient livelihood and identity.
This chapter provides an overview of the evaluation, management, and treatment of the most common manifestations of craniofacial trauma that a trauma surgeon is likely to encounter. Aspects of the history and physical examination that dictate special management are emphasized, along with indications for radiologic examination. Injuries to complex structures, including the lacrimal system, facial nerve, and Stensen’s duct, are reviewed. Preferred techniques for the treatment of soft-tissue injuries, including wound management, antibiotics, local anesthetics, and closure methods, are comprehensively discussed. The chapter concludes with an overview of common facial fracture patterns and their operative management. The information in this chapter will facilitate appropriate, timely multidisciplinary care that reduces the need for late operations, avoids prolonged rehabilitation, and minimizes psychological scarring of the craniofacial trauma patient.
Initial Evaluation
Facial trauma, though deserving of prompt attention, is rarely life-threatening. Because they are often dramatic in appearance and instinctually interesting, craniofacial injuries have the potential to deter the clinician from appropriate evaluation of other more serious occult injuries. The presence of a facial injury implies that a simultaneous injury to adjacent areas such as the neck, brain, and skull may have occurred. Therefore, brain injury, skull fracture, and cervical spine injury must be excluded, as such injuries often have more serious immediate consequences. In all circumstances, the American College of Surgeons principles of advanced trauma life support (ATLS) remain paramount. Assessment of airway, breathing, and circulation are performed in the primary survey. The level of consciousness according to the Glasgow Coma Scale (Table 1) should be succinctly recorded and serially reassessed.
Table 1 The Glasgow Coma Scale | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||
Evaluation of craniofacial injuries takes place in the secondary survey. The observation of other organ systems must be continued throughout the entire period of facial injury treatment and continuous monitoring provided where appropriate. That said, there are three mechanisms by which craniofacial trauma alone can be inherently life-threatening. These are (a) airway obstruction, (b) aspiration, and (c) hemorrhage.
Airway obstruction: The craniofacial trauma patient frequently has an impaired level of consciousness, and therefore cannot adequately protect his or her airway. Additionally, massive facial swelling, displaced fractures, extensive soft-tissue injuries, and cervical spine injury are common. Each of these singular factors, let alone in combination, greatly increases the risk of aspiration and the inability to maintain oxygen saturation. The maintenance of a safe airway is crucial in craniofacial trauma, and, as in all trauma cases, must be the first management priority. Intubating the craniofacial trauma patient can be very challenging, and the airway team must be prepared to perform emergency cricothyroidotomy or tracheotomy when standard orotracheal intubation is not possible. Cricothyroidotomy should be converted to tracheotomy as soon as feasible, especially in patients who are comatose or not expected to control their own airway within 1 week.
One special scenario is noteworthy: bilateral mandible fractures that lead to airway compromise due to prolapse of the central segment. Airway compromise can be temporized in this scenario by bridle wiring around two teeth on either side of the fracture segment, or, in the case of a prolapsed medial segment due to bilateral parasymphyseal fractures, with anterior traction on the tongue using a towel clamp or suture. This pulls the prolapsed medial segment anteriorly as an airway-preserving measure.
Aspiration: The confused or obtunded trauma patient may aspirate oral secretions, blood, or gastric contents. The risk of aspiration and subsequent aspiration pneumonia is exacerbated by simultaneous midface and mandibular fractures, and is more common in patients with cerebral injuries. Rapid, noisy respirations, a low arterial oxygen content, decrease in oxygenation, and a decrease in pulmonary compliance are seen early on. Simple intubation prevents aspiration and should be performed early when
there is evidence that the airway is not being protected.
Hemorrhage: Life-threatening hemorrhage from craniofacial trauma has two mechanisms: (a) bleeding from facial lacerations, and (b) bleeding from the sinuses and cranial base. Bleeding from facial lacerations is the result of transected arteries and veins. The partially transected major artery can result in near exsanguination. Arterial hemorrhage is best controlled by direct suture, carefully avoiding the locations of branches of the facial nerve. Similarly, major veins may require suture ligation. While blunt contusion causes bleeding within facial soft tissue, this bleeding is usually tamponaded by facial soft-tissue pressure. The result is a hematoma that is either diffuse or localized. Localized hematomas should be drained, as the pressure generated from the expanding hematoma may produce tissue necrosis. Additionally, pressure produced by osmotic imbibition as the hematoma dissolves may impair circulation, causing tissue atrophy and even infarction. The treatment of localized hematomas is discussed later in this chapter. Observation is the only treatment for diffuse hematomas.
Cranial base, orbital, and midface fractures may produce hemorrhage from lacerations of arteries and veins within the sinus cavities. Cranial base bleeding can involve major arteries and veins, cannot be controlled by tamponade, and must always be considered in cases of massive facial hemorrhage. It must be quickly recognized when present as it can cause rapid exsanguination. Generally, bleeding from midface fractures can be controlled by four mechanisms: (a) the maxilla can be repositioned and secured in the best “rest” position by applying maxillomandibular fixation (MMF); (b) a posterior pack can be placed as an obturator in the nasopharynx, and anterior packing can be placed against the posterior pack; this provides tamponade pressure for lacerated vessels in sinus walls; (c) selective arterial embolization may be utilized for those cases that do not respond to manual maxillary repositioning and anterior–posterior nasal packing; (d) rarely, and when the above measures fail, bilateral external carotid and superficial temporal artery ligation or coil embolization, performed simultaneously, reduces the pressure in the external carotid system and may assist in control of massive orbital and midface hemorrhage.
Once the initial trauma evaluation is complete, and life-threatening trauma (systemic or isolated craniofacial) has been adequately addressed, management can focus on craniomaxillofacial injury. Details surrounding the traumatic episode including mechanism of injury and elapsed time until presentation are crucial determinants of next steps in diagnostic and therapeutic measures. Historians, including witnesses, family members, and emergency medical staff, can provide valuable information. Many craniofacial trauma patients are under the influence of intoxicating substances, and this potentiality should be investigated through appropriate toxicology screens when indicated. The patient’s current medications and past medical history, including tetanus immunization status, should be documented.
The diagnosis of most facial injuries is accurately suggested by thorough clinical examination. Discoloration, pain, localized tenderness, numbness or paralysis, malocclusion, crepitus step-off or level discrepancies over the margins of facial bones, double vision, decreased visual acuity, facial asymmetry, gross facial deformity, changes in facial contour, and changes in eye position (exophthalmos or enophthalmos, vertical dystopia, etc.) are all symptoms suggestive of deeper structural trauma. Soft-tissue injuries are inevitable and one should suspect an existing fracture of the underlying facial bones beneath any contusion, bruise, or laceration. Ideally, photographs of trauma sites should be taken in the emergency department, or sketches of wounds should be included as part of the craniofacial evaluation.
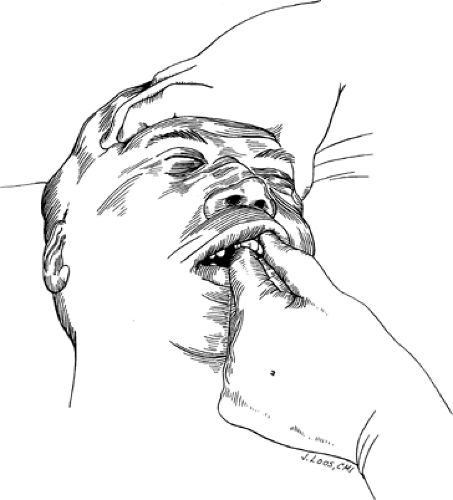
Two types of physical examination should be performed: sequential and directed. In the sequential examination, an orderly examination of all facial structures is methodically performed. Examination proceeds from cephalad to caudal (or caudal to cephalad), and lateral to medial in each of the following facial regions: forehead, orbits, nose, maxilla, and mandible. Extensive palpation of all bony surfaces should note tenderness and deformity. In particular, the superior and inferior orbital rims, zygomatic arches, and malar prominences should be palpated. The mandible should be thoroughly evaluated with an intraoral examination including direct palpation of the maxillary and mandibular dental arches, mandibular teeth, and the horizontal and vertical portions of the mandible. The occlusal relationship of the maxillary and mandibular dental arches should be noted. If lucid and cooperative, the patient should be asked if his or her teeth feel like they are meeting together normally. The excursion of the mandible while palpating the temporomandibular joint and the relationship of the mandible to the maxilla should also be evaluated. Midface instability suggestive of maxillary fractures can be determined by bimanual palpation (Fig. 1). In this technique, the upper alveolar ridge is manipulated with one hand while the other
hand stabilizes the head while palpating the nasal root.
hand stabilizes the head while palpating the nasal root.
The presence of “step-off” or “level” deformities in the dentition, bleeding, loose teeth, and intraoral lacerations all suggest areas of deeper bony involvement. Irregularities in the dental arch and abnormal areas of occlusion are all suggestive of localized fractures. Avulsed or missing teeth and intraoral or gingival lacerations indicate the possibility of an underlying fracture of the alveolus, or more extensive fracture of the mandible or maxilla. Lacerations of the lips, chin, palate, and floor of the mouth often accompany fractures of the jaws. The search for occult lacerations must include the eyelids, ear canal, mouth, floor of the mouth under the tongue, pharynx, and nasal cavity. Nasal examination is greatly facilitated by using a nasal speculum. Pain and pressure sensation, including complete anesthesia or hypoesthesia, should be documented in the supraorbital, corneal, infraorbital, and mental nerve distributions. Crucially, the neurologic facial examination, including evaluation of all cranial nerves, must be completed and documented before the administration of any local infiltrative anesthesia or nerve blocks. Any history of posttraumatic neck pain or alteration in peripheral motor or sensory function precludes operative treatment of facial injuries, as this raises suspicion for concomitant cervical spine injury.
The eye and function of vision must be specifically evaluated in the sequential examination with ophthalmologic consultations called when appropriate. The symmetry of the pupil, speed of pupillary reaction, presence of hyphema, and range of extraocular motion should be evaluated. The presence of periorbital or subconjunctival ecchymosis implies the possibility of an orbital fracture or globe injury. Visual acuity, field deficits, diplopia, afferent pupillary defect, or decreased light perception must be promptly evaluated.
Following the sequential physical examination, a directed physical examination should then thoroughly reevaluate specific areas where fractures or injury to specific structures are suspected as suggested by the sequential examination. The following key injuries are common, and warrant extensive directed examination.
Any lacerations of the eyelid suggest the possibility of globe rupture, and the globe must be examined for integrity if an eyelid laceration is discovered. Lacerations occurring in the medial third of the lower or upper eyelids suggest the possibility of lacrimal system injury, and the punctae and lacrimal duct should be thoroughly examined. The repair of injuries to the lacrimal system is discussed later in the chapter.
Fractures that involve the frontal or basilar skull may lacerate the dura, leading to pneumocephalus (passage of air inside the skull) or cerebrospinal fluid (CSF) leak. CSF may exit from the nose (CSF rhinorrhea) or ear (CSF otorrhea). This implies a communication between the subdural space and the external environment, raising the possibility of meningitis. CSF rhinorrhea or otorrhea is often obscured by the presence of blood mixed with draining CSF, making the detection and confirmation of a CSF leak difficult. A “double ring” or “halo” sign may be visible when draining blood and CSF is absorbed to a paper towel. This may be subsequently confirmed via serum electrophoresis. In the presence of displaced fractures, intracranial repair of the dura is indicated. Definitive operative treatment is accompanied by the administration of prophylactic antibiotics for several days. Therefore, rhinorrhea and/or otorrhea in the setting of craniofacial trauma should be evaluated thoroughly for the presence of CSF, warranting detailed computed tomography (CT) evaluation of the cranial base. Conversely, the presence of pneumocephalus on CT imaging raises high clinical suspicion for a CSF leak that should be thoroughly investigated and ruled out.
Radiologic Evaluation
Computed tomographic scans of the face, cervical spine, and head are warranted in nearly all cases of facial trauma. A thin-cut (<3 mm/slice) axial face CT with coronal and sagittal reconstructions is the current “gold standard” for radiographic evaluation of the craniofacial trauma patient. Historically, plain radiographs were ordered to evaluate facial and cervical fractures. This modality has been outdated due to the superior image quality and three-dimensional anatomic relationships afforded by CT. CT scans provide reliable, accurate information that aids in surgical planning, and have been shown to be more cost-effective than radiographic series.
CT images should include the frontal bone, frontal sinus, orbital and nasal regions, midface, and mandible, including the temporomandibular joints. If there is tooth involvement in any identified fracture on CT, a Panorex image should be obtained to assess tooth and tooth root injury. This is the only situation in craniofacial trauma where thin-cut, multiplanar CT imaging is not the gold standard for bony injury. Patients with multiple injuries cannot be sent unmonitored for radiographic evaluation. Three-dimensional CT scans can greatly aid in operative planning of complex craniofacial trauma, and will likely play an increasing role in the imaging of craniofacial trauma as this technology becomes more widely available.
In most cases, CT evaluation of the craniofacial trauma patient supplements and confirms, but never replaces, the findings of a thorough clinical examination. A review of both bone and soft-tissue CT windows should be promptly completed, and the specific areas with radiographically identified fractures reexamined. This is particularly useful in cases of suspected intraocular muscle entrapment as discussed later.
General Considerations
After completion of the primary survey, secondary survey, and radiographic imaging, soft-tissue injuries of the face may be definitively treated. Lacerations are thoroughly inspected and accessed for depth and direction. Any foreign bodies are identified, the level of wound contamination is assessed, and damage to deeper structures, such as muscles, nerves, or bone, is identified. Tetanus prophylaxis is essential, and is administered according to the guidelines of the American College of Surgeons (Table 2). The goals of initial treatment are the cleansing of wounds, debridement of devitalized tissue, evacuation of hematomas, and tension-free reapproximation of wound edges. Puncture wounds are managed by thorough irrigation and debridement without formal closure. Many soft-tissue injuries can be treated in the emergency department, provided the patient is hemodynamically stable, wounds are not severely contaminated, and there is no threat of airway compromise. If any of these criteria are not met, if fractures are present, or if the patient is uncooperative (i.e., pediatric patients), operative repair in a formal surgical theater is warranted.
Anesthesia
For most soft-tissue injuries, local anesthesia is adequate to achieve debridement and closure. Before injecting a local anesthetic, a complete motor and sensory neurological examination of the face must be documented. This not only serves medico-legal purposes, but also conveys important information to other specialists that may participate in subsequent patient care outside of the emergency department.
Local anesthesia can be administered via direct field injection, or through anatomical nerve blocks. Topical application of local anesthesia to the laceration may provide a level of analgesia that allows subsequent injection with minimal discomfort. Direct field injections, while requiring less technical skill, distort anatomy, making precise closure difficult, and often result in incomplete or fleeting anesthesia due to imprecise infiltration. Therefore, important anatomical landmarks, including the vermillion border and brow line, should be marked before local anesthetic infiltration so that these crucial areas can be accurately repaired (Fig. 2). These regions benefit greatly from trigeminal nerve blocks and therefore avoid local soft-tissue distortion.
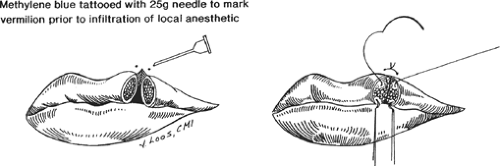 Fig. 2. Marking the vermilion border before local infiltration of anesthetic aids precise repair of lacerations of the lip. |
Anatomical nerve blocks require less anesthetic volume (typically 2 mL) and allow for accurate tissue reapproximation because they do not distort anatomic landmarks. Nerve blocks of the supraorbital, supratrochlear, infraorbital, and mental areas are effective and easily performed (Fig. 3). When performing nerve blocks, injection must be immediately stopped and the needle withdrawn if the patient experiences sharp pain in the distribution of the nerve being anesthetized. This indicates direct intraneural injection, which can lead to permanent denervation. The ear is a notoriously difficult area to anesthetize due to multiorigin and redundant innervation. A great auricular block is effective for the inferior ear and superior mandible areas. Complete ear anesthesia requires local injection in a diamond/ring pattern circumferentially around the ear.
Table 2 Recommendations for Tetanus Prophylaxis of the Committee on Trauma, American College of Surgeons | ||
|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree