INTRODUCTION
External factors, forces, and agents play a significant role in the causation of human disease. The environment in which we live is hardly benign and we are constantly exposed to its potential hazards. These include physical, chemical, thermal, and electrical forces as well as ionizing radiation. Noncommensal microbiological organisms are also external agents. While within the spectrum of human disease there are conditions where external factors have little or no role, such as some inherited disorders of metabolism or the muscular dystrophies, in most human afflictions external factors interact with host factors to produce disease. Certain lung cancers are linked to cigarette smoking and liver disease is a well-documented consequence of heavy alcohol consumption, yet in spite of the clear evidence that links these two agents to these diseases, it is also the case that only a minority of smokers and drinkers respectively develop them. At the other end of the spectrum lie the instances where external forces or agents are essentially the only factors as in trauma from a natural catastrophe like an earthquake or a -man-made event such as a motor vehicle crash.
The environmental hazards any one individual is exposed to are determined by a variety of factors including geography, socioeconomic status, and culture. This is true not only for infectious entities such as malaria which depends on an insect vector that itself requires certain climatic conditions for its existence but also for various forms of trauma. Cobra bites are a common problem in India but not in the United States. Motor vehicle-related injuries, gunshot wounds, cutting injuries, and disorders related to contaminated air and water vary from country to country and regionally within countries just as do the incidence of infectious and other diseases.
This chapter will deal with diseases or conditions that are primarily the result of external factors but will not discuss diseases caused by microorganisms except to mention that infections, often from normal flora, are a common complication of trauma and remind readers that many vectors that spread infection require the physical trauma of a bite to inoculate the host. Tetanus caused by a toxin produced by the bacillus, Clostridium tetani, usually occurs after the introduction of that soil-dwelling organism into tissues as a consequence of a wound and similarly gas gangrene from Clostridium perfringens and other species. In the days before vaccination for tetanus, antiseptic surgery, and antibiotics, these entities were a common often-fatal complication of agricultural, martial, and other trauma and in some areas of the World today remain so.
INJURY
A measure of the burden of injury to the healthcare system in the United States is the fact that one-third of all emergency department (ED) visits in 2008, some 42.8 million, were injury related (Table 3-1). Injury is the leading cause of death for people ages 1–44 years in the United States, and because these deaths are in younger individuals, the years of potential life lost is greater than many conditions that account for a greater number of deaths (Table 3-2).
| Cause of Death | YPPL | Total Percentage (%) |
|---|---|---|
| All causes | 20,486,000 | 100 |
| Malignancies | 4,327,000 | 21.1 |
| Unintentional injury | 3,272,000 | 16.0 |
| Heart disease | 3,054,000 | 14.9 |
| Perinatal disease | 1,093,000 | 5.3 |
| Suicide | 1,009,000 | 4.9 |
| Homicide | 783,000 | 3.8 |
| Congenital abnormalities | 588,000 | 2.9 |
| All others | 6,359,000 | 31.0 |
Acute injuries have immediate consequences for the victim with the potential for subsequent and long-term complications. Recurring trauma, even that which has little apparent immediate consequence, can also lead to disorders. A single episode of heavy ethanol intake may lead to acute intoxication with little or no subsequent complications, while repeated episodes can result in cardiomyopathy and/or cirrhosis of the liver, two of the many potential consequences of chronic alcohol abuse. If the acute ingestion is large enough, however, it may lead to fatal respiratory depression. Moreover, in an inebriated state an individual is at greater risk of additional injury whether by falling, attempting to drive a motor vehicle, leaving a pot on the stove and starting a fire, or becoming involved in an activity that they would not have undertaken in a sober state.
A driver injured in a motor vehicle crash sustains some degree of immediate impairment, depending on the severity of the crash. The period required for recovery will also vary accordingly. During that period they are at risk of a variety of complications including infection and deep vein thrombosis with pulmonary embolism. In many instances of trauma, recovery is incomplete and the affected individual will thereafter function at a lower level than before the incident, thereby suffering a diminished quality of life. If there is sufficient impairment, such as paralysis or severe brain damage, susceptibility to pressure sores, infection, and other long-term complications may lead to a significantly reduced life span.
Repeated injuries due to chemicals or toxins can lead to disease as is the case for smoking and ethanol. This may also occur after physical and other modes of trauma. Examples include repetitive motion disorders such as carpal tunnel syndrome, osteoarthritis in the limbs of athletes, professional or otherwise, and traumatic encephalopathy. This latter condition, dementia pugilistica, was first noted in boxers following repeated blows to the head, and is now being recognized in football players and other participants in activities where concussions are common. External factors that can lead to injury can be separated into five major categories: physical, chemical, thermal, electrical, and ionizing radiation.
Physical injuries are those that are related to mechanical interactions and are the most common types of acute injuries from external forces seen in medicine. Motor vehicle wrecks, gunshot wounds, stabbing and cutting injuries, falls, and various mechanical asphyxias fall into this category. We include in this category the effects of pressure and altitude.
Chemical injury includes exposure to noxious or asphyxiant gases, medications both legal and illegal, and other chemical, metals, and mineral agents.
Thermal injury results from the exposure to fire and other sources of heat as well as intensely cold surfaces. Environmental exposure to heat or cold may also lead to local injury and/or systemic dysfunction.
Electrical forces include the natural phenomenon of lightning as well as exposure to man-made electrical currents.
Ionizing radiation employed as a therapeutic and diagnostic modality in medicine can also lead to unintended injury. Such radiation is also present naturally in our environment and the specter of the consequences of the detonation of a nuclear bomb or a mishap at a nuclear power plant currently “haunt” our society. Solar radiation can potentially lead to both acute and chronic health problems.
QUICK REVIEW
The same paradigm with which physicians approach the diagnosis of “natural” illnesses is utilized as a first principle in the consideration of injuries from external factors. History, signs and symptoms, supplemented by laboratory tests and imaging studies are used to identify the basic pathological process, the underlying disease, which explains them. Similarly, in the case of trauma, one accepts that injuries caused by a particular injury mechanism will be similar in appearance and character. That is, a sharp object, a bullet or a blow from a blunt instrument will produce distinctive injuries that can be recognized as to their source. Likewise, electrical and thermal forces cause distinctive and recognizable injuries. Drugs or toxins may also produce characteristic signs and symptoms that can be utilized to identify a specific agent. In evaluating physical injuries, this is often referred to as recognizing patterned injury. The appearance of an injury reflects the nature of the object and force that caused it and allows the informed observer to infer the cause of an individual injury from its appearance.
A second principle is that particular situations in which injuries occur produce groupings or larger patterns of injury. Thus, the driver of a motor vehicle that collides head-on with an immoveable object will be thrown forward as the vehicle decelerates. If unrestrained, their chest will strike the steering wheel and their head the windshield. This may produce visible external injuries to the head and chest as well as typical internal organ damage. Awareness of the nature of the injury incident in such a case is important to the evaluating physician when the victim arrives at ED as it helps inform what diagnostic and therapeutic steps may need to be taken. Failure to appreciate the underlying causes of injuries may have consequences beyond a failure to adequately provide immediate medical care. If it is not recognized that the injuries a patient presents with are inconsistent with the explanation provided by the patient or their caretaker(s), that patient may be returned to a environment where they are at risk of further injury or even death. This is particularly the case for injuries inflicted in abusive relationships. Infants are unable to speak for themselves, and older children, spouses, partners, and the elderly may be unwilling to reveal the true source of their trauma because of fear or shame. Similarly the failure to recognize that a toxin exposure may have an environmental cause, or that the patients symptoms are due to a toxin, may result in the patient being sent back to be further exposed.
It then follows that in the evaluation of injury from external forces not only must the immediate cause of the injury be identified but also an understanding of how the victim encountered the injurious force must be sought.
It is customary to separate traumatic injuries into three categories based on the circumstances in which they are incurred: unintentional (accidental), self-inflicted, and assaultive, (deliberately caused by another human). The latter two are referred to as “intentional” injuries and assaultive is sometimes also referred to as “violent.” When applied to fatal injuries, this leads to the classification of trauma-related deaths as accident, suicide, or homicide. These designations are referred to as “manners” of death. An unintentional (accidental) injury is one that is not the consequence of a deliberate human action intended to cause harm, but it is important to appreciate that many injuries deemed unintentional are in fact the consequence of actions intentionally undertaken by the injured or another party, actions that may clearly have put the injured party at significant risk. In fact, the line that delineates intentional from unintentional when the risk of self or other injury is high and clearly apparent to the neutral observer can be difficult to draw and presents a recurring dilemma in medicolegal death investigation and certification as well as in the courts regarding legal culpability. For instance, when a chronic drug abuser dies of an overdose is it the consequence of a miscalculation, carelessness, desire for a better “high,” or a calculated intent to end it all? Some “recreational” activities are more dangerous than others, for example, mountain climbing versus vegetable gardening. At what point does the likelihood of injury inherent in a voluntary activity dictate that a resulting injury and death is suicide rather than accident? Most accident insurance policies have exclusions for activities the insurance company considers too dangerous to cover even though a death occurring during that activity would be certified as accidental by a medicolegal authority. Designating an injury or death as “accidental” does not mean either that there can be no criminal or civil culpability on the part of another human agency. Similarly, classifying a death as a homicide does not necessarily mean that someone is criminally liable. Crimes and civil liability are defined by law and manner of death classification is intended primarily for epidemiological purposes as is the similar designation of nonfatal injuries as unintentional, intentional, self-intent, and assault. Strategies to reduce the number of head injuries due to falls are quite different from those due to assaults.
WHAT WE DO Medicolegal Death Investigation
Forensic pathologists play a major role in the area of medicolegal death investigation. This historically derives from pathologists’ involvement with morbid anatomy and autopsies. In fact many of the first autopsies noted in the literature were performed for medicolegal reasons. While the heyday of the autopsy as a tool in our understanding of basic disease processes may have passed, the autopsy still remains an essential diagnostic procedure in determining cause of death and gathering needed information in deaths that occur suddenly and unexpectedly or as a result of trauma. These deaths in most of the world require medicolegal investigation and certification. This is the subspecialty of forensic pathology. In medicolegal death investigation, a medicolegal authority (MLA) assumes jurisdiction and control over certain decedents in order to ascertain why they died. The forensic pathologist may be the MLA, which in the United States is usually a Medical Examiner or Coroner, or may be employed by the MLA. Medical Examiners are appointed officials and ordinarily physicians, although not always forensic pathologists. Coroners are for the most part elected lay officials, though in a few states they must be physicians in order to run for the office. There is no uniformity in the organization of medicolegal death investigation systems within the United States, which are state and/or county based. There is even some variation in which deaths must be reported among the states. With a few exceptions, however, it is the case that all deaths related to acute trauma must be reported to the MLA and the MLA is responsible for certifying them. Deaths due entirely to natural disease are ordinarily certified by the decedent’s attending physician.
Medicolegal death investigation systems have an important surveillance function since unexpected and unexplained deaths also come under their jurisdiction. They have played a role in the identification of a number of emerging infectious entities over the years including AIDS, Hantavirus, and Legionnaires disease. Data amassed by Medical Examiner and Coroner’s offices are critical in monitoring deaths due to trauma, drugs, and medications. This data provides the epidemiological information necessary to both identify areas where interventions are possible and the basis for determining whether such interventions once implemented have been successful.
As mentioned previously, patients may exhibit signs and symptoms from underlying natural disorders as well as injuries, the consequence of an untoward interaction with the environment. Traumatic injuries may lead to disorders that are not considered external, like pulmonary emboli or infection. It is important, however, to recognize a connection when it is there since to ignore it is akin to treating symptoms of disease without addressing the underlying cause. Pathogenic sequences connect causes and effects. In such sequences, each entity listed is the consequence of the one preceding it. A myocardial infarct results from myocardial ischemia due to diminished or interrupted coronary blood flow that is the consequence of coronary restriction from atherosclerosis. The underlying or proximate condition leading to the infarct is then atherosclerosis. An individual might develop sepsis due to peritonitis that was caused by a bowel injury incurred in a motor vehicle wreck. The wreck is then the underlying or proximate cause of the sepsis. This is particularly important in the process of death certification where the certifier must decide what the underlying disease condition leading to death was. Many deaths are inaccurately certified in regard to their cause when the certifier assigns it to the last process, the one immediately preceding death, and fails to include the underlying cause of that condition. In the case of the last example, attributing death to sepsis due to peritonitis without including the trauma would result in the death being classified as natural rather than unnatural. Failing to link pulmonary fibrosis to asbestos exposure or liver failure to acetaminophen toxicity conceals the contributions of those external factors to human disease.
FACTORS INFLUENCING PHYSICAL INJURY
Physical injury may occur when a moving individual strikes a solid object or surface or a stationary individual is impacted or compressed by a moving object or force. In such interactions, there are several factors that determine the likelihood that significant injury will result.
All moving objects or bodies have kinetic energy and as the amount of energy in an interaction increases so does the likelihood of injury. Kinetic energy is the product of the mass of an object times the square of the velocity divided by two. As the mass (weight) increases, there is a direct proportional increase in the amount of energy, while as the velocity increases the energy goes up by the square of the velocity increase. For example, if a baseball and a car were both traveling 30 miles per hour, one could safely catch the baseball, but certainly not the car because the baseball weighs less than half a pound while the car weighs 3000 lb. Similarly a jump from a 3 foot platform to the ground would seldom lead to injury, but the same person jumping from a 32 foot platform would be likely to suffer serious perhaps even fatal injury. The additional velocity imparted by the acceleration of gravity over the 29 foot difference imparts to the moving body sufficient kinetic energy to distort and disrupt internal structures when the individual impacts the ground.
Area over which force is applied: The likelihood of injury is also related to the area over which the particular force is applied. Concentration of the energy of impact over a small area can overcome the resistance of the tissues to deformation and penetration. This can allow entry of an object into the body leading to damage to deeper internal organs. Even in the absence of penetration, there may be sufficient local deformation to cause mechanical disruption of underlying organs and tissues. Bullets, knives, arrows, and other sharp objects have the potential to cause serious injury because they can overcome the resistance of the skin and often underlying bone to reach vital organs and structures, even though the quantities of kinetic energy involved are not large. Similarly a blow from a bat, pipe, or club concentrates the area over which the energy of the impact is dissipated, resulting in more local and/or even deeper injury than would have occurred if the impacting surface was broader. The same applies in reverse when a moving body impacts a stationary surface, for example, stepping on a nail or falling and striking the projecting edge of a piece of furniture.
Time interval during which force is applied: Another factor is the time interval over which the interaction occurs. If it can be lengthened, the likelihood of injury can be lessened. The padding of helmets and dashboards in part does this. It is the principal that allows “bungee” jumping and the different consequences that follow diving into a swimming pool full of water versus one that is empty. In both instances, the energy generated by the fall is safely absorbed and dissipated over distance and time by the elastic cords in the first instance and the yielding water in the second.
Tissue resistance to force: The body’s tissues also vary in their resistance to trauma with bone being more resistant that skin. Internal connective tissues are more resistant than muscle that is more resistant than internal organs such as liver and spleen.
Body area(s) affected by force: The significance of any injury to the overall health of an organism is related to the parts affected in addition to the extent of tissue disruption. Injuries that compromise the vital functions of respiration and circulation have the greatest potential to be immediately life threatening, whereas injuries to the extremities or noncritical organs are more potentially survivable, particularly with timely appropriate medical treatment. Many of these factors are not only exploited in the design of weaponry but are also utilized in devising protective strategies. Seat belts, cushioned dashboards, air bags, protective armor, and bicycle helmets all attempt to decrease the likelihood of injury to internal organs in forceful interactions by dissipating the forces of collisions over a larger area extending the interval over which they are dissipated as well as shifting them to tissues of greater resistance.
Fitness of individual: A last factor to be considered is the fitness of the individual injured. Significant preexisting medical conditions as well as the extremes of age may render one individual less likely to survive a given degree of insult than a fitter individual. Older persons are often more fragile and have a diminished capacity for tissue repair. Survival from severe burns, for instance, is inversely proportional not only to the extent and severity of the burns but also to the age of the victim. Injuries of an extent that would easily be survived by younger individuals often prove fatal to the elderly, and a fall leading to a broken hip, rapid decompensation, and death is a common occurrence. Infants and small children have the optimal capacity for repair but are relatively more fragile—an impact that might only bruise an adult can prove fatal to an infant.
HISTOPATHOLOGY OF PHYSICAL TRAUMA
The histopathology of physical trauma is that of inflammation and wound repair and is virtually never employed in the evaluation of nonfatal injuries. In the investigation of fatalities, however, microscopy can aid in the determination of the age of bruises, lacerations, and hemorrhages. (Case 3-1) It may also be helpful in confirming the presence of powder residues in close range or contact gunshot wounds.
CASE 3-1
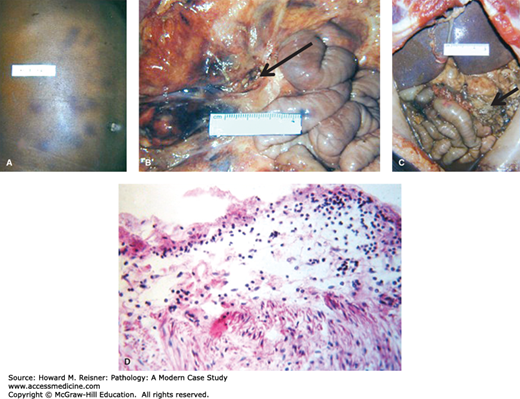
A 2-year-old boy is brought to an emergency room (ER) with a complaint of abdominal pain, having collapsed while being bathed at home by a relative. He experiences respiratory arrest, cannot be resuscitated and is pronounced dead at the ER. Autopsy reveals multiple cutaneous bruises including some on the abdomen (Figure 3-1A). Internal examination reveals a mesenteric tear (Figure 3-1B arrow), a laceration of the small bowel and active peritonitis (Figure 3-1C arrow).
Death was deemed due to peritonitis consequent to a blow or blows to the abdomen that ruptured the bowel. Suspicion initially focused on the relative but the degree of inflammation at the site of the rupture (Figure 3-1D) indicated that the fatal injury must have occurred at least a day prior to death implicating a different caregiver.
MECHANISMS OF PHYSICAL TRAUMA
Interactions that lead to injury may be characterized as blunt, sharp, or penetrating, although there is overlapping between these categories. Blunt trauma can result from falls and blows from objects with blunt (as opposed to sharp) surfaces as well as collisions with blunt objects or surfaces. The majority of physical injuries encountered in most medical practices will fall into this category. Blunt force interactions can produce the following.
Bruises (contusions): These result from the mechanical disruption of blood vessels. Blood escapes into the surrounding tissues leading to swelling and discoloration. Although cutaneous bruises are the most visible they can also occur within internal organs and tissues. Cutaneous bruises can be visually aged, although not precisely. Fresh bruises are reddish-purple and change color as the body “repairs” the injury and clears the hemorrhage. The only consistent pattern is a change to yellow initially at the periphery of the bruise, eventually fading to brown. This alteration first appears at 1–3 days postinjury. Bruises generally are resorbed within 3–4 weeks with bruises in more vascular areas disappearing more rapidly. In instances where histological examination of the bruise is possible, greater accuracy can sometimes be obtained but there is still considerable variability.
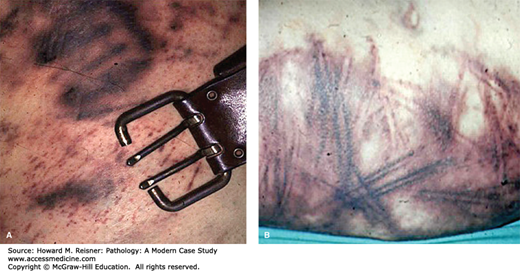
The shape of a bruise reflects the shape and nature of the object that struck the body or the surface that the body struck. This is important for both forensic and clinical reasons. Recognizing that the looped bruises noted on a child’s back during an hospital ER visit were the result of its being “disciplined” with a cord or belt rather than by playing with the family dog per the history given by the caretaker could lead to a potentially lifesaving intervention (Figure 3-2).
FIGURE 3-2
(A) Bruises may take the shape of the object that caused them—in this case a belt buckle. (B) “Tramline” bruises showing a distinctive parallel pattern result from skin impact with elongated rounded objects that force blood to the margins of the impact. This example shows curving of the bruises produced by a flexible object; an electrical cord.
Abrasions (scrapes, “burns”): These are the consequence of interactions that are tangential to the injured surface and result in damage or loss of the superficial and often deeper layers of skin. Such injuries are common in sports and the ordinary play of children and adults. They can be particularly extensive when high-speed interactions are involved such as a fall from a moving vehicle, such as a motorcycle (Figure 3-3).
Lacerations (tears): These occur when the integrity of the skin or other tissue is disrupted due to crushing or torsional forces. They are more common over bony prominences where skin can be compressed between an impinging object or surface and underlying bone. An identical blow to the head that leads to a scalp laceration may only produce a bruise in a part of the body without underlying bone such as the abdomen. A laceration is characterized by irregular, often bruised, and abraded margins. The tissues at the margins may be devitalized to the extent that clinically debridement may be required before the edges can be reapproximated. The term laceration should only be used for injuries of this nature and not for those caused by sharp objects. Like bruises the size and shape of a laceration provide information about the nature of the object or surface that produced it (Figure 3-4).
Avulsions: These are shearing injuries caused by tangential forces. In an avulsion, the skin or tissues are substantially separated from the deeper underlying structures. A common example would be the separation of a fingernail from its bed by catching it on a protruding object. So-called “scalping” injuries where the skin of the scalp is torn and separated from the underlying skull would be another example.
Fractures: Bone may be disrupted by compression, twisting, or bending. Such fractures are described as “incomplete” when the broken parts are not separated, “complete” when they are, “comminuted” when complete and the fracture results in more than two fragments. When the overlying skin is lacerated by broken bone, it is designated as “compound.” “Pathologic” fractures are those that occur at sites where bone has been weakened by natural diseases such as tumor or osteoporosis. Such fractures can be the consequence of ordinary weight bearing. There are many specific clinical designations for the fractures of various bones, often eponymic, in part, reflecting the frequency with which such injuries are consistently seen in the clinical setting; for example, Le Fort I, II, and III fractures describe trauma to the maxillae and adjacent bones, resulting from blows or other facial impacts. This reflects the earlier touched upon principle that particular injury situations often result in predictable patterns of injury.
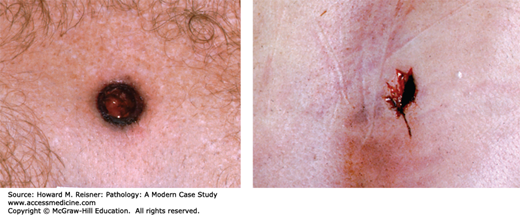
Incised wounds (cuts): These are injuries produced by objects with sharp or cutting edges such as knives, scalpels, or broken glass. They should not be described as “lacerations!” Such injuries are characterized by distinct linear margins without bruises or abrasions. The tissues are cleanly separated down into the depths of the wound (Figure 3-6). Most “stab” wounds are caused by sharp implements and are discussed further below.
FIGURE 3-6
Two examples of incised wounds. (Left) Incised wound of the wrist with suicidal intent. Note presence of tentative or hesitation cuts crossing the wound often characteristic of suicidal injuries. (Right) Homicidal incised wounds that demonstrate “clean” margins and characteristic gaping in the direction of tissue tension.
Chop injury: Instruments with sharp edges that are also very heavy produce injuries with both sharp and blunt force characteristics when they are used as weapons. These include axes, machetes, cleavers, brush hooks, and swords. The resulting skin wounds often have straight clean margins, since these weapons have sharp edges. When firm underlying tissue or bone is struck, it may be cleaved to an extent that would not have been possible with a lighter cutting implement. Impacted bone may show a straight-edged defect identical to the chop mark that results when an axe strikes a piece of wood. The rest of the bone underlying the impact site may also break, resulting in a complete fracture.
Penetrating injury: These injuries can be caused by both blunt and pointed objects and those with sharp edges as well as projectiles and are characterized by the fact that they have passed through the skin and extended deeper into the body. The extent of internal trauma cannot always be appreciated by the external appearance of a wound (Case 3-2). If a wound passes completely through the body, it is described as “perforating.” These terms may also be used to describe an injury to an individual organ or body structure.
CASE 3-2
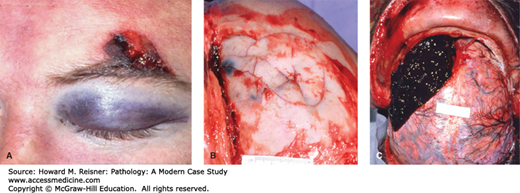
A 27-year-old man got into an argument at a bar and was struck in the head with a pool cue. He was not rendered unconscious, left the premises under his own power and was seen to get into his vehicle and drive away. A few hours later his truck was noted parked on the shoulder of a nearby road. The key was turned off in the ignition and he was in the driver’s seat slumped over deceased. External examination revealed a small laceration of the left supraorbital area and a periorbital ecchymosis (Figure 3-5A).
Internal examination demonstrated a partly depressed comminuted fracture of the underlying frontal bone (Figure 3-5B). The fracture line passed through the vascular groove on the inner table of the skull carrying the middle meningeal artery disrupting that vessel causing a large epidural hemorrhage (EDH). This expanding mass had led to left-sided transtentorial brain herniation and his death (Figure 3-5C).
Intracerebral hemorrhage is a common consequence of head trauma and can occur in the epidural, subdural, and/or subarachnoid compartments (EDH, subdural hemorrhage [SDH], and subarachnoid hemorrhage [SAH], respectively). EDH is almost always associated with a skull fracture that tears an imbedded or adherent arterial vessel. Because of the middle meningeal artery’s course within a vascular groove in the relatively thin squamous portion of the temporal bone, it is particularly vulnerable. SDHs are usually seen over the cerebral convexities and are felt to be resulted from the tearing of veins bridging the subdural space along the falx. SAH results from disruption of meningeal or other vessels on the surface or base of the brain as may happen with the ruptue of congenital lesions, “berry” aneurysms, of the circle of Willis (see Chapter 21). SAH can also accompany cerebral contusions or from blood dissecting to the surface from deeper intracerebral bleeding.
EDH and SDH become intracranial space occupying lesions and may lead to brain stem herniation. The mechanism whereby “pure” acute SAH causes death is not entirely clear but may involve vascular spasm. In instances of EDH, SDH, and SAH, there may also be accompanying traumatic cerebral parenchymal injury that may be of greater significance than the extracerebral blood. The rapidity with which the bleeding occurs is an important factor. Slow accumulations of blood, particularly in SDHs, are often well tolerated with little or no symptoms, becoming chronic and in some instances eventually being largely organized and resorbed while a similar volume of blood accumulating more rapidly would lead to herniation and death.
Stab wounds: Such wounds are usually sharp force injuries caused by knives or knife-like objects but can also result from the thrust into or the impaling of the body onto other pointed objects, for example, screwdriver or ice pick. The depth of the wound cannot be judged by the appearance of the wound in the skin and what appears to be a small cut in the skin may in fact be a potentially lethal wound to deeper internal organs. Since a blade cuts as it passes through the skin, the defect in the skin can be longer than the width of the blade itself, and because the body and tissues are compressible, the depth of the wound may be greater than the length of the stabbing instrument. The depth may also be less since the instrument may not be fully inserted.
Gunshot wounds: These are penetrating injuries produced by rapidly traveling projectiles of small size. It is the high speed of these objects and the small area over which their resultant kinetic energy is applied that causes injury, not their mass (weight). In most firearms, the projectile whether bullet or shot is accelerated down a hollow metal tube, the gun barrel, by an expanding cloud of hot gases generated by the ignition of a quantity of gunpowder, although there are guns that use other sources of gas such as CO2 or compressed air to propel their missiles. Some of the latter can achieve velocities comparable to gunpowder weapons, though their projectiles are usually much smaller. Nonetheless they can still produce serious and even fatal trauma. The projectiles fired from guns are usually composed of lead because of its density and relatively low melting temperature that allows it to be easily cast into various shapes. The projectiles are either cylindrical, generally with a rounded or pointed nose; (bullets), or spherical (shot). The former are used in rifled weapons and the latter in smoothbore weapons (shotguns). Rifled weapons have spiral grooves cut into the bore of the gun barrel that imparts a spin to the bullet as it passes through. This, combined with the elongated shape of the projectile, gives the projectile greater ballistic stability allowing it to travel further and straighter. In a rifled weapon, only one projectile at a time travels down the barrel, although they may be capable of firing many times in rapid succession. Long-barreled rifled weapons are called rifles and short barreled ones handguns. The internal diameter of the gun barrel is its caliber that may be given in inches or millimeters. This determines the diameter of the bullet. Shotguns are smooth bored, have no internal rifling, and are designed to fire multiple projectiles, or “load,” at once. This load of shot spreads out after leaving the barrel to produce a cloud of projectiles, the better to strike a small moving target, such as a flying bird. Small shot for hunting birds is called “birdshot” and larger shot or pellets for bigger game is called “buckshot.” The diameter or bore of a shotgun is described in terms of its “gauge” (which is, for larger bore guns, the number of lead balls the diameter of the barrel that it takes to make up a pound). Both bullets and shot vary in size, but bullets also show considerable variation in shape while shot is always spherical. Bullets may be composed solely of lead or may be coated with another metal, “jacketed.” These variations in shape and covering, in addition to variation in size (caliber), are intended to enhance the performance of the gun and/or the bullet. Lead shot may also be thinly coated with another metal and some shot are made of steel to curb lead poisoning in birds who ingest the spent shot while feeding. Large single projectile rounds, usually referred to as slugs, may be used in shotguns for larger game. Early guns, both long barreled and short, were smooth bored and usually fired single lead balls.
A bullet striking the body may not only penetrate it but may also pass completely through the body. Gunshot wounds are the most common form of perforating injuries. For medicolegal purposes, it is critical to distinguish wound entrances from exits, and it is ordinarily possible to do so in the case of gunshot wounds and often stabs and other perforating trauma.
Entry bullet wounds: When a bullet impacts a surface perpendicularly in a nose first configuration, it produces a defect that is rounded and regular in appearance. On the skin, there is often a thin collar of abrasion at the margins of the defect. Lead or other residue on the bullet may also be deposited at this margin and appear as an encircling fine gray residue or “wipe-off.” If the impact is at an acute angle, the defect may be elongated or elliptical in shape. The configuration of the nose of the bullet will to some degree affect the appearance of the defect as well as the presence of intervening clothing. Typically the actual defect is slightly smaller than the diameter of the projectile. Individual shotgun pellet entry wounds will have the same appearance as bullet entry wounds (Figure 3-7 left).
Exit bullet wounds: When a projectile exits the body, it tends to produce an irregular wound as the skin is stretched outward from within. Since the projectile is not impacting the epidermis, there is no abrasion collar. The projectile may have expanded or become distorted during its passage through the body or in the case of a bullet may now be traveling sideways or base forward so that the defect it produces is usually larger than the diameter of the projectile. It is generally the case, (with important exceptions), that an exit wound is larger than the corresponding entrance wound (Figure 3-7 right).
The core of disruption that a projectile produces along its course is related to the size of the projectile and its velocity, that is, its kinetic energy. As bullets become larger and/or move faster, they tend to produce more damage to the organs and tissues that they pass through. As a bullet becomes heavier, it also becomes larger and thus has a greater cross section leading to a larger path of injury. Some bullets are designed to expand as they pass through tissue also increasing their cross-sectional area. Similarly longer bullets tend to tumble or “yaw” as they pass through tissue and the greater exposed surface produces a larger and potentially more destructive wound track. If a bullet fragments and disperses into the tissues, it may produce more damage than a bullet that remains intact and bone struck by projectiles can also fragment and be driven into tissues along the wound track.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree