Chapter 16 Drugs Used in the Treatment of Coagulation Disorders
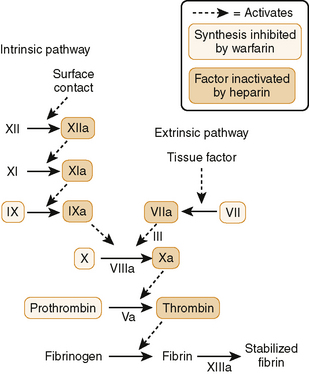
16-2 Intrinsic and extrinsic pathways of coagulation.
(From Brenner G and Stevens C: Pharmacology, 3rd ed. Philadelphia, Saunders, 2010, Figure 16-2.)
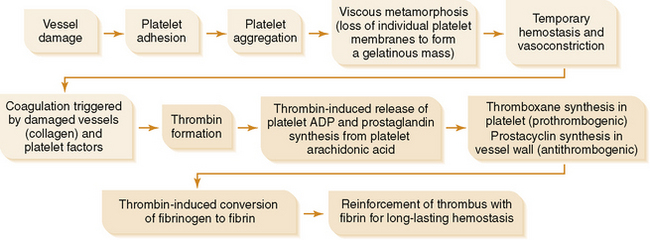
(1) All required factors (XII, XI, IX, VIII) are present in blood and coagulation is initiated by collagen from damaged blood vessel.
(4) Measured by prothrombin time (PT) or international normalized ratio (INR), if using warfarin therapy
• Nonsteroidal anti-inflammatory drug (NSAID); also used as an analgesic and as an antipyretic (see Chapter 18).
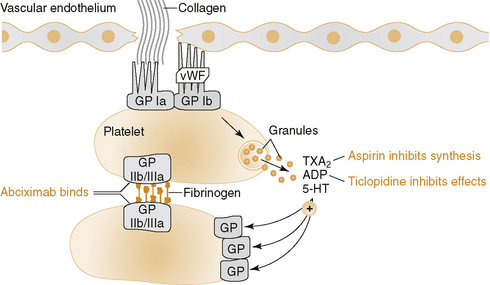
a. Aspirin inhibits synthesis of thromboxane A2 (TXA2), a potent platelet aggregator and vasoconstrictor, by irreversible acetylation of cyclooxygenase (COX-1) in platelets.
TABLE 16-1 Clinical Uses of Anticoagulant, Antiplatelet, and Fibrinolytic Drugs
| Clinical Use | Primary Drug* | Secondary Drug* |
|---|---|---|
| Acute thrombotic stroke | Fibrinolytic drug | — |
| Artificial heart valve | Warfarin or aspirin | Dipyridamole |
| Atrial fibrillation | Heparin, warfarin, or LMWH | Aspirin |
| Deep vein thrombosis | ||
| Treatment | Heparin, warfarin, or LMWH | — |
| Surgical prophylaxis | LMWH | Heparin |
| Heparin-induced thrombocytopenia (HIT) | “-rudins” | Argatroban |
| Myocardial infarction | ||
| Treatment | Fibrinolytic drug, heparin, aspirin, or abciximab | — |
| Prevention | Aspirin | Clopidogrel |
| Percutaneous transluminal coronary angioplasty | Abciximab, heparin, aspirin, or clopidogrel | — |
| Pulmonary embolism | Fibrinolytic drug, heparin, warfarin, or LMWH | — |
| Stroke | Aspirin, clopidogrel, or warfarin | — |
| Transient ischemic attacks | Aspirin | Warfarin |
| Unstable angina | Aspirin, abciximab, heparin, or LMWH | — |
LMWH, low-molecular-weight heparin.
* If aspirin is contraindicated or not tolerated, ticlopidine may be used. If warfarin is contraindicated or not tolerated, another oral anticoagulant may be used.
(3) COX-2 is present at the sites of acute and chronic inflammation as well as in endothelial cells.
b. TXA2 increases the PIP2 (phosphatidylinositol biphosphate pathway) in platelets, causing aggregation (reduced by aspirin).
c. Low-dose aspirin therapy (1 baby [81 mg] or 1 adult [325 mg] tablet per day) primarily inhibits COX-1 to prevent synthesis of TXA2 without decreasing the synthesis of prostacyclin (PGI2) in endothelial cells, which inhibits platelet aggregation.
d. Higher doses of aspirin (2 or more adult tablets per day) inhibit synthesis of both TXA2 and PGI2.
(1) Interferes with adenosine diphosphate (ADP)-induced binding of fibrinogen to platelet membrane at specific receptor sites (GpIIb/IIIa)
(2) Inhibits platelet aggregation and platelet-platelet interactions that produce platelet thrombi (e.g., coronary artery thrombosis)
(1) Prevents thrombotic stroke (initial or recurrent) in patients who are intolerant or unresponsive to aspirin
(2) Prevents thrombus formation in patients with cardiac stents and in treatment of acute coronary syndromes (in combination with aspirin)
(1) Severe bone marrow toxicity, including agranulocytosis (neutropenia), aplastic anemia (pancytopenia; rare); occurs mostly with ticlopidine
(3) Clopidogrel is associated with a lower incidence of adverse cutaneous, GI, and hematologic reactions than ticlopidine.
(4) Clopidogrel causes some drug-drug interactions (inhibits cytochrome P-450 enzymes); inhibits metabolism of:
(2) Potentiates action of PGI2, which is coupled to a cyclic adenosine monophosphate (cAMP)-generating system in platelets and vasculature, causing decreased platelet aggregation and vasodilation, respectively
(1) Abciximab prevents binding of fibrinogen, von Willebrand factor, and other adhesive molecules to the glycoprotein receptor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree