A. Diabetes mellitus is classified by the underlying disease etiology (type 1 vs. type 2) rather than by age-of-onset (juvenile-onset vs. adult-onset diabetes) or treatment modality (insulin-dependent vs. non–insulin-dependent diabetes).
1. The insulin deficiency in type 1 diabetes is the result of autoimmune-mediated destruction of pancreatic beta cells.
2. Onset of type 1 diabetes is at a younger age than onset of type 2 diabetes, and sensitivity to insulin is normal. In contrast, the peripheral insulin resistance of type 2 diabetes is often coupled with a failure to secrete insulin because of pancreatic β cell dysfunction.
3. Oral hypoglycemic drugs are alternatives to exogenous administration of insulin to patients with type 2 diabetes.
B. Low plasma concentrations of insulin, although inadequate to prevent hyperglycemia, may block lipolysis. This differential effect of insulin explains why hyperglycemia can exist without the presence of ketone bodies. Ketosis can be reliably prevented by continuously providing all diabetic patients with glucose and insulin. Prevention is uniquely important in the perioperative period when nutritional intake is altered.
C. The goals of therapy for patients with diabetes mellitus include preventing the adverse consequences of hypoglycemia and hyperglycemia, avoiding weight gain, and reducing microvascular and macrovascular complications.
1. Symptoms often resolve when blood glucose levels are less than 200 mg/dL.
2. Long-term metabolic control of diabetes is best monitored by measurement of glycosylated hemoglobin (HbA1c), which reflects glucose control over the previous 2 to 3 months. In general, HbA1c values less than 6.0% to 7.0% are associated with fewer microvascular complications.
II. Insulin. Patients with type 1 diabetes mellitus do not produce insulin and require insulin therapy to survive. Insulin is prescribed for patients with type 2 diabetes mellitus if treatment with oral glucose regulators fails. Insulin therapy mirrors the normal pattern of insulin secretion (pulsatile secretion that occurs under basal conditions and in response to meals) with basal supplementation and by short-acting insulin taken before food absorption. Insulin receptors become fully saturated with low concentrations of insulin (continuous infusion of insulin, 1 to 2 units per hour, has the same or even greater pharmacologic effect than a single larger intravenous [IV] dose that is cleared rapidly from the circulation).
A. Pharmacokinetics
1. Insulin is metabolized in the kidneys and liver (~50% of the insulin that reaches the liver through its portal vein is metabolized in a single passage). Nevertheless, renal dysfunction alters the disappearance rate of circulating insulin to a greater extent than does hepatic disease (unexpected prolonged effects of insulin are found in patients with renal disease, reflecting impairment of both its metabolism and excretion by the kidneys).
2. Despite rapid clearance from plasma after IV injection of insulin, the pharmacologic effect lasts for 30 to 60 minutes because insulin is tightly bound to tissue receptors. Insulin administered subcutaneously releases slowly into the circulation to produce a sustained biologic effect.
3. Insulin is secreted into the portal venous system in the basal state at a rate of approximately 1 unit per hour. After food intake, the rate of insulin secretion increases 5- to 10-fold. The total daily secretion of insulin is approximately 40 units.
4. The sympathetic and parasympathetic nervous systems innervate the insulin-producing islet cells to influence the basal rate of hormone secretion as well as the response to stress (α-adrenergic stimulation decreases and β-adrenergic or parasympathetic nervous system stimulation increases the basal secretion of insulin).
5. The insulin response to glucose is greater after oral ingestion than after IV infusion because glucose-dependent insulinotropic polypeptide is released after oral ingestion of glucose and the pancreatic β cell response is augmented.
6. To gain adequate glycemic control in type 1 diabetes, at least two daily subcutaneous injections of intermediate- or long-acting insulin combined with rapid-acting insulin are nearly always required.
B. Insulin Preparations and Delivery (Table 38-2). Human insulin manufactured using recombinant DNA technology has replaced insulin extracted from beef and pork pancreas. Allergy or immunoresistance to animal insulins is no longer a serious problem.
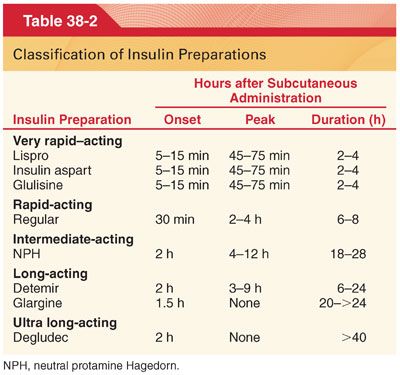
1. The basic principle of replacement is to provide a slow, long-acting, continuous supply of insulin (neutral protamine Hagedorn [NPH] insulin, insulin glargine, insulin detemir, or insulin degludec) that mimics the nocturnal and interprandial basal secretion of normal pancreatic β cells.
2. Commercially prepared insulin is bioassayed, and its physiologic activity (potency), based on the ability to decrease blood glucose concentration, is expressed in units. The potency of insulin is 22 to 26 U/mg.
a. Insulin U-100 (100 U/mL) is the most commonly used commercial preparation. The total daily exogenous dose of insulin for treatment of type 1 diabetes mellitus is usually in the range of 0.5 to 1 U/kg/day.
b. This insulin requirement may be increased dramatically by stress associated with sepsis or trauma.
3. Continuous subcutaneous insulin infusion (CSII) through an external pump delivers basal insulin (0.01 to 0.015 U/kg/hour) and bolus doses before meals. With this system, nocturnal versus daytime basal requirements can be accommodated, infusions can be altered during exercise, and doses can be calculated via algorithms of previous glucose values and insulin delivery. Short-acting insulin (regular) and ultra rapid-acting insulins (lispro, aspart, and glulisine) are the only preparations used for CSII delivery pumps.
C. Lispro is a short-acting insulin analogue that more closely parallels physiologic insulin secretion and needs (injected subcutaneously begins to act within 15 minutes, the peak effect is reached in 45 to 75 minutes, and the duration of action is only 2 to 4 hours).
1. Lispro injected just before eating provides a postprandial plasma insulin concentration profile similar to that of normal insulin secretion.
2. An important benefit of lispro is a decrease in postprandial hyperglycemia and less risk of hypoglycemia, which may follow injection of regular insulin.
D. Insulin aspart and glulisine are synthetic rapid-acting analogues with a profile of action and therapeutic benefits similar to those of lispro.
E. Regular insulin (crystalline zinc insulin) is a fast-acting preparation and is the only form of insulin that can be administered IV as well as subcutaneously.
1. Administration of regular insulin is preferred for treating the abrupt onset of hyperglycemia or the appearance of ketoacidosis.
2. In the perioperative period, regular insulin is administered as a single IV injection (1 to 5 units) or as a continuous infusion (0.5 to 2.0 units per hour) to treat metabolic derangements associated with diabetes mellitus.
F. Neutral protamine Hagedorn is an intermediate-acting preparation whose absorption from its subcutaneous injection site is delayed because the insulin is conjugated with protamine.
G. Side Effects
1. Hypoglycemia is the most serious side effect of insulin therapy (patients are vulnerable to hypoglycemia if they receive exogenous insulin in the absence of carbohydrate intake, as during a perioperative period, especially before surgery).
a. The first symptoms of hypoglycemia are the compensatory effects of increased epinephrine secretion: diaphoresis, tachycardia, and hypertension. Symptoms of hypoglycemia involving the central nervous system (CNS) include mental confusion progressing to seizures and coma.
b. The diagnosis of hypoglycemia during general anesthesia is difficult because anesthetic drugs mask the classic signs of sympathetic nervous system stimulation (signs of sympathetic nervous system stimulation are likely to be confused with responses evoked by painful surgical stimulation in an anesthetized patient).
c. Severe hypoglycemia is treated with 50 to 100 mL of 50% glucose solution administered IV (alternatively, glucagon, 0.5 to 1.0 mg IV).
2. Allergic Reactions
a. Use of human insulin preparations has eliminated the problem of systemic allergic reactions that could result from administration of animal-derived insulins.
b. Local allergic reactions are characterized by an erythematous indurated area that develops at the site of insulin injection (cause is likely to be noninsulin materials in the insulin preparation).
c. Chronic exposure to low doses of protamine in NPH insulin may stimulate the production of antibodies against protamine. Patients remain asymptomatic until a large dose of protamine is administered IV to antagonize the anticoagulant effects of heparin.
3. Lipodystrophy results when fat atrophies at the site of subcutaneous injection of insulin.
4. Insulin Resistance
a. Patients requiring greater than 100 units of exogenous insulin daily are in a state of insulin resistance.
b. Acute insulin resistance is associated with trauma from infection or surgery.
5. Drug Interactions
a. There are hormones administered as drugs that counter the hypoglycemic effect of insulin (adrenocorticotrophic hormone, estrogens, glucagon).
b. Epinephrine inhibits the secretion of insulin and stimulates glycogenolysis.
c. Certain antibiotics (tetracycline or chloramphenicol), salicylates, and phenylbutazone increase the duration of action of insulin and may have a direct hypoglycemic effect.
d. The hypoglycemic effect of insulin may be potentiated by monoamine oxidase inhibitors.
III. Oral Glucose Regulators. Oral drugs with different mechanisms of action are available for controlling plasma glucose concentrations in patients with type 2 diabetes mellitus (Table 38-3). None of these drugs will adequately control hyperglycemia indefinitely (use of combinations of oral drugs from the onset of treatment may be indicated). The effect on HbA1c is similar for these drugs.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


