Patient Story
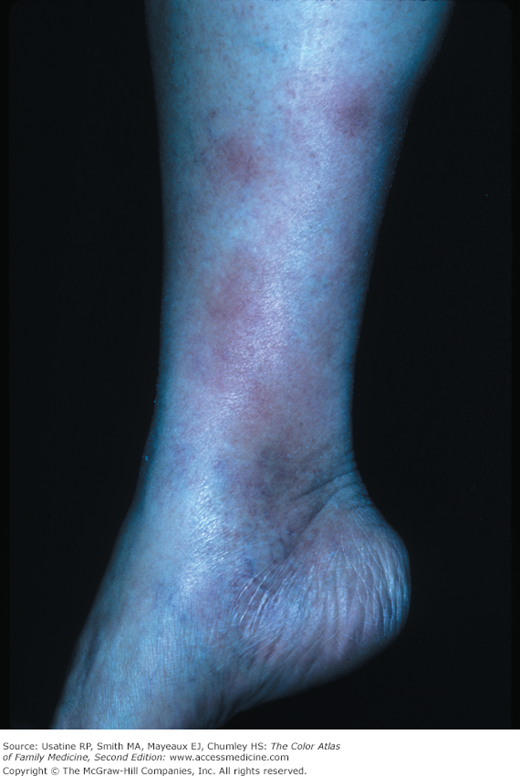
A young woman presented to the office with several days of overall malaise, fever, and sore throat. At the time of presentation she noted some painful bumps on her lower legs, and denied trauma (Figure 178-1). No history of recent cough or change in bowel habits has been reported. The patient had no chronic medical problems, took no medications and had no known drug allergies. Her temperature was slightly elevated, but other vitals were normal. On examination, her oropharynx revealed tonsillar erythema and exudates. Bilateral lower extremities were spotted with slightly-raised, tender, erythematous nodules that varied in size from 2 to 6 cm. Rapid strep test was positive and she was diagnosed clinically with erythema nodosum (EN) secondary to group A β-hemolytic Streptococcus. She was treated with penicillin and NSAIDs, and was advised temporary bedrest. She experienced complete resolution of the EN within 4 weeks.
Introduction
Epidemiology
- Erythema nodosum occurs in approximately 1 to 5 per 100,000 persons.1 It is the most frequent type of septal panniculitis (inflammation of the septa of fat lobules in the subcutaneous tissue).2
- EN tends to occur more often in women, with a male-to-female ratio of 1:4.5 in the adult population, generally during the second and fourth decades of life (Figures 178-1, 178-2, and 178-3).3
- In 1 study, an overall incidence of 54 million people worldwide was cited in patients older than 14 years of age.4
- In the childhood form, the female predilection is not seen.
Etiology and Pathophysiology
- Most EN is idiopathic (Figures 178-3 and 178-4). Although the exact percentage is unknown, 1 study estimated that 55% of EN is idiopathic.5 This may be influenced by the fact that EN may precede the underlying illness. The distribution of etiologic causes may be seasonal.6 Identifiable causes can be infectious, reactive, pharmacologic, or neoplastic.
- Histologic examination is most useful in defining EN. Defining characteristics of EN are a septal panniculitis without presence of vasculitis. That this pattern develops in certain areas of skin may be linked to local variations in temperature and efficient blood drainage.
- Septal panniculitis begins with polymorphonuclear cells infiltrating the septa of fat lobules in the subcutaneous tissue. It is thought that this is in response to existing immune complex deposition in these areas.7 This inflammatory change consists of edema and hemorrhage which is responsible for the nodularity, warmth, and erythema.
- The infiltrate progresses from predominantly polymorphonuclear cells, to lymphocytes, and then histiocytes where fibrosis occurs around the lobules. There may be some necrosis though minimal as complete resolution without scarring is the typical course.
- The histopathologic hallmark of EN is the Miescher radial granuloma. This is a small, well-defined nodular aggregate of small histiocytes around a central stellate or banana-shaped cleft.
Risk Factors
- Group A β-hemolytic streptococcal pharyngitis has been linked to EN (Figure 178-1). A retrospective study of 129 cases of EN over several decades reports 28% had streptococcal infection.5
- Nonstreptococcal upper respiratory tract infections may also play a role.1
- Historically, tuberculosis (TB) was a common underlying illness with EN, but TB is now a rare cause of EN in developed countries. There are reports of EN occurring in patients receiving the bacille Calmette-Guérin vaccination.8 In developed countries, sarcoidosis is more commonly found. One study estimates sarcoidosis as being the cause of 11% of EN cases (Figure 178-2).5,7
- EN occurs in 3% of all patients with coccidiomycosis,9 and approximately 4% of patients with histoplasmosis.10
- EN is less frequently associated with other infections agents, including Yersinia gastroenteritis, Salmonella, Campylobacter, toxoplasmosis, syphilis, amebiasis, giardiasis, brucellosis, leprosy, Chlamydia, Mycoplasma, Brucella, hepatitis B (infection and vaccine), Epstein-Barr virus, and Bartonella.4,11
- When the EN rash occurs with hilar adenopathy, the entity is called Lofgren syndrome. Lofgren syndrome in TB represents primary infection. A more common cause of Lofgren syndrome is sarcoidosis.7
- The literature reports that EN is seen in patients with inflammatory bowel diseases. It is usually prominent around the time of GI flare-ups, but may occur before a flare. Most sources report a greater association between Crohn disease and EN than between ulcerative colitis and EN. Other chronic diseases associated with EN include Behçet disease and Sweet syndrome.11
- Some debate exists over causality from pregnancy and oral contraceptives in the occurrence of EN.
- Besides oral contraceptives, medications implicated as causing EN are antibiotics including sulfonamides, penicillins, and bromides. However, the antibiotics may have been prescribed for the underlying infection that had caused EN.11

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree