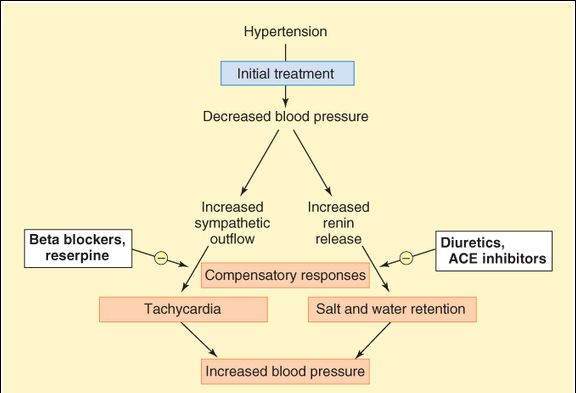
Less than 20% of cases of hypertension are due to (“secondary” to) factors that can be clearly defined and corrected. This type of hypertension is associated with pheochromocytoma, coarctation of the aorta, renal vascular disease, adrenal cortical tumors, and a few other rare conditions. Most cases of hypertension are idiopathic, also called “primary” or “essential” hypertension. The strategies for treating idiopathic high blood pressure are based on the determinants of arterial pressure (see Figure 6-4). These strategies include reductions of blood volume, sympathetic tone, vascular smooth muscle tone, and angiotensin effects. Unfortunately, the baroreceptor reflex and the renin response in primary hypertension are reset to maintain the higher blood pressure. As a result, they respond to lower blood pressure with compensatory homeostatic responses, which may be significant (Table 11-1). As indicated in Figure 11-1, some compensatory responses can be counteracted with  blockers (for tachycardia) and diuretics or angiotensin antagonists (for salt and water retention).
blockers (for tachycardia) and diuretics or angiotensin antagonists (for salt and water retention).
TABLE 11-1 Compensatory responses to antihypertensive drugs and some of their adverse effects.
Class and Drug Compensatory Responses Adverse Effects Diuretics Hydrochlorothiazide Minimal Hypokalemia, slight to moderate hyperlipidemia, hyperuricemia, hyperglycemia, lassitude, weakness, impotence Furosemide Minimal Hypokalemia, hypovolemia, ototoxicity Sympathoplegics Clonidine Salt and water retention Dry mouth, severe rebound hypertension if drug is suddenly stopped Methyldopa Salt and water retention Sedation, positive Coombs, test, hemolytic anemia (rare) Ganglion blockers (obsolete) Salt and water retention Severe orthostatic hypotension, constipation, blurred vision, sexual dysfunction Reserpine (low dose) Minimal Diarrhea, nasal stuffiness, sedation, depression Alpha1-selective blockers
Salt and water retention, slight tachycardia Orthostatic hypotension (usually limited to first few doses) Beta blockers Minimal Sleep disturbances, sedation, impotence, cardiac disturbances, asthma Vasodilators Hydralazine Salt and water retention, tachycardia Reversible lupus-like syndrome (but lacking renal effects) Minoxidil Marked salt and water retention, marked tachycardia Hirsutism, pericardial effusion Nifedipine, other calcium channel blockers Minor salt and water retention Constipation, cardiac disturbances, flushing Nitroprusside Salt and water retention Cyanide, thiocyanate toxicity Angiotensin antagonists ACE inhibitors Minimal Cough, renal damage in the fetus and in preexisting renal disease Angiotensin receptor blockers Minimal Renal damage in the fetus and in preexisting renal disease
FIGURE 11-1
Compensatory responses (red boxes) to decreased blood pressure when treating hypertension. The initial treatment that causes the compensatory responses might be a vasodilator. Arrows with minus signs indicate drugs used (white boxes) to minimize the compensatory responses. ACE, angiotensin-converting enzyme.
High-Yield Terms to Learn
Baroreceptor reflex Primary autonomic mechanism for blood pressure homeostasis; involves sensory input from carotid sinus and aorta to the vasomotor center and output via the parasympathetic and sympathetic motor nerves Catecholamine reuptake pump (norepinephrine transporter [NET]) Nerve terminal transporter responsible for recycling norepinephrine after release into the synapse Catecholamine vesicle pump Storage vesicle transporter that pumps amine from cytoplasm into vesicle End-organ damage Vascular damage in heart, kidney, retina, or brain Essential hypertension Hypertension of unknown etiology; also called primary hypertension False transmitter Substance, for example, octopamine, stored in vesicles and released into synaptic cleft but lacking the effect of the true transmitter, for example, norepinephrine Orthostatic hypotension Hypotension on assuming upright posture; postural hypotension Postganglionic neuron blocker Drug that blocks transmission by an action in the terminals of the postganglionic nerves Rebound hypertension Elevated blood pressure (usually above pretreatment levels) resulting from loss of antihypertensive drug effect Reflex tachycardia Tachycardia resulting from lowering of blood pressure; mediated by the baroreceptor reflex Stepped care Progressive addition of drugs to a regimen, starting with one (usually a diuretic) and adding in stepwise fashion a sympatholytic, an ACE inhibitor, and (sometimes) a vasodilator Sympatholytic, sympathoplegic Drug that reduces effects of the sympathetic nervous system
Diuretics
Diuretics are covered in greater detail in Chapter 15 but are mentioned here because of their importance in hypertension. These drugs lower blood pressure by reduction of blood volume and probably also by a direct vascular effect that is not fully understood. The diuretics most important for treating hypertension are the thiazides (eg, hydrochlorothiazide) and the loop diuretics (eg, furosemide). Thiazides may be adequate in mild hypertension, but the loop agents are often used in moderate, severe, and malignant hypertension. Compensatory responses to blood pressure lowering by diuretics are minimal (Table 11-1). When thiazides are given, the maximum antihypertensive effect is often achieved with doses lower than those required for the maximum diuretic effect.
Skill Keeper 1: Development of New Antihypertensive Drugs
(See Chapter 5)
A new drug is under development for the treatment of hypertension. What types of data will the producer of this drug have to provide to carry out clinical trials? What data will be needed to market the drug? The Skill Keeper Answer appears at the end of the chapter.
Sympathoplegics
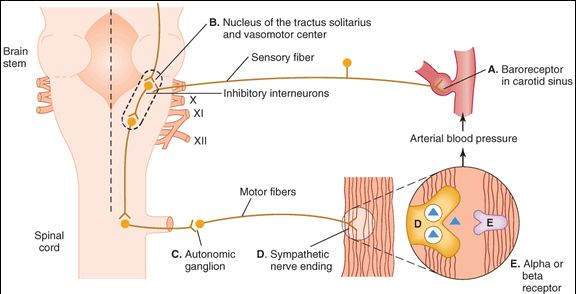
Sympathoplegic drugs interfere with sympathetic (SANS) control of cardiovascular function. The result is a reduction of one or more of the following: venous tone, heart rate, contractile force of the heart, cardiac output, and total peripheral resistance (see Figure 6-4). Compensatory responses and adverse effects are marked for some of these agents (Table 11-1). Sympathoplegics are subdivided by anatomic site of action (Figure 11-2).
FIGURE 11-2
Baroreceptor reflex arc and sites of action of sympathoplegic drugs. The letters (A-E) indicate potential sites of action of subgroups of sympathoplegics. No clinically useful drugs act at the baroreceptor (site A), but drugs are available for each of the other sites.
Baroreceptor-Sensitizing Agents
A few natural products, such as veratrum alkaloids, appear to increase sensitivity of baroreceptor sensory nerves and reduce SANS outflow while increasing vagal tone to the heart. These agents are toxic and no clinically available drugs act at this site.
Central Nervous System-Active Agents
Alpha2-selective agonists (eg, clonidine, methyldopa ) cause a decrease in sympathetic outflow by activation of  2 receptors in the CNS. These drugs readily enter the CNS when given orally. Methyldopa is a prodrug; it is converted to methylnorepinephrine in the brain. Clonidine and methyldopa both reduce blood pressure by reducing cardiac output, vascular resistance, or both. The major compensatory response is salt retention. Sudden discontinuation of clonidine causes rebound hypertension, which may be severe. This rebound increase in blood pressure can be controlled by reinstitution of clonidine therapy or administration of
2 receptors in the CNS. These drugs readily enter the CNS when given orally. Methyldopa is a prodrug; it is converted to methylnorepinephrine in the brain. Clonidine and methyldopa both reduce blood pressure by reducing cardiac output, vascular resistance, or both. The major compensatory response is salt retention. Sudden discontinuation of clonidine causes rebound hypertension, which may be severe. This rebound increase in blood pressure can be controlled by reinstitution of clonidine therapy or administration of  blockers such as phentolamine. Methyldopa occasionally causes hematologic immunotoxicity, detected initially by test tube agglutination of red blood cells (positive Coombs’ test) and in some patients progressing to hemolytic anemia. Both drugs may cause sedation—methyldopa more so at therapeutic dosage.
blockers such as phentolamine. Methyldopa occasionally causes hematologic immunotoxicity, detected initially by test tube agglutination of red blood cells (positive Coombs’ test) and in some patients progressing to hemolytic anemia. Both drugs may cause sedation—methyldopa more so at therapeutic dosage.
Ganglion-Blocking Drugs
Nicotinic blockers that act in the ganglia are very efficacious but because their adverse effects (Table 11-1) are severe, they are now considered obsolete. Hexamethonium and trimethaphan are extremely powerful blood pressure-lowering drugs. The major compensatory response is salt retention. Toxicities reflect parasympathetic blockade (blurred vision, constipation, urinary hesitancy, sexual dysfunction) and sympathetic blockade (sexual dysfunction, orthostatic hypotension).
Postganglionic Sympathetic Nerve Terminal Blockers
Drugs that deplete the adrenergic nerve terminal of its norepinephrine stores (eg, reserpine ) or that deplete and block release of the stores (eg, guanethidine) can lower blood pressure. The major compensatory response is salt and water retention. In high dosages, both reserpine and guanethidine are very efficacious but produce severe adverse effects. Reserpine is still occasionally used in low doses as an adjunct to other agents. Guanethidine has been withdrawn from the US market. Reserpine readily enters the CNS; guanethidine does not. Both have long durations of action (days to weeks). The most serious toxicity of reserpine is behavioral depression, which may require discontinuation of the drug. The major toxicities of guanethidine are orthostatic hypotension and sexual dysfunction. Guanethidine requires the norepinephrine reuptake pump (uptake 1, NET; see Figure 6-2) to reach its intracellular site of action. Therefore, drugs that inhibit this pump (eg, cocaine, tricyclic antidepressants) interfered with the action of guanethidine.
Monoamine oxidase (MAO) inhibitors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree