Patient Story
A 44-year-old man presents with concern over a mole on his back that his wife says is growing larger and more variable in color. The edges are irregular and the color almost appears to be “leaking” into the surrounding skin. He reports no symptoms related to this lesion. On physical exam, the nevus is 9 mm in diameter with asymmetry and variations in color and an irregular border (Figure 165-1). A full-body skin exam did not demonstrate any other suspicious lesions. Dermoscopy showed an irregular network with multiple asymmetrically placed dots off the network (Figure 165-2). A scoop saucerization was performed with a DermaBlade taking 2-mm margins of clinically normal skin (Figure 165-3). Although this could have been an early thin melanoma, the pathology showed a completely excised compound dysplastic nevus with no signs of malignancy. No further treatment was needed except yearly skin exams to monitor for melanoma.
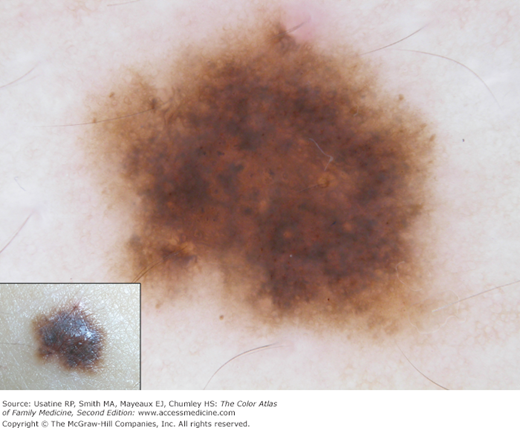
Figure 165-3
A scoop saucerization was performed with a DermaBlade taking 2-mm margins of clinically normal skin. Although this could have been an early thin melanoma, the pathology showed a completely excised compound dysplastic nevus with no signs of malignancy. (Courtesy of Richard P. Usatine, MD.)
Introduction
Dysplastic nevi (DN)/atypical moles are acquired melanocytic lesions of the skin whose clinical and histologic definitions are controversial and still evolving. These lesions have some small potential for malignant transformation and patients with multiple DN have an increased risk for melanoma.1
The presence of multiple DN is a marker for increased melanoma risk just as red hair is, and, analogously, cutting off the red hair or cutting out all the DN does not change that risk of melanoma. The problem with DN is that any one lesion that is suspicious for melanoma must be biopsied to avoid missing melanoma, not to prevent melanoma from occurring in that nevus in the future.
Synonyms
Atypical nevus, atypical mole, Clark nevus, nevus with architectural disorder, and melanocytic atypia.1
Epidemiology
- Two percent to 9% of the population has atypical moles (AMs).2,3 In a Swedish case-control study, 56% of cases (121 patients with melanoma) and 19% of 310 control subjects had nevi fulfilling the clinical criteria for DN.4 Among patients with melanoma, the rate of DN ranges from 34% to 59%.3 DN are uncommon in children; in a study of Swedish children (N = 524), none had DN.5 In another study of pathology reports from nevi removed from patients younger than 18 years old, 3 of 199 nevi submitted for histologic analysis met the histologic criteria for DN.6
- Individuals with fair skin types are at higher risk of DN.3
- The sudden eruption of benign and atypical melanocytic nevi has been reported and is associated with blistering skin conditions and a number of disease states, including immunosuppression. Subsets of patients with immunosuppression have increased numbers of nevi on the palms and soles.7
- The National Institute of Health Consensus Conference on the diagnosis and treatment of early melanoma defined a syndrome of familial atypical mole and melanoma (FAMM). The criteria of FAMM syndrome are:8
- The occurrence of malignant melanoma in one or more first- or second-degree relatives.
- The presence of numerous (often >50) melanocytic nevi, some of which are clinically atypical.
- Many of the associated nevi show certain histologic features (see below under BIOPSY).
- The occurrence of malignant melanoma in one or more first- or second-degree relatives.
Etiology and Pathophysiology
- Most DN are compound nevi (Figure 165-1) possessing a junctional and intradermal component (see Chapter 162, Nevus).1 The junctional component is highly cellular and consists of an irregular distribution of melanocytes arranged in nests and lentiginous patterns along the dermoepidermal junction. The dermal component, located at the center, consists of nests and strands of melanocytes with distinct sclerotic changes.1
- DN exhibit a host response consisting of irregular rete ridge elongation, subepidermal sclerosis, proliferation of dermal capillaries, and a perivascular, lymphohistiocytic inflammatory infiltrate.1
- Individuals with DN may have deficient DNA repair, and DN lesions are associated with overexpression of pheomelanin (pigment produced by melanocytes), which may lead to increased oxidative DNA damage and tumor progression.9
Diagnosis
- Variable mixtures of color including tan, brown, black, and red within a single lesion (Figures 165-4 and 165-5).
- Irregular, notched borders; pigment may fade off into surrounding skin (Figure 165-5).
- Flat or slightly raised (Figures 165-4, 165-5, and 165-6) with the macular portion at edge. Not verrucous or pendulous.
- Lesions frequently surrounded by a reddish hue from reactive hyperemia making them appear target-like.
- Usually larger than 6 mm; may be larger than 10 mm (Figures 165-1 and 165-4).
- Patients with FAMM syndrome may have more than 100 lesions, far greater than the average number of common moles (<50) in most individuals.