Endocrine Pathology
PITUITARY
General Principles
Where is the pituitary gland located?
In the sella turcica near the optic chiasm and cavernous sinus
What are the two distinct parts of the pituitary gland?
- Anterior lobe (adenohypophysis)
- Posterior lobe (neurohypophysis)
What is the origin of the anterior lobe?
Rathke pouch—oral cavity
What is the portal vascular system of the anterior pituitary?
A transport system for circulating hormones between the hypothalamus and anterior pituitary
What are the major cell types in the anterior pituitary?
Somatotrophs; lactotrophs; corticotrophs; thyrotrophs; gonadotrophs
Table 11.1 Pituitary Hormones
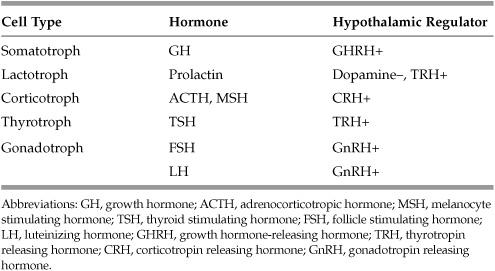
Prolactin release has a negative feedback mechanism—prolactin increases dopamine release from the hypothalamus, dopamine then inhibits prolactin secretion. Therefore, an increase in dopamine results in a decrease in prolactin, and a decrease in dopamine (as seen with many antipsychotics) results in an increase in prolactin.
What is the embryologic origin of the posterior pituitary?
Neuroectoderm—outpouching of the third ventricle with modified glial and axonal components from supraoptic and paraventricular nuclei
What hormones are produced in the hypothalamus and stored in the posterior pituitary?
Oxytocin; vasopressin (antidiuretic hormone [ADH])
What are the effects of oxytocin on the human body?
Contracts the uterus and lactiferous ducts in mammary glands
When is vasopressin secreted from the posterior pituitary?
Decreased blood volume; increased osmolarity
What role does vasopressin play in the kidney?
Saves water by increasing permeability at collecting ducts, ie, antidiuretic hormone
Anterior Pituitary Pathology
What is the visual field defect that occurs in patients with pituitary adenomas?
Bitemporal hemianopsia
What is the field defect caused by?
Compression of the optic nerve at the optic chiasm
What do pituitary adenomas look like histologically?
Uniform monoclonal polygonal cells in cords or sheets
What is the most common type of hyperfunctioning pituitary adenoma?
Prolactinoma
What are the symptoms associated with a prolactinoma?
Amenorrhea, galactorrhea, erectile dysfunction (in males), ± visual field deficit
Elevated levels of prolactin suppress secretion of follicle stimulating hormone (FSH) and luteinizing hormone (LH)
What are the histologic findings consistent with prolactinoma?
Lactotroph hyperplasia with secretory granules on immunohistochemical staining
What are other causes of hyperprolactinemia?
Medications; cirrhosis; hypothyroidism; stress
Which drugs can cause galactorrhea?
Neuroleptics/antipsychotics (eg, haloperidol); reserpine (antihypertensive); phenothiazines; metoclopramide
By what mechanism do most drugs cause galactorrhea?
Blocking dopamine receptors thereby releasing inhibition of prolactin
What is the treatment for galactorrhea?
Bromocriptine (dopamine agonist)
What is acromegaly?
The result of continued stimulation by excess growth hormone (GH) after closure of the epiphyseal plates (ie, adults), characterized by frontal bossing (prominent forehead), large head, nose, hands, protruding jaw, thick tongue, and deepening of the voice
What syndrome is caused by growth hormone adenoma of the pituitary in a child who is still growing (epiphyses have not closed)?
Gigantism
What oncogene is associated with growth hormone adenomas?
GSP oncogene
What is the treatment for growth hormone adenomas?
Surgical removal of tumor or radiation
What is Cushing disease?
Elevated serum cortisol secondary to corticotroph cell (ACTH releasing) pituitary adenoma, resulting in weight gain, truncal obesity, abdominal striae, buffalo hump, headaches, hypertension, irregular menses, hyperpigmentation of the skin
Also an increase in serum cortisol with similar symptoms (except for hyperpigmentation), but secondary to an adrenal adenoma or carcinoma releasing cortisol
Is Cushing disease or syndrome more common?
Cushing disease—accounting for ∼70% of cases
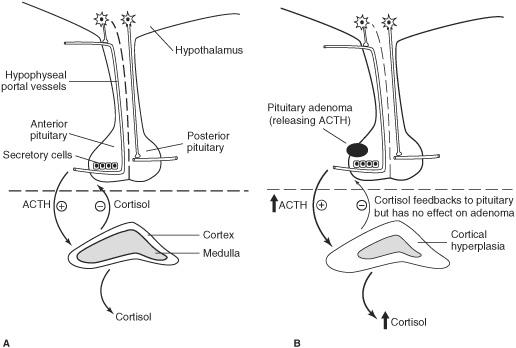
Figure 11.1 A. Normal pituitary-adrenal axis. B. Cushing disease.
What is the syndrome that is associated with pituitary microadenoma, bitemporal hemianopsia, hyperpigmentation, and Cushing syndrome?
Nelson syndrome
What is the cause of Nelson syndrome?
The loss of the inhibitory effect of corticosteroids on a corticotroph adenoma of the pituitary. The adenoma increases in size after removal of bilateral adrenal glands for treatment of Cushing syndrome.
What are the symptoms of a gonadotroph adenoma of the pituitary gland?
No recognizable syndrome; decreased libido; amenorrhea
What are the symptoms of a thyrotroph adenoma of the pituitary gland?
Tachycardia, palpitations, weight loss, and diarrhea
What are null-cell adenomas of the pituitary?
Nonfunctional adenomas, a cause of hypopituitarism
What is pituitary apoplexy?
Sudden hemorrhage into a pituitary adenoma which can result in panhypopituitarism
What is the treatment for the symptoms of hypopituitarism that occur with pituitary apoplexy?
Glucocorticoids and thyroid hormones
What is Sheehan syndrome?
Postpartum ischemic necrosis of the pituitary, often resulting in panhypopituitarism
What is the cause for Sheehan syndrome?
During pregnancy the size of the pituitary gland increases. At delivery, severe hemorrhage or shock causes anoxic injury of the anterior pituitary.
What is the treatment for Sheehan syndrome?
Give glucocorticoids due to decreased ACTH and thyroid hormones due to decreased thyroid-stimulating hormone (TSH).
Posterior Pituitary Pathology
What are the classic features of central diabetes insipidus (DI)?
Increased frequency and volume of urination; increased thirst; polydipsia
What will serum and urine lab tests find in patients with central DI?
- Serum—increased sodium and osmolarity
- Urine—negative glucose and low osmolarity
What is the underlying cause for central DI?
Damage to posterior pituitary
What hormone is lacking in central DI?
ADH
What are the common causes of central DI?
Head trauma (including surgery or radiation); tumor; sarcoidosis
What is the treatment for central DI?
Vasopressin/desmopressin
What is the other mechanism/form of diabetes insipidus?
Nephrogenic DI—renal tubules are unresponsive to ADH
Are ADH levels increased, decreased, or normal in nephrogenic DI?
Normal to increased levels
What drugs can cause nephrogenic DI?
Lithium; demeclocycline; methoxyflurane
What is the treatment for nephrogenic DI?
Thiazides
What is the most common presentation of syndrome of inappropriate secretion of antidiuretic hormone (SIADH)?
Altered mental status
What are the common causes of SIADH?
Neoplasm (paraneoplastic syndrome, especially associated with small cell carcinoma of the lung); infections—(meningitis, encephalitis, pneumonia); pain and nausea (especially in perioperative period); mediations (narcotics, carbamazepine); pituitary injury (release of oxytocin)
What is the urine like in patients with SIADH?
Inappropriately concentrated urine
What are the treatments for SIADH?
Fluid restriction; demeclocycline—inhibits ADH effect on renal tubules
What is the dreaded complication that may occur with rapid correction of sodium levels in a patient with SIADH?
Central pontine myelinolysis—acute, noninflammatory demyelination of neurons occurring predominately within the pons of the brain stem
THYROID
General Principles
What is the embryologic origin of the thyroid?
Pharyngeal epithelium
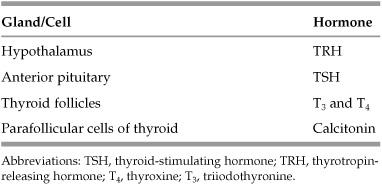
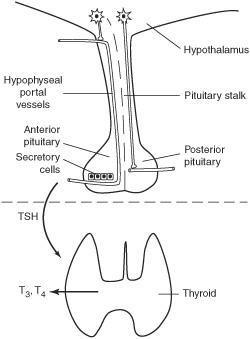
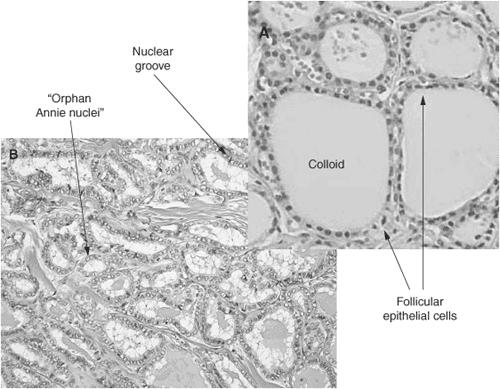
Figure 11.2 Normal thyroid (euthyroid).
What is the role of thyroid hormones in the body?
Increase basal metabolic rate; β-adrenergic effects; bone growth (along with GH); central nervous system (CNS) maturity
What mineral is necessary for thyroid hormone synthesis?
Iodine
What transports thyroid hormone (T3/T4) in the blood?
Thyroxine-binding globulin (TBG); only the free, unbound hormone is active
Which is more potent T3 or T4?
T3 binds to receptors with greater affinity than T4; however, T4 is the major product of the thyroid, which is then converted to T3 peripherally
Hyperthyroidism
What are the symptoms of hyperthyroidism?
Palpitations, weakness, nervousness/anxiety, weight loss, diarrhea, intolerance to heat, tremor
What are the common causes of hyperthyroidism?
Grave disease; exogenous thyroid hormone; hyperfunctional goiter (multinodular goiter) or thyroid adenoma; thyroiditis
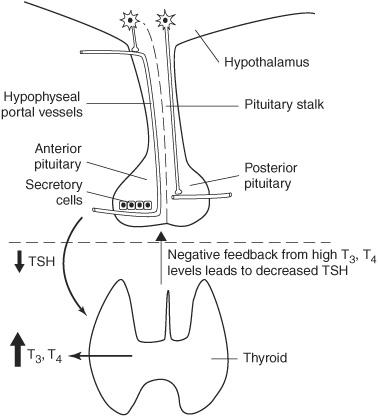
Figure 11.3 Hyperthyroidism (most commonly Grave disease).
What are the less common causes of hyperthyroidism?
Struma ovarii; TSH-secreting pituitary adenoma; choriocarcinoma/hydatidiform mole
What is the most common cause of endogenous hyperthyroidism?
Grave disease
What is the triad of Grave disease?
Hyperthyroidism; Ophthalmic pathology (exophthalmos); Pretibial myxedema
*Grave disease makes you HOP
What is pretibial myxedema?
Skin that overlies shins is thick and indurated, resembling an orange peel. (Rare complication of Grave disease.)
What are other abnormal physical examination findings associated with Grave disease?
Bruit over enlarged thyroid; lid lag; proptosis; weak extraocular muscles
What is the cause of Grave disease?
Development of an autoantibody which stimulates the TSH receptor
What type of immunoglobulin is the autoantibody?
Immunoglobulin G (IgG)
What HLA types are associated with Grave disease?
HLA-DR3 and HLA-B8
What other diseases are commonly found in people with Grave disease?
Systemic lupus erythematosus (SLE); pernicious anemia; diabetes mellitus (DM) type I; Addison disease
What is the morphology of the thyroid gland in Grave disease?
Diffusely enlarged gland, with hypertrophy and hyperplasia
What lab abnormalities are seen in Grave disease?
Increased T3 and T4; decreased TSH
What is the treatment for Grave disease?
Propylthiouracil (PTU); ablation by radiation; surgical removal
What cause of hyperthyroidism most commonly occurs in postpartum women and histologic findings on biopsy show a lymphocytic infiltrate?
Subacute lymphocytic thyroiditis
What are the other names for subacute lymphocytic thyroiditis?
Silent or painless thyroiditis
Which HLA types are associated with subacute lymphocytic thyroiditis?
HLA-DR3 and HLA-DR5
What rare cause of thyroiditis is characterized by extensive fibrosis of the thyroid gland?
Riedel thyroiditis
What syndrome consists of hyperthyroidism with goiter but lacks the ophthalmic and dermatologic characteristics of Grave disease?
Plummer syndrome
What causes thyroid goiters to form?
Impaired synthesis of thyroid hormones
Do multinodular goiters cause hyperthyroidism, hypothyroidism, both, or neither?
Most are euthyroid, but a small percentage are hyperfunctioning
Hypothyroidism
What are the signs and symptoms of hypothyroidism?
Weight gain, cold intolerance, fatigue, depression, constipation, brittle hair, cool skin, and decrease deep tendon reflexes (DTRs)
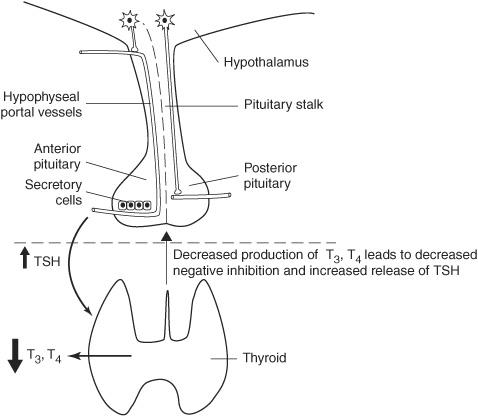
Figure 11.4 Hypothyroidism (most commonly Hashimoto thyroiditis).
What drugs can cause hypothyroidism?
Lithium; amiodarone; propylthiouracil (PTU)
What diseases are associated with hypothyroidism?
Sarcoidosis; amyloidosis; carpal tunnel syndrome
What dietary deficiency can result in thyroid goiters and hypothyroidism?
Iodine deficiency
Iodine deficiency in utero results in what disease?
Congenital hypothyroidism (formerly known as cretinism), typically picked up on newborn screening but can present with mental retardation, short stature, hypotonia, and macroglossia
What is the most common cause of hypothyroidism?
Hashimoto thyroiditis
What physical examination finding of the thyroid is associated with Hashimoto thyroiditis?
Rubbery, nontender diffusely enlarged thyroid
What is the typical presentation of Hashimoto thyroiditis?
Transient hyperthyroidism followed by chronic hypothyroidism
What is the cause of Hashimoto thyroiditis?
Autoimmune destruction of the thyroid gland
What are the histologic features of Hashimoto thyroiditis?
Extensive lymphocytic cell infiltrate, atrophic lymphoid follicles, and Hürthle cell metaplasia
What human leukocyte antigen (HLA) type is associated with Hashimoto thyroiditis?
HLA-DR3 and HLA-DR5
What are some of the autoantibodies (AB) associated with Hashimoto thyroiditis?
Antimicrosomal antibody; anti-TSH receptor antibody
What other autoimmune diseases are seen in patients with Hashimoto thyroiditis?
Systemic lupus erythematosus (SLE); rheumatoid arthritis (RA); Sjögren syndrome; pernicious anemia; autoimmune adrenalitis; type I diabetes
For what type of cancers are people with Hashimoto thyroiditis at higher risk?
B-cell lymphomas of the thyroid gland
What are other names for de Quervain thyroiditis?
Subacute granulomatous thyroiditis
What makes de Quervain thyroiditis unique?
“Painful” thyroid compared to subacute lymphocytic thyroiditis which is classically “painless”; may be preceded by viral upper respiratory infection
What viruses have been associated with de Quervain thyroiditis?
Mumps; coxsackie virus; adenovirus
What HLA type is associated with de Quervain thyroiditis?
HLA-B35
What does de Quervain thyroiditis show microscopically?
Multinucleate giant cells, granulomatous inflammation
Neoplastic
A young adult, female patient has a solitary, painless neck mass. What is the most likely diagnosis?
Thyroid adenoma
True or False? The vast majority (>90%) of discrete solitary masses of the thyroid are benign:
True
What are some features that make a lesion of the thyroid suspicious for cancer?
Solitary lesion; radiation history; cold nodule; female sex
What are some features that are poor prognostic factors?
Age >45 years; male sex; extension of tumor beyond the thyroid; metastasis
When a solitary lesion is detected, what is the next step in diagnosis?
Fine needle aspiration (FNA)
What is the most common type of thyroid cancer?
Papillary carcinoma
* Papillary is the most Popular
What microscopic findings distinguish papillary carcinoma from other types?
Psammoma bodies; glandular cells are arranged in a papillary architecture; orphan Annie nuclei; nuclear grooves
Figure 11.5 A. Benign thyroid tissue composed of colloid-producing follicles. Parafollicular C cells are located in the interstitium. B. Papillary thyroid carcinoma with nuclear grooves, intranuclear inclusions (not really visible at this magnification), empty appearing nuclei (“orphan Annie nuclei”), and back-to-back follicles with little intervening interstitium. (Reproduced, with permission, from Wettach T, et al: Road Map Pathology, New York: McGraw-Hill, 2009; fig 11-2.)
What familial syndromes have an increased risk of developing papillary carcinomas?
Gardner syndrome; familial adenomatous polyposis (FAP); Cowden syndrome (familial goiter/skin hamartomas)
What is the second most common type of thyroid carcinoma (10%-20%)?
Follicular carcinoma
What is seen microscopically in follicular carcinoma?
Microfollicular hyperplasia with invasion into surrounding thyroid tissue (as opposed to adenoma, which has microfollicular hyperplasia but is encapsulated and does not invade)
What is the third most common type of thyroid carcinoma (5%)?
Medullary carcinoma
What cell type is associated with medullary carcinoma?
Parafollicular C cells
What is seen microscopically in medullary carcinoma?
Neuroendocrine cells arranged in nests or neuroendocrine spindle cells invading into surrounding normal thyroid tissue. Tumor cells immunostain for TTF-1 and calcitonin. Amyloid deposits are often present.
What substance do the parafollicular C cells normally secrete?
Calcitonin
What other substances do medullary carcinomas of the thyroid secrete besides large amounts of calcitonin?
Serotonin; vasoactive intestinal peptide (VIP); somatostatin
What familial syndrome is associated with an increased risk of medullary thyroid carcinoma?
Multiple endocrine neoplasia (MEN) 2A and 2B
What are the three most important things to remember about medullary carcinoma?
- MEN syndromes 2A and 2B
- Amyloid
- C-cells/Calcitonin
*MED student named MAC
What is the least common type of thyroid carcinoma?
Anaplastic carcinoma
What is unique about anaplastic thyroid carcinoma?
Very aggressive; poorly differentiated microscopically; metastasizes to lungs
PARATHYROID
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree