Esophageal Perforation
Soji Ozawa
Masaki Kitajima
Introduction
There have been many reports of esophageal perforation since the Dutch physician Hermann Boerhaave reported the case of the Grand Admiral of Holland who died as a result of a “spontaneous” rupture of the esophagus in 1724. According to Barrett, J.R. Meyer of Berlin was the first to recognize this disease prior to death. Barrett made the first early diagnosis and performed the first surgical repair in 1946. Early recognition later improved, antibiotics became more widely available, and mortality rates decreased. As various technologies advanced, instrumental perforation became more common, and the definitions of perforation became blurred. Diagnosis remains difficult, methods of management continues to be controversial, and treatment outcome depends on early diagnosis. This chapter describes the etiology, pathophysiology, and treatment of esophageal perforation as a full-thickness tear in the esophageal wall.
Etiology
Iatrogenic
Instrumentation
Instrumental perforation of the esophagus is the most common. Flynn et al. reported that 48% of ruptures are iatrogenic, 33% are caused by external trauma, and only 8% are spontaneous. Rigid endoscopy is associated with a higher incidence of perforation (0.11%) than flexible endoscopy (0.03%).
The most common site of perforation during endoscopy is at the cricopharyngeus, but when esophageal dilatation is performed, the site of perforation is at the stricture of the original disease. The American Society of Gastrointestinal Endoscopy Survey estimated that the incidence of esophageal perforation by bougienage and metal-olive dilators is 0.4% and 0.6%, respectively. Nair et al. reported that pneumatic dilatation for achalasia is associated with an incidence of perforation of 1.7%. Both higher inflation pressure and previous pneumatic dilatation increase the risk.
Endoscopic thermal therapy of gastrointestinal bleeding is associated with an incidence of perforation of 1% to 2%. In contrast to other endoscopic therapies, perforation after endoscopic variceal sclerotherapy occurs 5 to 7 days postoperatively (1% to 6%), and it results from transmural necrosis of the esophageal wall. Perforation is also reported to occur as a result of pinching of the esophageal mucosa between the endoscope and the overtube during endoscopic variceal ligation.
Endoscopic LASER therapy for esophageal cancer is also associated with esophageal perforation. It usually occurs during the procedure or 1 week later. Endoscopic photodynamic therapy for esophageal cancer was found to be associated with esophageal perforation (4.6%) in a multicenter phase III trial, and bipolar electrocoagulation is associated with a similar incidence of esophageal perforation. Perforation has been reported to occur in 5% to 25% of patients after esophageal stenting; however, expandable metallic stents are much safer than rigid plastic stents. Endoscopic ultrasound is associated with a perforation rate of 0.1%.
Perforation due to nonendoscopic instrumentation is rare. Endotracheal tube intubation sometimes results in perforation of the cervical esophagus.
Surgical Injury
Esophageal perforation sometimes occurs after vagotomy, radical pneumonectomy, Heller myotomy, antireflux surgery, submucosal tumor encleation, thyroid resection, tracheostomy, thoracic aneurysm repair, mediastinoscopy, insertion of a thoracotomy tube, spine surgery, and so forth.
Boerhaave’s Syndrome
Boerhaave’s syndrome has also been called “barogenic perforation” and “postemetic perforation.” Although the term “spontaneous esophageal rupture” is also used for Boerhaave’s syndrome, truly spontaneous cases are rare, because most cases occur after severe vomiting.
Although Boerhaave’s syndrome is classically postemetic, other causes of a sudden rise in intraesophageal pressure, including weight lifting, laughing, hyperemesis gravidarum, and seizures, can result in “spontaneous” rupture. Spontaneous rupture almost always occurs on the left side of the distal third of the esophagus. A review of l84 cases of spontaneous rupture revealed that the vast majority (90%) were in the lower third of the esophagus, with 8% occurring in the middle third and 2% in the upper third. Other large series have confirmed this site distribution. Most tears occur along the longitudinal axis, and they vary from 0.6 to 8.9 cm in length. The mucosal tear is often longer than the muscle tear, which is important to repair the esophageal wall completely. The reason for the predilection for the lower third of the esophagus on the left side remains unclear, but weakening of the wall at the sites of entry of nerves and vessels, lack of adjacent supporting structures, the vertical orientation of the longitudinal muscle bundles, and the anterior angulation of the esophagus are all regarded as contributing factors.
Trauma
The incidence of esophageal perforation as a result of trauma is 8% to 15.3%. Trauma-related perforation is divided into two types: blunt trauma and penetrating trauma. The incidence of esophageal perforation as a result of blunt trauma is very low (0.001%). The most common cause is chest injury by a steering wheel in a traffic accident. The intraesophageal pressure rises rapidly and causes perforation of the hypopharyngoesophageal junction. Esophageal perforation sometimes occurs as a result of intratracheal injury, fracture of the second rib, fracture of the cervical spine, and hyperextension of the neck.
Penetrating injuries produced by knives and bullets are more common. The incidence of esophageal perforation by penetrating injuries is 11% to 17%. Perforation is more common in the cervical esophagus than in the thoracic esophagus. The overall mortality rate remains high (15% to 40%).
Tumor
Locally advanced esophageal cancer is sometimes associated with an esophageal fistula to the mediastinum, an esophagotracheal, or an esophagobronchial fistula.
Foreign Body
Foreign body ingestion and endoscopic removal are sometimes associated with esophageal perforation (7% to 14%). The site of the perforation is at physiological narrowing. Penetrating injuries by sharp or pointed metallic objects, animal or fish bones, and toothpicks can cause perforation. Pressure
necrosis by foreign body, such as a coin, is a rare cause of perforation except in children. The initial clinical manifestations of esophageal perforation may occur within 48 hours or as late as 2 weeks.
necrosis by foreign body, such as a coin, is a rare cause of perforation except in children. The initial clinical manifestations of esophageal perforation may occur within 48 hours or as late as 2 weeks.
Caustic Injury
Ingestion of caustic substances can cause devastating injury to the esophagus. Liquefaction necrosis of the esophageal wall after ingestion of lye causes the wall of the esophagus to degenerate and results in perforation. The perforation occurs as a result of inflammation, vascular thrombosis, ulceration, and necrosis of the esophageal wall 3 to 5 days after ingestion.
Drug-Induced
The drugs that are the most common cause of esophageal perforation are tetracycline preparations, potassium chloride, quinidine, and nonsteroidal anti-inflammatory drugs. Sustained-release formulations are more likely to cause injury. Long-term contact between drugs and the esophageal mucosa can cause esophageal perforation.
Infection
Infectious esophagitis, including Candida esophagitis, herpes simplex viral esophagitis, and cytomegaloviral esophagitis, usually develops in immunocompromised hosts. Although infectious esophagitis is a rare cause of esophageal perforation, there have been reports of spontaneous perforation associated with Candida esophagitis and herpes simplex viral esophagitis.
Other Causes
Barrett’s ulcer and ulcerative esophagitis with Zollinger–Ellison syndrome sometimes cause perforation. Aneurysms and aberrant right subclavian artery also sometimes result in esophageal rupture.
Pathophysiology
Because the esophagus lacks a serosal layer anatomically, it is susceptible to perforation than other gastrointestinal organs. Once perforation of the thoracic esophagus occurs, gastric contents, saliva, bile, pancreatic juice, etc., enter the mediastinum and necrotizing mediastinitis develops. Because of the anatomical location of the esophagus in the mediastinum, perforation of the midesophagus results in changes in the right pleural cavity, while perforation of the distal esophagus results in changes in the left pleural cavity. Cervical perforation is often associated with a localized periesophageal abscess. Thoracic perforations tend to disseminate mediastinal contamination of fluids and bacteria because of the negative intrathoracic pressure. Polymicrobial invasion by bacteria, such as Staphylococcus, Pseudomonas, Streptococcus, and Bacteroides, occurs within 12 hours, and the infection may result in fluid sequestration, sepsis, and death. If untreated, intra-abdominal perforation becomes complicated by peritonitis, shock, and death. If the perforation is localized, sepsis and shock may not develop, and this subacute state (24 hours to 2 weeks) is often accompanied by chest pain and dyspnea.
The diagnosis of esophageal perforation often depends on the radiographic findings. Emergency posteroanterior and lateral chest and upright abdominal X-rays should be obtained. A lateral X-ray of the neck is useful when there is suspicion of the perforation of the cervical esophagus. Typical X-ray findings include pleural effusion, pneumomediastinum, subcutaneous emphysema, hydrothorax, and hydropneumothorax. Chest X-ray appears normal in the early phase. Emphysema becomes manifested by 1 hour after the perforation, and pleural effusion is detected several hours after the perforation. The chest X-ray findings have been reported to be abnormal in 80% of instrumental perforation cases. Pneumomediastinum is present in 60% of the cases. For anatomical reasons, perforation of the midthoracic esophagus is associated with right-sided pleural effusion, whereas the perforation of the distal thoracic esophagus is associated with left-sided pleural effusions.
Esophagography with diatrizoate meglumine and diatrizoate sodium (Gastrografin) should follow plain radiography. The examination should be performed with the patient in the upright, supine, and lateral decubitus positions. If the patient is at high risk for aspiration, contrast medium angiography is the medium of first choice to prevent induction of pulmonary edema by Gastrografin. Barium can be used if special care is taken to prevent mediastinitis and prolonged retention. The detection rate is 60% for cervical perforation and 90% for surgically confirmed perforations. The false-negative rate as a result of spasm, tissue edema, and other factors is 10% to 36%.
Computer tomography (CT) is useful in cases that are difficult to diagnose. Significant CT findings include air in the mediastinal soft tissue around the esophagus, abscess cavities adjacent to the esophagus, and communication of the air-filled esophagus with adjacent mediastinal or paramediastinal air-fluid collections.
Endoscopy is useful as a highly accurate method of diagnosis in difficult cases. Although caution is required, endoscopic examination of the entire esophagus is necessary to accurately diagnose the location, length, and number of perforations and preexisting diseases of the esophagus and the stomach. The endoscopic examination should be performed under general anesthesia in the operating room by a skilled endoscopist. Diagnostic thoracentesis is also used, and significant findings include the presence of an acidic pH, elevated salivary amylase level, purulent foul-smelling material, and undigested food.
The goal of treatment must be to prevent further contamination thorough the perforation, to eliminate infection produced by contamination, to restore the integrity and continuity of the gastrointestinal tract, and to restore and maintain adequate nutrition. There are two major types of treatment: surgical and nonsurgical. Surgical treatment includes primary closure, reinforced closure, closure and drainage, resection, drainage alone, T-tube drainage, exclusion and diversion, and intraluminal stents. The surgical approaches include conventional thoracotomy or laparotomy and minimally invasive thoracoscopy or laparoscopy. The principles of surgical treatment are debridement of all infected and necrotic tissue, secure closure of the perforation with an appropriate means of preventing leakage, correction or elimination of distal obstruction, and drainage of contaminated and infected areas. An enteral nutrition route, such as a jejunostomy, should be added for nutritional support to any surgical method.
Surgical Approaches
The surgical approach depends on the location of the perforation. When the perforation is in the cervical esophagus, the esophagus can usually be exposed through a left oblique incision in the neck. If the perforation is in the upper two-thirds of the thoracic esophagus, it can be approached through a right posterolateral thoracotomy in the fourth or fifth intercostal space. The perforation of the lower third of the thoracic esophagus can be approached through a left posterolateral thoracotomy in the sixth or seventh intercostal space. If the perforation is in the abdominal esophagus,
the esophagus can be approached through an upper midline laparotomy. Minimally invasive approaches, such as thoracoscopic or laparoscopic approaches, have recently been reported. Although simple primary closure and primary closure reinforced with gastric fundus are possible, it seems difficult to completely debride all the infected and necrotic tissues and to secure closure of the perforation by reinforcing it with muscle, such as with a pedicled intercostal muscle flap. The minimally invasive approaches, therefore, may be limited to early and uncontaminated perforations of the esophagogastric junction.
the esophagus can be approached through an upper midline laparotomy. Minimally invasive approaches, such as thoracoscopic or laparoscopic approaches, have recently been reported. Although simple primary closure and primary closure reinforced with gastric fundus are possible, it seems difficult to completely debride all the infected and necrotic tissues and to secure closure of the perforation by reinforcing it with muscle, such as with a pedicled intercostal muscle flap. The minimally invasive approaches, therefore, may be limited to early and uncontaminated perforations of the esophagogastric junction.
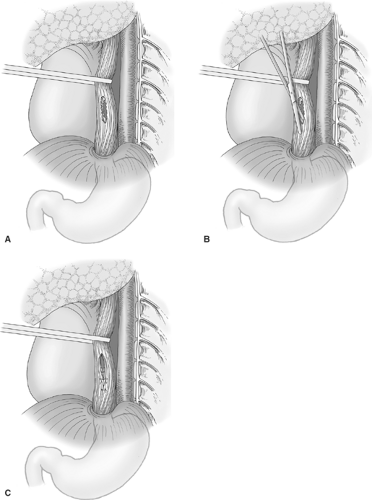 Fig. 1. A: Repair of perforation in the lower third of the intrathoracic esophagus. The perforation of the mucosa is usually more extensive than the laceration of the muscle layer. B: The muscular layer is incised superiorly and inferiorly to allow visualization of the extent of mucosal defect. C: Closure of the esophageal mucosa on healthy tissue is completed, and followed by closure of the muscular layer.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|