Erectile Dysfunction
KEY CONCEPTS
![]() The incidence of erectile dysfunction is low in men younger than 40 years of age. The incidence increases as men age, likely as a result of concurrent medical conditions that impair the vascular, neurologic, psychogenic, and hormonal systems necessary for a normal penile erection.
The incidence of erectile dysfunction is low in men younger than 40 years of age. The incidence increases as men age, likely as a result of concurrent medical conditions that impair the vascular, neurologic, psychogenic, and hormonal systems necessary for a normal penile erection.
![]() Many commonly used drugs have sympatholytic, anticholinergic, sedative, or antiandrogenic effects that may exacerbate or contribute to the development of erectile dysfunction. Clinicians should be familiar with these agents and be prepared to make adjustments in drug regimens to minimize adverse effects of these drugs on a patient’s erectile function.
Many commonly used drugs have sympatholytic, anticholinergic, sedative, or antiandrogenic effects that may exacerbate or contribute to the development of erectile dysfunction. Clinicians should be familiar with these agents and be prepared to make adjustments in drug regimens to minimize adverse effects of these drugs on a patient’s erectile function.
![]() The first step in clinical management of erectile dysfunction is to identify and, if possible, reverse the underlying causes. Risk factors for erectile dysfunction, including hypertension, diabetes mellitus, smoking, and chronic ethanol abuse, should be addressed and minimized.
The first step in clinical management of erectile dysfunction is to identify and, if possible, reverse the underlying causes. Risk factors for erectile dysfunction, including hypertension, diabetes mellitus, smoking, and chronic ethanol abuse, should be addressed and minimized.
![]() Specific treatments for erectile dysfunction include vacuum erection devices (VEDs), pharmacologic treatments, psychotherapy, and surgery. Of these, phosphodiesterase inhibitors are the medications of first choice.
Specific treatments for erectile dysfunction include vacuum erection devices (VEDs), pharmacologic treatments, psychotherapy, and surgery. Of these, phosphodiesterase inhibitors are the medications of first choice.
![]() The ideal treatment of erectile dysfunction should have a fast onset, be effective, be convenient to administer, be cost effective, have a low incidence of serious adverse effects, and be free of serious drug interactions.
The ideal treatment of erectile dysfunction should have a fast onset, be effective, be convenient to administer, be cost effective, have a low incidence of serious adverse effects, and be free of serious drug interactions.
![]() Specific treatment is first initiated with the least invasive forms of treatment, including VEDs or oral phosphodiesterase inhibitors, followed by intracavernosal injections or intraurethral inserts, and finally by surgical insertion of a penile prosthesis.
Specific treatment is first initiated with the least invasive forms of treatment, including VEDs or oral phosphodiesterase inhibitors, followed by intracavernosal injections or intraurethral inserts, and finally by surgical insertion of a penile prosthesis.
![]() VEDs can have a slow onset of action (30 minutes) and are not discreet; therefore, they are most effective for a couple in a stable relationship.
VEDs can have a slow onset of action (30 minutes) and are not discreet; therefore, they are most effective for a couple in a stable relationship.
![]() Although phosphodiesterase inhibitors are convenient and effective regardless of the etiology of erectile dysfunction, they fail in 30% to 40% of patients. Also, phosphodiesterase inhibitors are contraindicated in patients taking any dosage formulation of nitrate.
Although phosphodiesterase inhibitors are convenient and effective regardless of the etiology of erectile dysfunction, they fail in 30% to 40% of patients. Also, phosphodiesterase inhibitors are contraindicated in patients taking any dosage formulation of nitrate.
![]() Testosterone supplementation should be reserved for patients with primary or secondary hypogonadism who have erectile dysfunction as a consequence of a decreased libido. Testosterone supplementation should not be used by patients with erectile dysfunction who have normal serum testosterone levels.
Testosterone supplementation should be reserved for patients with primary or secondary hypogonadism who have erectile dysfunction as a consequence of a decreased libido. Testosterone supplementation should not be used by patients with erectile dysfunction who have normal serum testosterone levels.
![]() Although intracavernosal injections and intraurethral pellets of alprostadil are effective independent of the etiology of erectile dysfunction, they fail in one third of patients. To self-administer medication by these routes, patients require training to minimize administration-related adverse effects.
Although intracavernosal injections and intraurethral pellets of alprostadil are effective independent of the etiology of erectile dysfunction, they fail in one third of patients. To self-administer medication by these routes, patients require training to minimize administration-related adverse effects.
The National Institutes of Health Consensus Development Panel on Impotence defines erectile dysfunction as the persistent failure to achieve a penile erection to allow for satisfactory sexual intercourse.1 A persistent failure refers to erectile dysfunction for a minimum of 3 months.2 Patients may refer to it as impotence.
Erectile dysfunction must be distinguished from disorders of libido, ejaculatory disorders, and infertility, which are caused by different pathophysiologic mechanisms and are treated with alternative agents (Table 66-1). A patient may suffer from one or more disorders of sexual dysfunction. For example, an elderly man with primary hypogonadism may suffer from decreased libido and erectile dysfunction. Diagnosis of the type of sexual disorder that a patient has is a key to initiating the most appropriate treatment.
TABLE 66-1 Types of Sexual Dysfunction in Men
EPIDEMIOLOGY
![]() The incidence of erectile dysfunction is low in men younger than 40 years of age but increases as men age.3–5 The Massachusetts Male Aging Study, a cross-sectional survey of a random sample of 1,290 men in the Boston area, was conducted during the period from 1987 to 1989. The study reported an overall prevalence of 52% for any degree of erectile dysfunction in men aged 40 to 70 years, with an age-related increase in incidence ranging from 12.4% in men aged 40 to 49 years, up to 46.4% in men aged 60 to 69 years.1,3 In the more recent Health Professional Follow-Up Study of more than 31,000 male health professionals aged 53 to 90 years, the prevalence of erectile dysfunction was 33%.4 Interestingly, although the prevalence of erectile dysfunction increases with patient age, many patients fail to seek medical treatment.5
The incidence of erectile dysfunction is low in men younger than 40 years of age but increases as men age.3–5 The Massachusetts Male Aging Study, a cross-sectional survey of a random sample of 1,290 men in the Boston area, was conducted during the period from 1987 to 1989. The study reported an overall prevalence of 52% for any degree of erectile dysfunction in men aged 40 to 70 years, with an age-related increase in incidence ranging from 12.4% in men aged 40 to 49 years, up to 46.4% in men aged 60 to 69 years.1,3 In the more recent Health Professional Follow-Up Study of more than 31,000 male health professionals aged 53 to 90 years, the prevalence of erectile dysfunction was 33%.4 Interestingly, although the prevalence of erectile dysfunction increases with patient age, many patients fail to seek medical treatment.5
Erectile dysfunction is sometimes assumed to be a symptom of the aging process in men. However, more likely it results from concurrent medical conditions of the patient (e.g., hypertension, arteriosclerosis, hyperlipidemia, diabetes mellitus, or psychiatric disorders) or from medications that patients may be taking for these diseases.6,7 For example, up to 50% of patients with diabetes mellitus develop erectile dysfunction, and medications such as β-blockers are associated with a high incidence of erectile dysfunction.
PHYSIOLOGY OF A NORMAL PENILE ERECTION
A normal penile erection requires full functioning of several physiologic systems: vascular, nervous, and hormonal. The patient also must be psychologically receptive to sexual stimuli.8,9
Vascular System
The penis comprises two corpora cavernosa on the dorsal side and one corpus spongiosum on the ventral side. The corpus spongiosum surrounds the urethra and forms the glans penis. The corpora are composed of multiple interconnected sinuses, which can fill with blood to produce an erection. The corpora cavernosa are encased by the tunica albuginea, a fibrous tissue membrane, which has limited distensibility. In the flaccid state, arterial flow into and venous outflow from the corpora are balanced. During the erectile phase, arterial blood flow increases and blood fills the sinusoids within the corpora, which causes penile swelling and elongation. The erection is prolonged by a decrease in venous outflow from the corpora, which is caused by compression of subtunical venules against the tunica albuginea by the swollen corpora (Fig. 66-1).
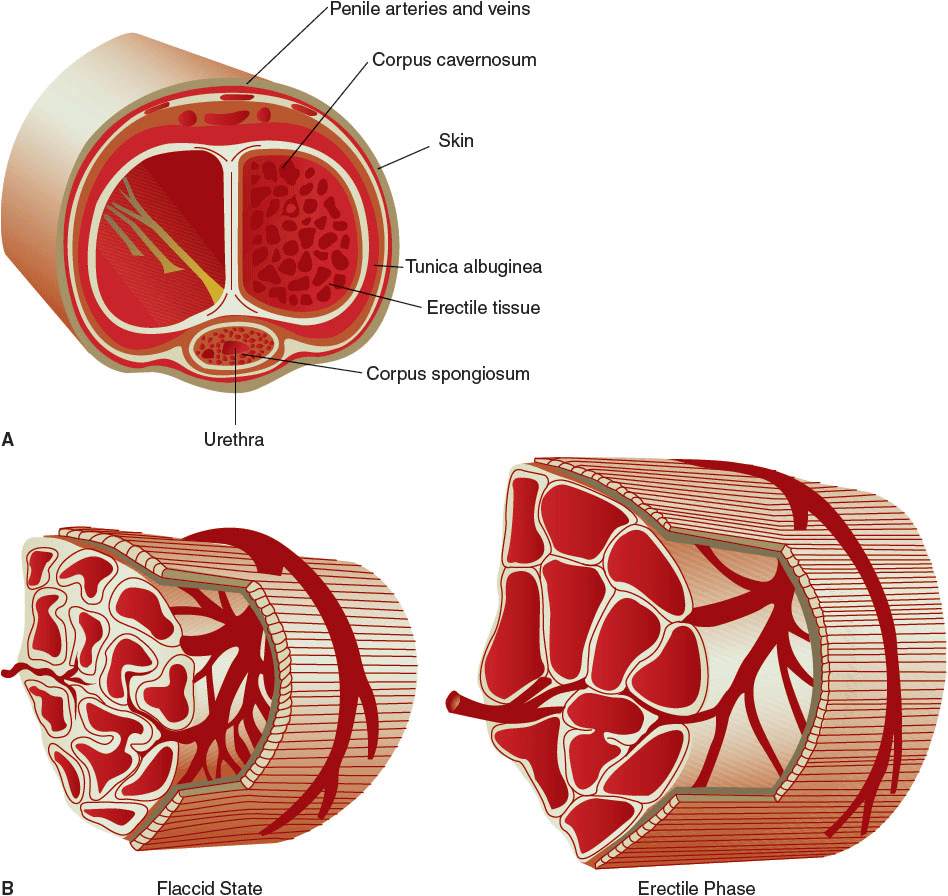
FIGURE 66-1 Microanatomy of and vascular changes in the penis in flaccid and erect states. In the flaccid state, arterial flow into and venous outflow from the corpora are balanced. During the erectile phase, arterial blood flow increases and blood fills the sinusoids within the corpora, causing penile swelling and elongation. The erection is prolonged by a decrease in venous outflow from the corpora, which is caused by compression of subtunical venules by the swollen corpora. (From Walsh PC, ed. Campbell’s Urology, 8th ed. Philadelphia, PA: WB Saunders; 2002:1595, 1697.)
Arterial flow into the corpora is enhanced by acetylcholine-mediated vasodilation. Acetylcholine indirectly enhances arterial flow to the corpora and increases sinusoidal filling of the corporal tissue. That is, acetylcholine is a coneurotransmitter, which works along with other nonpeptidergic intracellular neurotransmitters—including cyclic guanosine monophosphate (cGMP), cyclic adenosine monophosphate (cAMP), or vasoactive intestinal polypeptide—to produce vasodilation. In effect, cGMP and cAMP are secondary messengers that direct desired effects in target tissues.
Specifically, acetylcholine produces an erection probably through two different pathways. Through one pathway, in the presence of sexual stimulation to genital tissue, acetylcholine enhances the production of nitric oxide by endothelial cells and-nonadrenergic–noncholinergic neurons. Nitric oxide enhances the activity of guanylate cyclase, which increases the conversion of cyclic guanosine triphosphate to cGMP. cGMP decreases intracellular calcium concentrations in smooth muscle cells of penile arteries and cavernosal sinuses. As a result, smooth muscle relaxation occurs, which enhances arterial blood flow to and blood filling of the corpora.9 An erection results.
In an alternative pathway, acetylcholine or prostaglandin E enhances the activity of adenyl cyclase, which increases the conversion of cyclic adenosine triphosphate to cAMP, a potent muscle relaxant. Similar to cGMP, cAMP decreases intracellular calcium concentrations to produce smooth muscle relaxation in cells of the arteries and cavernosal sinuses. Arterial blood flow to and blood filling of the corpora are enhanced, and a penile erection results.9
Nervous System and Psychogenic Stimuli
Some erections are mediated by a sacral nerve reflex arc (e.g., erections can occur while the patient is sleeping). However, in the conscious patient, sensory sexual stimulation mediates erections via the CNS. That is, when a patient sees an attractive partner, hears sweet words, smells a particular scent, or tastes or touches a pleasant object, these situations can result in an erection. In this case, the patient’s brain processes this information and the nervous impulse is carried down the spinal cord to peripheral cholinergic nerves that innervate the vascular supply to the corpora, resulting in an erection.
The medial preoptic area of the hypothalamus is thought to be that portion of the brain responsible for integrating external stimuli. Here dopamine exerts a proerectogenic effect, whereas, α2-adrenergic stimulation causes the penis to become and/or remain flaccid. After moving down the spinal cord, stimulatory nerve impulses travel to the penis by efferent peripheral nerves, including inhibitory sympathetic neurons (T11–L2), proerectogenic parasympathetic neurons (S2–S4), and proerectogenic somatic neurons (S2–S4).
In summary, acetylcholine produces an erection by working along with other coneurotransmitters, including cGMP and cAMP. Thus, an erection is mediated neurologically, maintained by arterial blood filling of the corpora, and sustained by occlusion of venous outflow from the corpora.
Detumescence, or the progression of an erect penis to a flaccid state, results from the actions of norepinephrine, which contracts vascular smooth muscle to decrease arterial inflow to the corpora and contracts sinusoidal tissue in the corpora. As a result, venous outflow from the corpora increases.
Hormonal System
Testosterone is principally produced by the testes at a daily rate of 4 to 8 mg. Production follows a circadian pattern with highest blood levels in the morning and lowest levels in the evening. Physiologically active (free) testosterone comprises only 2% of circulating blood levels. About 50% to 60% of testosterone in the bloodstream is tightly bound to sex hormone-binding globulin and is inactive. The rest of circulating testosterone is reversibly bound to albumin; this portion of testosterone is in equilibrium with the free fraction.
Testosterone stimulates libido (sexual drive) and increases muscle mass in males. In some target cells with 5-α reductase, testosterone is activated to dihydrotestosterone. Dihydrotestosterone, which is more potent than testosterone, stimulates prostate gland growth, increases facial and body hair, induces baldness, and causes acne. In adipose tissue, a small portion of testosterone is converted to estradiol which can lead to gynecomastia.
Beginning at age 40 years, men experience a gradual decrease in testicular production of testosterone, with an associated decrease in muscle mass and sexual function.10 The Massachusetts Male Aging Study reported that 6% to 12% of elderly males had symptoms of hypogonadism.11
Within the normal physiologic serum total testosterone concentration range (normal, 300–1,100 ng/dL; 10.4–38.2 nmol/L), sexual drive is usually normal. However, because of variability in circulating levels of sex hormone-binding globulin, a patient’s serum concentration of testosterone should always be interpreted in the context of the patient’s symptoms and physical exam findings. To confirm hypogonadism when the serum total testosterone concentration is equivocal, the clinician should obtain a serum-free (bioavailable) testosterone level.
The relationship between erectile dysfunction and serum testosterone levels is complicated. Patients with normal serum testosterone levels may have erectile dysfunction, and patients with subnormal serum testosterone levels may have normal sexual function.5 When a patient has hypogonadism and libido is decreased, a patient may not develop erections. In this case, erectile dysfunction is considered secondary to a decreased libido.
PATHOPHYSIOLOGY
Erectile dysfunction can result from any single abnormality or combination of abnormalities of the four systems necessary for a normal penile erection. Vascular, neurologic, or hormonal etiologies of erectile dysfunction are collectively referred to as organic erectile dysfunction. Approximately 80% of patients with erectile dysfunction have the organic type. Patients who do not respond to psychogenic stimuli and have no organic cause for dysfunction have psychogenic erectile dysfunction.
Diseases that compromise vascular flow to the corpora cavernosum (e.g., peripheral vascular disease, arteriosclerosis, and essential hypertension) are associated with an increased incidence of erectile dysfunction. Diseases that impair nerve conduction to the brain (e.g., spinal cord injury or stroke) or conditions that impair peripheral nerve conduction to the penile vasculature (e.g., diabetes mellitus) can result in erectile dysfunction.7
Diseases associated with hypogonadism, primary or secondary, result in subphysiologic levels of testosterone, which cause diminished sexual drive (decreased libido) and secondary erectile dysfunction. Primary hypogonadism can be associated with the normal aging process in men or surgical removal of the testes for treatment of prostate or testicular cancer. Secondary hypogonadism may result from hypothalamic or pituitary disorders of luteinizing hormone–releasing hormone or luteinizing hormone, respectively; or elevated prolactin levels, which can be associated with pituitary tumors or can occur in patients with chronic renal failure.
Patients must be in the proper mental frame of mind to be receptive to sexual stimuli. Patients who suffer from malaise, have reactive depression or performance anxiety, are sedated, have Alzheimer’s disease, have hypothyroidism, or have mental disorders commonly complain of erectile dysfunction. In most studies, patients with psychogenic erectile dysfunction generally exhibit a higher response rate to various interventions than do patients with organic erectile dysfunction because the former have less severe disease.
Social habits of patients have been linked to erectile dysfunction. The vasoconstrictor effect of cigarette smoking may compromise blood flow to the corpora and decrease cavernosal filling. Excessive ethanol intake may lead to androgen deficiency, peripheral neuropathy, or chronic liver disease, all of which can contribute to erectile dysfunction.
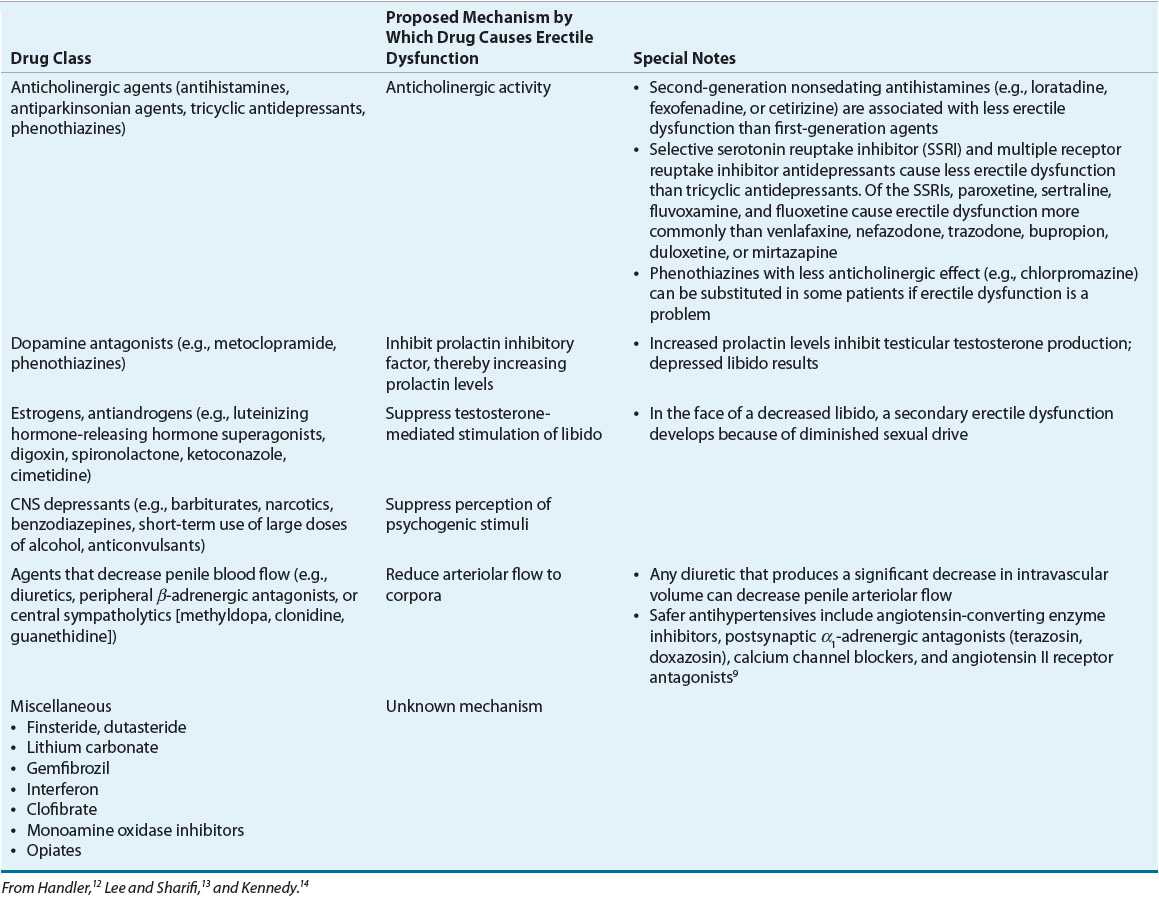
![]() Medications may cause erectile dysfunction through similar pathophysiologic mechanisms (Table 66-2).12–14 Medications are estimated to be responsible for approximately 10% to 25% of cases of erectile dysfunction.
Medications may cause erectile dysfunction through similar pathophysiologic mechanisms (Table 66-2).12–14 Medications are estimated to be responsible for approximately 10% to 25% of cases of erectile dysfunction.
TABLE 66-2 Medication Classes That Can Cause Erectile Dysfunction
DIAGNOSIS
With the availability in the late 1990s of effective medications for erectile dysfunction independent of the etiology, diagnostic evaluation of erectile dysfunction became streamlined. Key assessments include a description of the severity of erectile dysfunction, complete medical, psychosocial, and surgical histories, review of concurrent medications, physical examination, and selected clinical laboratory tests.8,15
To assess the severity of erectile dysfunction, the patient should be asked about the quality of sexual intercourse for the past 4 weeks to 6 months. A self-administered standardized questionnaire, such as the International Index of Erectile Dysfunction (IIEF), is often used. It is administered before initiation of any treatment and repeated at regular intervals during treatment. It includes 15 questions about the quality of sexual function and satisfactoriness of sexual intercourse.16 Questions include the following: How often were you able to maintain an erection? How difficult was it to sustain an erection? How satisfied are you with your sexual life? The physician should carefully assess the expectations for erectile function of the patient and the partner to ensure that expectations are reasonable. Shorter versions of the IIEF and other self-reporting questionnaires are also used in clinical practice. For example, the IIEF-EF comprises the six questions from the IIEF that focus on erectile function. The patient responds to each question, each response is scored on a range of 1 to 5. A score of 26 to 30 is considered normal function, 22 to 25 is mild erectile dysfunction, 17 to 21 is mild-to-moderate erectile dysfunction, 11 to 16 is moderate erectile dysfunction, and 10 or less is severe erectile dysfunction.
A medical history should be obtained to identify concurrent medical illnesses (e.g., hypertension, atherosclerosis, hyperlipidemia, diabetes mellitus, and depression) or surgical procedures (e.g., perineal or pelvic) that are risk factors for or are associated with organic or psychogenic erectile dysfunction. Underlying diseases that do not optimally respond to treatment should be addressed before specific treatment for erectile dysfunction is initiated. If the patient smokes cigarettes, drinks excessive amounts of ethanol, or uses recreational drugs, these social habits should be discontinued before specific treatment for erectile dysfunction is started.
CLINICAL PRESENTATION Erectile Dysfunction
A complete listing of the patient’s prescription and nonprescription medications and dietary supplements should be reviewed by the clinician, who should identify drugs that may be contributing to erectile dysfunction. If possible, causative agents should be discontinued or the dose should be reduced.
A physical examination of the patient should include a check for hypogonadism (i.e., signs of gynecomastia, small testicles, and decreased beard or body hair). The penis should be evaluated for diseases associated with abnormal penile curvature (e.g., Peyronie’s disease), which are associated with erectile dysfunction. Femoral and lower extremity pulses should be assessed to provide an indication of vascular supply to the genitals. Anal sphincter tone and other genital reflexes should be checked for the integrity of the nerve supply to the penis. A digital rectal examination in patients 50 years or older is needed to rule out benign prostatic hyperplasia, which may contribute to erectile dysfunction.
Selected laboratory tests should be obtained to identify the presence of underlying diseases that could cause erectile dysfunction. They include a fasting serum blood glucose and lipid profile. Serum testosterone levels should be checked in patients older than 50 years and in younger patients who complain of decreased libido and erectile dysfunction. At least two early morning serum testosterone levels on different days are needed to confirm the presence of hypogonadism.17
Finally, erectile dysfunction is a potential marker for arteriosclerosis. Therefore, older patients and those at intermediate and high risk for cardiovascular disease should undergo a cardiovascular risk assessment before starting on drug treatment for erectile dysfunction. By doing so, patients will be categorized into low-, intermediate-, or high-risk groups for cardiovascular morbidity related to sexual intercourse. Patients in the intermediate-risk group should undergo additional testing to reclassify them into the low- or high-risk group. The high-risk group should defer sexual activity. Patients in the low-risk group may start specific treatment for erectile dysfunction.8,18–20
TREATMENT
Erectile Dysfunction
Desired Outcomes
The goal of treatment is improvement in the quantity and quality of penile erections suitable for intercourse and considered satisfactory by the patient and his partner. Simple as this may sound, healthcare providers must ensure that patients and their partners have reasonable expectations for any therapies that are initiated. Furthermore, only patients with erectile dysfunction should be treated. Patients who have normal sexual function should not seek—or be encouraged to seek—treatment in an effort to enhance sexual function or enable increased activity. In addition, treatment should be well tolerated and be of reasonable cost.
General Approach to Treatment
![]() The Third Princeton Consensus Conference is a widely accepted multidisciplinary approach to managing erectile dysfunction that maps out a stepwise treatment plan.20–22 The first step in clinical management of erectile dysfunction is to identify and, if possible, reverse underlying causes. Risk factors for erectile dysfunction, including hypertension, coronary artery disease, dyslipidemia, diabetes mellitus, smoking, or chronic ethanol abuse, should be addressed and minimized. Patients should follow a heart-healthy lifestyle, which includes physical fitness, weight loss to achieve a normal body mass index, low cholesterol diets, no excessive ethanol intake, and no smoking.23 In some cases, these types of interventions are sufficient to restore erectile function.24 However, if erectile dysfunction does not respond to these measures, specific treatment is indicated.
The Third Princeton Consensus Conference is a widely accepted multidisciplinary approach to managing erectile dysfunction that maps out a stepwise treatment plan.20–22 The first step in clinical management of erectile dysfunction is to identify and, if possible, reverse underlying causes. Risk factors for erectile dysfunction, including hypertension, coronary artery disease, dyslipidemia, diabetes mellitus, smoking, or chronic ethanol abuse, should be addressed and minimized. Patients should follow a heart-healthy lifestyle, which includes physical fitness, weight loss to achieve a normal body mass index, low cholesterol diets, no excessive ethanol intake, and no smoking.23 In some cases, these types of interventions are sufficient to restore erectile function.24 However, if erectile dysfunction does not respond to these measures, specific treatment is indicated.
For patients with psychogenic erectile dysfunction, psychotherapy can be used as monotherapy or as an adjunct to specific treatments for the disorder. To enhance the relevance of psychotherapy, both the patient and the partner should be included in the counseling sessions. Treatment should be individualized and should address immediate factors that may be causing performance anxiety or depression. The effectiveness of psychotherapy is generally low, and long-term psychotherapy is often necessary.
![]()
![]()
![]() Specific treatments of erectile dysfunction include vacuum erection devices (VEDs), pharmacologic treatments, and surgery. The ideal treatment of this disorder should have a fast onset, be effective, be convenient to administer, be cost-effective, have a low incidence of serious adverse effects, and be free of serious drug interactions (Table 66-3). Generally, when choosing from among treatment approaches, those that are least invasive are selected first; more invasive therapies are reserved for patients who do not respond to first-line agents.
Specific treatments of erectile dysfunction include vacuum erection devices (VEDs), pharmacologic treatments, and surgery. The ideal treatment of this disorder should have a fast onset, be effective, be convenient to administer, be cost-effective, have a low incidence of serious adverse effects, and be free of serious drug interactions (Table 66-3). Generally, when choosing from among treatment approaches, those that are least invasive are selected first; more invasive therapies are reserved for patients who do not respond to first-line agents.
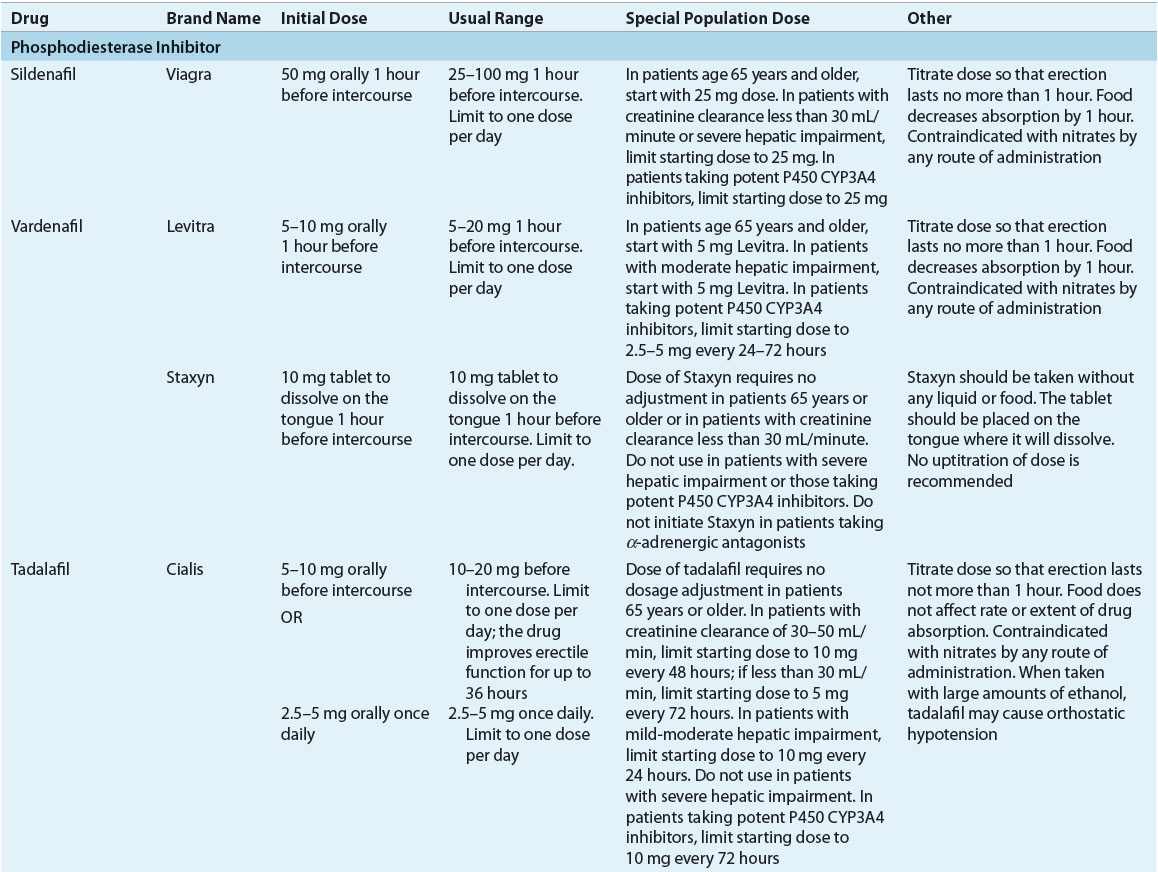
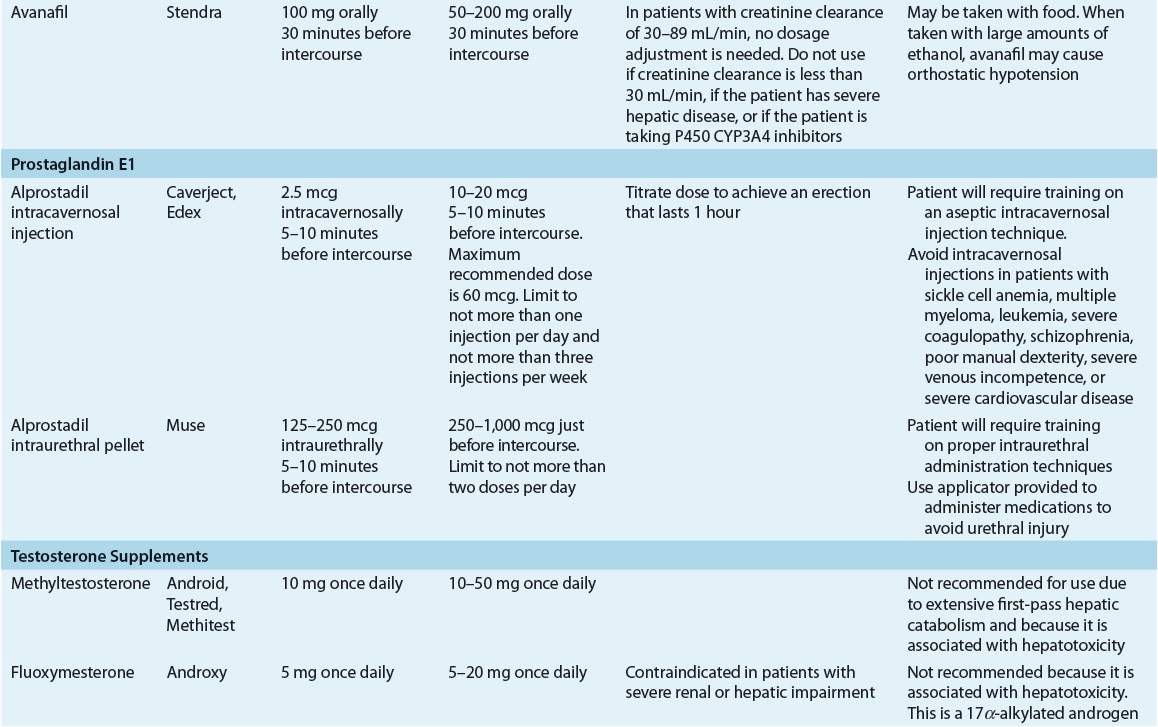
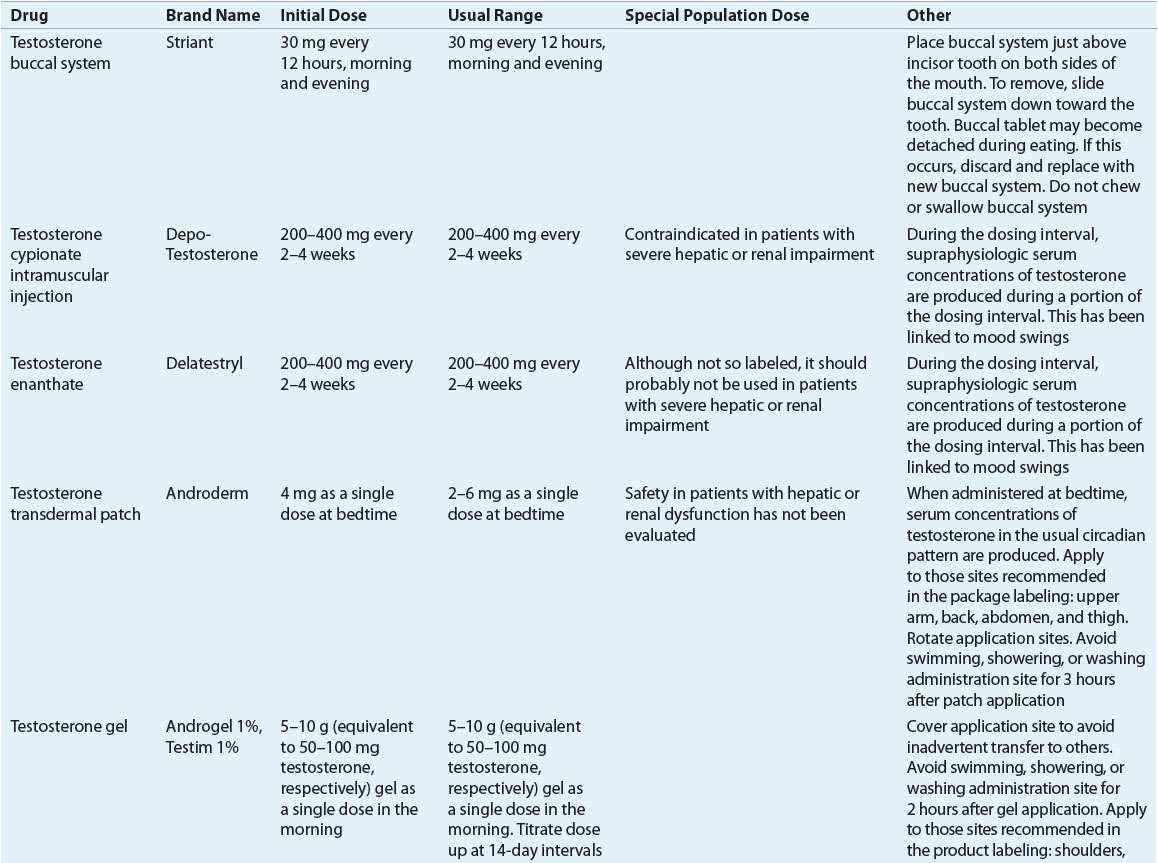
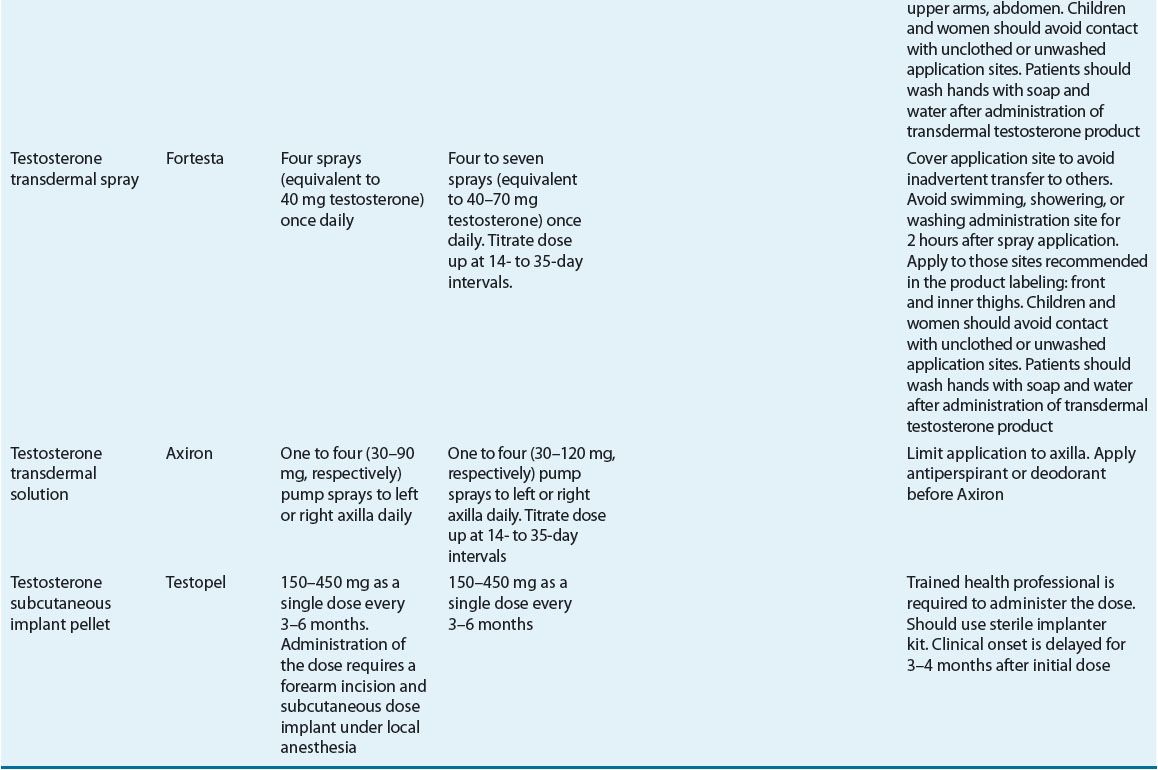
TABLE 66-3 Dosing Regimens for Selected Drug Treatments for Erectile Dysfunction
The American Urological Association Guideline on the Management of Erectile Dysfunction,15 the 2009 International Consultation of Sexual Medicine,25 and the American College of Physicians2 clearly identify oral phosphodiesterase inhibitors for first-line treatment. VEDs, intracavernosal injection of erectogenic agents, or intraurethral prostaglandin inserts are second-line treatments; prescribing of a particular agent for a patient should be individualized. Surgical intervention should be reserved for patients who fail to respond to first- and second-line treatments. A sample algorithm that guides selection of treatment is shown in Figure 66-2.
FIGURE 66-2 Algorithm for selecting treatment for erectile dysfunction.
Vacuum Erection Device
A VED has two parts: a pump, which generates a negative vacuum pressure; and a cylinder, which is closed at one end and into which the penis is inserted. The patient inserts his penis into the open end of the cylinder, which is then pushed up flush against his lower abdomen to create a vacuum chamber. Then the patient activates the pump to produce a vacuum pressure, which draws arteriolar blood into the corpora cavernosa. To prolong the erection, the patient can use constriction bands or tension rings, which are placed at the base of the penis, to keep the arteriolar blood in and reduce venous outflow from the penis. With the assistance of loading cones to protect the glans, these bands or rings can be rolled over the glans penis and up the erect penile shaft. Alternatively, they can be first threaded onto the plastic cylinder before the penis is inserted. Once the penis is erect, the band or ring can be rolled off the cylinder onto the base of the penis (Fig. 66-3). However, some patients prefer to apply the band or ring before the penis is erect.26,27
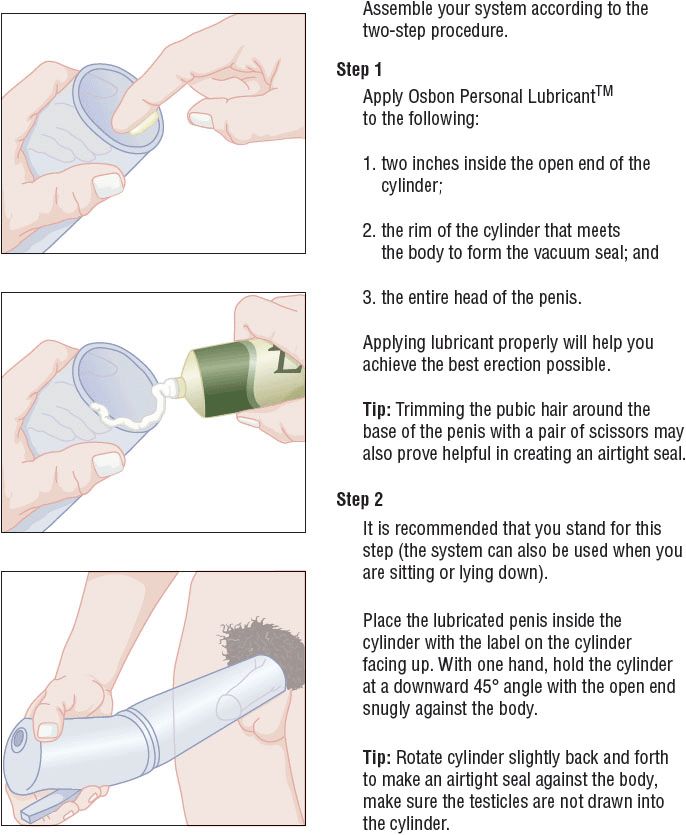
FIGURE 66-3 Technique for using a vacuum erection device. (From Osbon Erec Aid Esteem Vacuum Therapy System User Guide. Eden Prairie, MN: TIMM Medical Technologies, http://www.timmmedical.com/_l/pdf/timm-brochure-2012.pdf. Reprinted with permission.)
![]() The onset of action of the VED is 3 to 20 minutes. VEDs are not discreet. That is, a patient’s use of a VED is evident to the partner. For this reason, VEDs appear to work best in older patients who are married or who have stable sexual relationships. In this group, VEDs could be considered first-line therapy, and the overall satisfaction rate can be as high as 60% to 80% (range, 27–94%).26,27 VEDs may be used as second-line therapy in patients who do not respond to oral phosphodiesterase inhibitors, which includes patients who have had radical prostatectomy26 or those who do not respond to injectable drug treatments for erectile dysfunction. The combination of a VED with intracavernosal or intraurethral alprostadil26 or a phosphodiesterase inhibitor28 is associated with a higher efficacy rate than use of the VED alone. As a result, combination therapy sometimes is attempted before penile prosthesis surgery is considered in the patient who fails VED monotherapy.
The onset of action of the VED is 3 to 20 minutes. VEDs are not discreet. That is, a patient’s use of a VED is evident to the partner. For this reason, VEDs appear to work best in older patients who are married or who have stable sexual relationships. In this group, VEDs could be considered first-line therapy, and the overall satisfaction rate can be as high as 60% to 80% (range, 27–94%).26,27 VEDs may be used as second-line therapy in patients who do not respond to oral phosphodiesterase inhibitors, which includes patients who have had radical prostatectomy26 or those who do not respond to injectable drug treatments for erectile dysfunction. The combination of a VED with intracavernosal or intraurethral alprostadil26 or a phosphodiesterase inhibitor28 is associated with a higher efficacy rate than use of the VED alone. As a result, combination therapy sometimes is attempted before penile prosthesis surgery is considered in the patient who fails VED monotherapy.
Patients may discontinue using VEDs because they are inconvenient and or not discreet. It has been reported that 20% to 50% and 50% to 64% of initial users continue with VEDs after 1 year and 5 years, respectively.26,29 Also, 6% to 11% of partners complain that the penis is cool to the touch or is discolored (bluish) in appearance, particularly when constriction bands are used.
VEDs are available with battery-operated pumps, which offer convenience, particularly in patients with arthritis of the hands. The American Urological Association recommends the use of commercially available VEDs by prescription only. These have safety mechanisms that minimize the likelihood of excessively high vacuum pressures which can cause penile discomfort and injury.15
Pain or injury from VEDs most often is caused by the constriction bands used to sustain an erection. Because these rings trap blood in the corpora and reduce arteriolar flow into the penis, the penile shaft may feel cold and numb. If the constriction bands are applied for longer than 30 minutes, the penile shaft may turn blue and hurt. Patients may complain that a hinge-like erection is produced in that the penis pivots on the rubber ring or tension band. Patients sometimes fail to ejaculate.
VEDs are contraindicated in patients with sickle cell disease. These patients are prone to priapism, which can be exacerbated by the use of constriction bands with VEDs. The devices also should be used cautiously by patients taking oral anticoagulants because warfarin, through a poorly understood and idiosyncratic mechanism, can cause priapism.
Phosphodiesterase Inhibitors
Mechanism
In the presence of sexual stimulation, nitric oxide is released by neurons and endothelial cells in cavernosal tissue, thereby enhancing the activity of guanylate cyclase, the enzyme responsible for conversion of guanylate triphosphate to cGMP (Fig. 66-4).30 cGMP is a vasodilatory secondary messenger that upregulates the response to nitric oxide by activating protein kinase G. This decreases intracellular calcium levels, resulting in smooth muscle relaxation, enhanced arterial flow to the corpora cavernosa, and enhanced blood filling of cavernosal sinuses.30 Catabolism of cGMP in cavernosal tissue is mediated by phosphodiesterase isoenzyme type 5.
FIGURE 66-4 Mechanism of action of phosphodiesterase inhibitors. All inhibit catabolism of cGMP, a vasodilatory secondary messenger. (cGMP, cyclic guanosine monophosphate; NANC, nonadrenergic noncholinergic.)
Four competitive, reversible inhibitors of the phosphodiesterase isoenzyme type 5 found in genital tissue are marketed for erectile dysfunction in the United States (Table 66-4). Chemically, they are nonhydrolyzable analogs of cGMP and they act by decreasing catabolism of cGMP. However, phosphodiesterase isoenzyme type 5 is also found in peripheral vascular tissue, tracheal smooth muscle, and platelets. Inhibition of phosphodiesterase in these nongenital tissues can produce unwanted effects.30
TABLE 66-4 Pharmacodynamics and Pharmacokinetics of Phosphodiesterase Inhibitors
The four marketed phosphodiesterase inhibitors differ in their degree of selectivity in inhibiting phosphodiesterase isoenzyme type 5 and other phosphodiesterase isoenzymes, pharmacokinetic profiles, drug–food interactions, and adverse effects (see Table 66-4).
Efficacy
Because of their apparent effectiveness, convenient route of administration, and comparatively low incidence of serious adverse effects, phosphodiesterase inhibitors are considered first-line therapy for erectile dysfunction, particularly in younger patients. They allow for discreet use. Although not based on direct comparison trials, all four commercially available phosphodiesterase inhibitors are considered to be equally effective.31,32 Patient preference studies show that some patients may prefer one agent over another based on the preferences of the patient or partner; or the onset, duration, or cost of treatment.33 Usual starting and maintenance dose regimens are included in Table 66-3.
In the presence of sexual stimulation and in doses of 25 to 100 mg, sildenafil produces satisfactory erections in 56% to 82% of patients, independent of the etiology of erectile dysfunction. Similar results are documented in the product labeling for the other agents in this class (65–80% for vardenafil, 62–77% for tadalafil, and 50–55% for avanafil). Response rates in the lower range for phosphodiesterase inhibitors have been documented in patients with diabetes mellitus or after radical prostatectomy, or those with severe vascular disease, probably due to neuropathy or surgery-related nerve damage, respectively, in which nitric oxide availability is compromised.6,15,34 The effectiveness of the drugs appears to be dose related.
![]() Approximately 30% to 40% of patients do not respond to phosphodiesterase inhibitors.15 At least half of nonresponders can benefit from education on proper use of the drugs.34,35 Therefore, follow-up is always recommended after a phosphodiesterase inhibitor is initiated. Education of patients should include the following points: (a) patients must engage in sexual stimulation (foreplay) for the best response; (b) sildenafil and vardenafil should be taken on an empty stomach, at least 2 hours before meals, for the fastest response, but tadalafil and avanafil can be taken without regard to meals; (c) patients who do not respond to the first dose should continue with the phosphodiesterase inhibitor for at least five to eight doses before failure is declared, as increasing success rates are reported with sequential dose administration; (d) some patients require dosage titration up to 100 mg sildenafil, 20 mg vardenafil, 20 mg tadalafil, or 200 mg avanafil for a response; (e) patients should avoid excessive alcohol intake, which can cause drowsiness and hypotension and worsen erectile dysfunction; (f) involvement of the sexual partner can help improve the patient’s response to treatment; and (g) treatment of concomitant medical illnesses which contribute to erectile dysfunction (e.g., diabetes mellitus, hypertension, and hypogonadism) should be optimized. If the patient has depression because of divorce or loss of a sexual partner, or has performance anxiety, psychologic counseling may be helpful.21
Approximately 30% to 40% of patients do not respond to phosphodiesterase inhibitors.15 At least half of nonresponders can benefit from education on proper use of the drugs.34,35 Therefore, follow-up is always recommended after a phosphodiesterase inhibitor is initiated. Education of patients should include the following points: (a) patients must engage in sexual stimulation (foreplay) for the best response; (b) sildenafil and vardenafil should be taken on an empty stomach, at least 2 hours before meals, for the fastest response, but tadalafil and avanafil can be taken without regard to meals; (c) patients who do not respond to the first dose should continue with the phosphodiesterase inhibitor for at least five to eight doses before failure is declared, as increasing success rates are reported with sequential dose administration; (d) some patients require dosage titration up to 100 mg sildenafil, 20 mg vardenafil, 20 mg tadalafil, or 200 mg avanafil for a response; (e) patients should avoid excessive alcohol intake, which can cause drowsiness and hypotension and worsen erectile dysfunction; (f) involvement of the sexual partner can help improve the patient’s response to treatment; and (g) treatment of concomitant medical illnesses which contribute to erectile dysfunction (e.g., diabetes mellitus, hypertension, and hypogonadism) should be optimized. If the patient has depression because of divorce or loss of a sexual partner, or has performance anxiety, psychologic counseling may be helpful.21
The phosphodiesterase inhibitors should not be used by patients with normal erectile function. Also, according to FDA-approved labeling, the drugs should not be used in combination with other forms of therapy for erectile dysfunction because prolonged erections (which may lead to priapism) may result.15,36 Also, phosphodiesterase inhibitors should be avoided in patients predisposed to developing priapism, including men with sickle cell anemia, leukemia, or multiple myeloma.
Long-term use of phosphodiesterase inhibitors for five to six consecutive years continues to be effective and is not associated with tachyphylaxis. The voluntary discontinuation rate among patients who respond to phosphodiesterase inhibitors is less than 2% per year.36–38
Clinical Controversy…
Despite the initial effectiveness of phosphodiesterase inhibitors and the measures to salvage patients with re-education, some patients will show minimal or no response to maximum doses of a phosphodiesterase inhibitor. Various strategies have been attempted in this subgroup of patients, including the following:
1. The effectiveness of switching from one phosphodiesterase inhibitor to another when the patient does not respond to an initial agent is controversial. In one study, vardenafil was beneficial in patients who did not respond to sildenafil.39 However, less than 5% of patients who fail to respond to a phosphodiesterase inhibitor experience benefit from switching to another phosphodiesterase inhibitor.34 Controlled clinical trials in larger patient groups are needed before this strategy is used as routine treatment.
2. High-dose phosphodiesterase inhibitor treatment (e.g., sildenafil 200 mg) has been used anecdotally. However, such doses are also associated with a higher frequency of adverse effects.40
3. In patients with primary hypogonadism and erectile dysfunction, correcting the former with testosterone supplementation improves the response to a phosphodiesterase inhibitor.41
4. Phosphodiesterase inhibitors have been combined with intracavernosal or intraurethral alprostadil in selected patients.42,43



