Gastrointestinal Pathology
EMBRYOLOGY
From which embryologic tissue are most gastrointestinal organs derived?
Endoderm
During which weeks of embryologic development does most visceral organ development occur?
Organogenesis occurs between weeks 3 and 8.
Through what structure does blood flowing to fetus through the umbilical vein arrive in the inferior vena cava?
The ductus venosus
Which adult structure does the umbilical vein ultimately give rise to?
The falciform ligament which contains the ligamentum teres
Which four structures give rise to the diaphragm?
- Septum transversum
- Dorsal mesentery of the esophagus
- Pleuroperitoneal folds
- Body wall
What adult structures does the ventral pancreatic bud ultimately give rise to?
Main pancreatic duct, uncinate process, and head of the pancreas
What adult structures does the dorsal pancreatic bud ultimately give rise to?
Accessory pancreatic duct and body, isthmus, and tail of the pancreas
Into which three sections is the primitive gut divided?
- Foregut (pharynx to duodenum)
- Midgut (duodenum to transverse colon)
- Hindgut (distal transverse colon to rectum)
ANATOMY
In which way is the division of the primitive gut anatomically relevant?
The division corresponds to anatomic regions of shared blood supply. The foregut is supplied by the celiac trunk, the midgut is supplied by the superior mesenteric artery, and the hindgut is supplied by the inferior mesenteric artery.
Which other gastrointestinal organs are supplied by the celiac trunk?
Liver, gallbladder, and pancreas
What are the three main branches of the celiac trunk?
- Common hepatic artery
- Splenic artery
- Left gastric artery
What are the different anatomic regions of the stomach?
Cardia, fundus, body, antrum, and pylorus
Which gastrointestinal organs are located in the retroperitoneum?
Second, third, and fourth portions of the duodenum, descending colon, ascending colon, and most of the pancreas (except the tail)
Which three ligaments are connected to the liver?
- Falciform
- Hepatoduodenal
- Gastrohepatic ligaments
What structures are contained in the hepatoduodenal ligament?
The hepatic artery, portal vein, and common bile duct
What structures are contained in the gastrohepatic ligament?
The gastric arteries
What is the difference in vascularization above and below the pectinate line?
Above the pectinate line is supplied by the superior rectal artery and drained by the superior rectal vein which drains to the portal vein. Below the pectinate line is supplied by the inferior rectal artery and drained by the inferior rectal vein which drains to the IVC.
Name three major salivary glands associated with the oral cavity:
- Parotid
- Submandibular
- Sublingual
A congenital defect in which an abnormal ring or collar of pancreatic tissue encircles the duodenum, causing nausea, vomiting, feeling of fullness, and feeding intolerance in the newborn
HISTOLOGY
What kind of epithelium lines the oral cavity?
Nonkeratinized stratified squamous epithelium
What kind of epithelium lines the esophagus?
Nonkeratinized stratified squamous epithelium
What are the three layers of esophageal mucosa?
- Epithelium
- Lamina propria
- Muscularis mucosa
Describe the muscles of the esophagus:
The upper third of the esophagus contains skeletal muscle, the middle third has both skeletal and smooth muscle, and the lower third consists entirely of smooth muscle.
What type of epithelium lines the stomach?
Simple columnar epithelium
What cell types are found within gastric glands and what do they produce?
- Parietal cells—produce HCI and intrinsic factor
- Mucosal neck cells and lining cells—produce protective mucus
- Neuroendocrine system cells—produce various hormones
- Regenerative cells
- Chief cells—produce precursor enzymes
How is the gastric mucosal barrier maintained?
Through constant mucus and bicarbonate secretion, mucosal blood flow, and prostaglandin synthesis
Name the layers of the wall of the intestine:
From internal to external: mucosa (epithelium, lamina propria, muscularis mucosa), submucosa, muscularis externa, and serosa/adventitia
Where is the submucosal plexus located?
Between the submucosa and the inner layer of the muscularis
What do neurons in the submucosal plexus predominately regulate?
Local secretions, blood flow, and absorption
Where is the myenteric plexus located?
Between the inner (circular) and outer (longitudinal) layers of the muscularis
What do neurons in the myenteric plexus predominately regulate?
Gut motility
What type of epithelium lines the small intestine?
Simple columnar epithelium
What is the major function of the small intestine?
Absorption and enzymatic digestion of amino acids, monosaccharides, and lipids
What determines the absorptive capacity of the small intestine?
Available surface area (mucosal folds, villi, and microvilli)
What type of epithelium lines the large intestine?
The colon is lined by simple columnar epithelium. The anus is lined by simple columnar epithelium to the rectum, then simple cuboidal epithelium to the anal valves, and finally, stratified squamous epithelium beyond the anal valves.
Where are Brunner glands located and what is their function?
In the submucosa of the duodenum—they produce alkaline secretions to neutralize acidic stomach contents
What are the functions of the liver?
Synthesis of serum proteins; processing of dietary amino acids, carbohydrates, lipids, and vitamins; detoxification of pollutants; secretion of endogenous waste products into bile
What laboratory values are used to evaluate hepatocyte function and biliary excretion?
- Hepatocyte function—AST, ALT, lactate dehydrogenase (LDH), serum albumin, prothrombin time (PT), and serum ammonia
- Biliary excretion—serum bilirubin, urine bilirubin, serum alkaline phosphatase, serum γ-glutamyl transpeptidase, and serum 5-nucleotidase
MOUTH AND ESOPHAGUS
Congenital
What is cleft lip?
A failure of fusion of the maxillary and medial nasal processes during embryologic development resulting in a gap in the upper lip while the palate remains intact
What is cleft palate?
A failure of fusion of the lateral palatine processes, the nasal septum, and/or the median palatine processes. The resulting gap leaves the nasal cavity in communication with the oral cavity.
What are the most common congenital anomalies of the esophagus?
Esophageal atresia and tracheoesophageal fistula (TEF)
Define atresia:
The absence of a luminal opening
What is the most frequent type of TEF?
A distal TEF with proximal esophageal atresia
Anatomic
What is achalasia?
The incomplete relaxation of the lower esophageal sphincter with consequent dilatation of the proximal esophagus due to the loss of the myenteric plexus
What is typical of achalasia on barium esophagogram?
“Bird beak” appearance with distal esophageal stenosis and proximal dilation, may see air-fluid (or contrast) line in upper esophagus
What disease causes secondary achalasia and frequently occurs in South America?
Chagas disease
What are the clinical signs and symptoms of achalasia?
Progressive dysphagia, nocturnal regurgitation, aspiration pneumonia, weight loss, cough, and airway obstruction
What malignancy is associated with achalasia?
Esophageal carcinoma
What is diffuse esophageal spasm (DES)?
An esophageal motor disorder due to a functional imbalance between excitatory and inhibitory postganglionic neurons
What is typical of DES on barium esophagogram?
A “cork screw” pattern
What are the clinical signs and symptoms of DES?
Dysphagia and diffuse chest pain
What is the difference between a Mallory-Weiss tear and Boerhaave tear?
A Mallory-Weiss tear is a partial-thickness tear usually at the gastroesophageal junction. Boerhaave tear is a full-thickness perforation in the distal third of the esophagus. Both are associated with recent vomiting.
What factors contribute to esophageal tears or perforation?
Forceful vomiting, gastroesophageal reflux disease (GERD), and procedures such as endoscopy, dilation/intubation of the esophagus, and placement of a nasogastric tube
What are varices?
Tortuous, dilated veins—frequently involving the esophageal, rectal, and epigastric vessels
What condition is associated with esophageal varices?
Portal hypertension
What are the clinical signs and symptoms of esophageal varices?
Patients are usually asymptomatic, but if varices rupture, they can present with hematemesis or lower gastrointestinal (GI) bleed.
Infectious
What are common, painful, recurrent ulcerations of the oral mucosa known as?
Cold sores (aphthous ulcers)
What is the causative agent of cold sores?
Herpes simplex virus (HSV) (usually type 1)
HSV transmission requires intimate contact with a person actively shedding the virus
- Type 1 (oral)—transmission via direct contact with lesions through kissing or sharing utensils
- Type 2 (genital)—transmitted sexually or perinatally from infected mother to baby
How does herpes gingivostomatitis manifest in young children (primary infection)?
Fever, sore throat, erythema, and pharyngeal edema, usually followed by ulcerative lesions on the oral and pharyngeal mucosa
What are the diagnostic tools used in HSV detection?
Tzanck test of the vesicular fluid, polymerase chain reaction (PCR), and viral culture
What are the classic microscopic changes seen in herpes infection?
Infected cells clump together to form multinucleated giant cells with eosinophilic, intranuclear viral inclusions
How does Candida albicans infection of the mouth or esophagus appear clinically?
Patients present with whitish plaques of curd-like material which can be scrapped off of the mucosal surface.
Who is likely to get oral candidiasis?
Patients undergoing chemotherapy, those with diabetes, chronic debilitating diseases, acquired immunodeficiency syndrome (AIDS) or other types of immunodeficiency, patients on antibiotics, and infants.
What is sialadenitis?
Inflammation of the major salivary glands
What causes sialadenitis?
Etiology can be viral, bacterial, traumatic, or autoimmune.
What are the most common bacterial causes of sialadenitis?
Staphylococcus aureus and Streptococcus viridans
What is a common viral cause of sialadenitis?
Mumps
What are some infectious causes of esophagitis in immunosuppressed patients?
Herpes simplex virus (HSV), cytomegalovirus (CMV), and Candida albicans
Trauma
What is leukoplakia?
An irregular, whitish patch/plaque caused by epidermal thickening or hyperkeratosis and is believed to be a defense or reparative response to insult. Whereas candidiasis lesion can be scrapped off with mechanical forces, leukoplakia cannot.
What are the most common sites of leukoplakia on the oral cavity?
The vermilion border of the lower lip, the buccal mucosa, and the hard/soft palate
What are the common causes of leukoplakia?
Trauma; tobacco use; alcohol use; infection (Epstein-Barr virus [EBV], syphilis); chemical irritation
What percentage of oral leukoplakia is premalignant (dysplastic)?
5% to 25%
Define a mucocele:
A common lesion of the salivary glands that develops from the accumulation of saliva secondary to blockage and/or rupture of salivary gland ducts
What is the most common cause of mucocele formation?
Trauma
Neoplasm
What is erythroplasia?
A clinical term used to describe lesions of the mucous membranes which are red and nonulcerated
What percentage of erythroplasia undergoes malignant transformation?
More than 50%
The majority of oral cavity malignancies are what type of cancer?
Squamous cell carcinoma
What is the most common age group affected?
Patients older than 40 years
What are the risk factors for oral cancer?
Tobacco use, human papillomavirus (HPV) infection, leukoplakia, erythroplasia, alcohol abuse, and chronic irritation
What are the most common locations of squamous cell carcinoma in the oral cavity?
Ventral surface of the tongue, lower lips, floor of the mouth, gingiva, and soft palate
What is the most frequent site of salivary gland tumors?
Parotid gland (65%-80%)
What is the percentage of parotid gland tumors that are benign?
70% to 80%
What is the most common salivary gland tumor?
Pleomorphic adenoma (also known as “mixed tumor”)
What are the key characteristics of pleomorphic adenomas?
They are benign, painless, slow-growing, and have a tendency to recur. Pleomorphic adenomas have been reported to undergo malignant transformation.
What are two other common salivary gland tumors?
- Warthin tumor
- Mucoepidermoid carcinoma
What are the key features of a Warthin tumor?
Second most common salivary gland tumor; benign; male > female; smokers > nonsmokers; affects mainly the parotid glands; gross appearance—often multicystic containing “crankcase oil”-like fluid
What is the classic microscopic finding of a Warthin tumor?
Double layer of neoplastic epithelial cells on a reactive lymphoid stroma
What is a key epidemiologic feature of mucoepidermoid carcinomas?
They are the most common type of salivary gland malignancy in children.
What is the classic microscopic finding of mucoepidermoid carcinomas?
Variable mixture of squamous and mucin-producing cells in a cystic or sheet-like pattern
What is the most common malignancy of the esophagus worldwide?
Squamous cell carcinoma
What are the common risk factors for squamous cell carcinoma of the esophagus?
- Alcohol consumption*
- Tobacco use*
- Long-standing esophagitis
- Achalasia
- Vitamins A, C, thiamine, or pyridoxine deficiency
- High content of nitrites/nitrosamine in diet
- Fungal contamination of food
- Familial
*These are the biggest risk factors and the combination exponentially increases the risk of carcinoma. (This is an example of synergism.)
Inflammatory/Autoimmune
What systemic inflammatory conditions are associated with aphthous ulcerations in the mouth?
Inflammatory bowel disease and Behçet disease
What is an autoimmune cause of sialadenitis?
Sjögren syndrome (bilateral)
What is the clinical presentation of Sjögren syndrome?
Dry mouth (xerostomia), dry eyes (keratoconjunctivitis sicca), an associated second connective tissue disease, and parotid gland enlargement
Sjögren syndrome is associated with what type of malignancy?
Lymphoma
What are the key characteristics of Plummer-Vinson syndrome?
Iron deficiency anemia, glossitis, and esophageal webs
What are esophageal webs?
Thin membranes of normal esophageal tissue (including mucosa and submucosa) appearing in the middle to lower third of the esophagus causing pain and dysphagia (solids > liquids)
What are patients with Plummer-Vinson syndrome at increased risk of?
Squamous cell carcinoma of the pharynx/esophagus
What is esophagitis?
Inflammation of esophageal mucosa
What conditions lead to esophagitis?
GERD, Barrett esophagus, infections, and chemical irritation
Gastroesophageal reflux disease in which stomach acid refluxes into the esophagus
What are common causes of GERD?
Inappropriate relaxation of the lower esophageal sphincter, a sliding hernia, inadequate esophageal clearance, and delayed gastric emptying
What substances decrease the tone of the lower esophageal sphincter?
Coffee, cigarettes, alcohol, progesterone (pregnancy), chocolate, and calcium channel blockers
What are the classic symptoms of GERD?
Heartburn (often related to eating or lying supine), a sour taste in the mouth, and abdominal or chest pain
What are the complications of GERD?
Esophageal strictures, ulcers, hemorrhage, Barrett esophagus, and esophageal adenocarcinoma
What is Barrett esophagus?
A complication of long-standing GERD that results in intestinal metaplasia in which stratified squamous epithelium above the gastroesophageal junction is replaced with intestinal-type columnar epithelium including goblet cells.
What are the complications of Barrett esophagus?
Adenocarcinoma, stricture, and ulceration
STOMACH
Congenital
Define congenital pyloric stenosis:
Muscular hypertrophy of the pyloric smooth muscle wall causing obstruction
What are the key clinical features of pyloric stenosis?
Palpable mass (“olive”) in the epigastric region; persistent, nonbilious projectile vomiting in young infants; male > female
What do the common imaging studies show in patients with pyloric stenosis?
- X-ray—dilated stomach bubble
- Ultrasound—elongated pyloric channel (>14 mm) and thickened pyloric wall (>4 mm)
Infectious
What is H. pylori?
A spiral, microaerophilic, gram-negative bacterium that infects the mucosal layer of the GI tract and produces urease and cytotoxins
How is H. pylori transmitted?
Not well-defined, but may be transmitted via fecal-oral route
What malignancies are associated with chronic H. pylori infection?
Adenocarcinoma and lymphoma of the stomach
How is H. pylori diagnosed?
Biopsy, serological testing for H. pylori antibody, or urease breath test
What percentage of people infected with H. pylori develop peptic ulcers?
10% to 20%
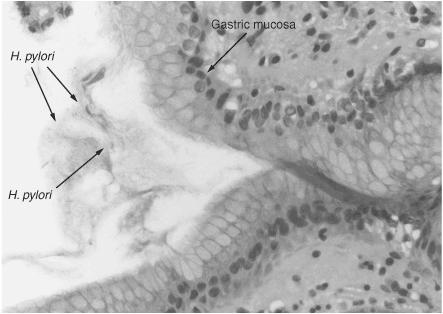
Figure 8.1 Mucosa of gastric fundus. Comma and rod-shaped H. pylori are present in fundic gland secretions. (Reproduced, with permission, from OHSU.)
Neoplasm
What are common examples of benign gastric neoplasms?
Leiomyomas; hyperplastic polyps; fundic gland polyps; adenomas
What are the most common malignant tumors of the stomach?
Gastric carcinoma (90%-95%), GI lymphoma, and carcinoid tumors
What are the risk factors for developing gastric carcinoma?
Chronic gastritis; dietary nitrates/smoked food/pickled vegetables; decreased intake of fresh fruits/vegetables; H. pylori infection; history of adenomatous polyps
What is linitis plastica (leather bottle stomach)?
Diffuse gastric cancer that results in a thickened, rigid stomach caused by the extensive infiltration of neoplastic cells in the gastric wall
What is the name for a firm, palpable left supraclavicular lymph nodes that represents metastatic carcinoma, typically from a primary carcinoma in the thoracic or abdomen?
Virchow node
What is a Krukenberg tumor?
Metastasis of gastric adenocarcinoma to the ovaries. Histologically, these tumors often have signet-ring cell features.
What are the clinical signs and symptoms of gastric carcinoma?
Weight loss, abdominal pain, dysphagia, anorexia, nausea, and vomiting
Inflammatory/Autoimmune
What is chronic gastritis?
Mucosal inflammation with lymphocytic and plasma cell infiltrates leading to gastric gland loss, mucosal atrophy, and intestinal metaplasia
What are the two types of chronic gastritis?
- Type A or autoimmune chronic gastritis—caused by antibodies to parietal cells
- Type B or infectious chronic gastritis—caused by H. pylori
To which part of the stomach does autoimmune chronic gastritis localize?
The body of the stomach
To which part of the stomach does infectious chronic gastritis localize?
The antrum of the stomach
What is acute gastritis?
Mucosal inflammation with edema and a predominately neutrophil inflammatory infiltrate
What are common causes of gastritis?
Heavy use of nonsteroidal anti-inflammatory drugs (NSAIDs); alcohol consumption and smoking; treatment with chemotherapy; uremia; systemic infection; severe stress (trauma, burn, surgery); ischemia and shock; suicidal ingestion of acids and alkali; mechanical trauma
What is the clinical presentation of gastritis?
Usually asymptomatic, but can cause nausea, vomiting, abdominal pain, hematemesis, and melena
What are peptic ulcers?
Chronic, usually solitary, punched-out erosions of the mucosa occurring mainly in the duodenum or stomach, but can be found in any portion of GI tract exposed to gastric acid and pepsin
What is the classical presentation of PUD?
Localized chronic, intermittent, epigastric burning/aching/gnawing pain accompanied by nausea, vomiting, bloating, and belching
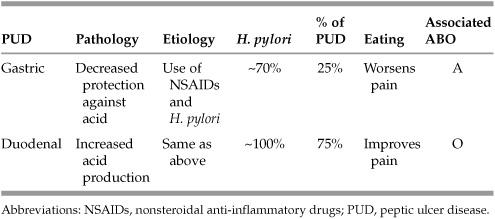
What clinical feature may help distinguish gastric ulcers from duodenal ulcers?
Abdominal pain will be greater with meals if the patient has a gastric ulcer and will decrease with meals if the patient has a duodenal ulcer
What are the complications of PUD?
Hemorrhage, perforation, and gastric outlet obstruction
What conditions are associated with PUD?
H. pylori infection, use of NSAID and/or high-dose corticosteroids, Zollinger-Ellison syndrome, central nervous system (CNS) injuries, sepsis, and extensive burns
- Triple therapy for H. pylori infection—amoxicillin/tetracycline, metronidazole, and bismuth
- Proton pump inhibitors, antacids, and H2 blockers
- Lifestyle changes—decrease tobacco and alcohol consumption
Table 8.1 Classical Differences between Duodenal and Gastric Ulcers
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


