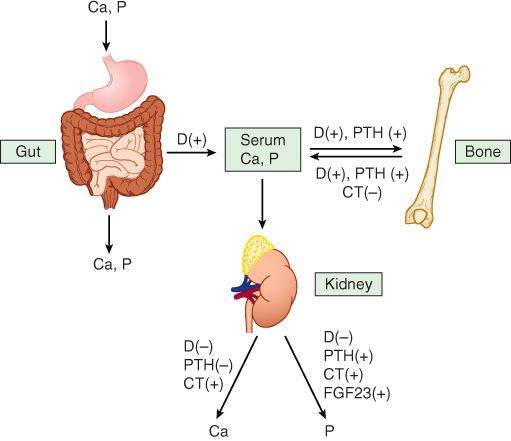
FIGURE 42-1
Effects of active metabolites of vitamin D (D), parathyroid hormone (PTH), calcitonin (CT), and fibroblast growth factor 23 (FGF23) on calcium and phosphorus homeostasis. Active metabolites of vitamin D increase absorption of calcium from both gut and bone, whereas PTH increases reabsorption from bone. Vitamin D metabolites and PTH both reduce urinary excretion ofcalcium. In animals with vitamin D deficiency, active metabolites of vitamin D produce a net increase in bone mineralization by increasing the availability of serum calcium and phosphate.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 41-1.)
High-Yield Terms to Learn
Hyperparathyroidism A condition of PTH excess characterized by hypercalcemia, bone pain, cognitive abnormalities, and renal stones. Primary disease results from parathyroid gland dysfunction. Secondary disease most commonly results from chronic kidney disease Osteoblast Bone cell that promotes bone formation Osteoclast Bone cell that promotes bone resorption Osteomalacia A condition of abnormal mineralization of adult bone secondary to nutritional deficiency of vitamin D or inherited defects in the formation or action of active vitamin D metabolites Osteoporosis Abnormal loss of bone with increased risk of fractures, spinal deformities, and loss of stature; remaining bone is histologically normal Paget’s disease A bone disorder, of unknown origin, characterized by excessive bone destruction and disorganized repair. Complications include skeletal deformity, musculoskeletal pain, kidney stones, and organ dysfunction secondary to pressure from bony overgrowth Rickets The same as osteomalacia, but it occurs in the growing skeleton RANK ligand An osteoblast-derived growth factor that stimulates osteoclast activity and osteoclast precursor differentiation
Hormonal Regulators of Bone Mineral Homeostasis
Parathyroid Hormone
Parathyroid hormone (PTH), an 84-amino-acid peptide, acts on membrane G-protein-coupled receptors to increase cyclic adenosine monophosphate (cAMP) in bone and renal tubular cells. In the kidney, PTH inhibits calcium excretion, promotes phosphate excretion, and stimulates the production of active vitamin D metabolites (Figure 42-1, Table 42-1). In bone, PTH promotes bone turnover by increasing the activity of both osteoblasts and osteoclasts (Figure 42-2B). Osteoclast activation is not a direct effect and instead results from PTH stimulation of osteoblast formation of RANK ligand (RANKL), a member of the tumor necrosis factor (TNF) cytokine family that stimulates the activity of mature osteoclasts and the differentiation of osteoclast precursors.
TABLE 42-1 Actions of PTH and active vitamin D metabolites on intestine, kidney, and bone.
Organ PTH Active Vitamin D Metabolites Intestine Indirectly increases calcium and phosphate absorption by increasing vitamin D metabolites Increased calcium and phosphate absorption Kidney Decreased calcium excretion, increased phosphate excretion Increased resorption of calcium and phosphate but usually net increase in urinary calcium due to effects in GI tract and bone Bone Calcium and phosphate resorption increased by continuous high concentrations. Low intermittent doses increase bone formation Direct effect is increased calcium and phosphate resorption; indirect effect is promoting mineralization by increasing the availability of calcium and phosphate Net effect on serum levels Serum calcium increased, serum phosphate decreased Serum calcium and phosphate both increased
Reproduced and modified, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009.
FIGURE 42-2
Hormonal interactions controlling bone mineral homeostasis. (A) The 1,25-dihydroxyvitamin D that is produced by the kidney under control of parathyroid hormone (PTH) and fibroblast growth hormone 23 (FGF23) stimulates intestinal uptake of calcium and phosphate, and, in those with vitamin D deficiency, promotes bone formation. Calcitonin inhibits resorption from bone, whereas PTH stimulates bone resorption. Extracellular calcium and 1,25-dihydroxyvitamin D inhibit PTH production. (B) Both PTH and 1,25-dihydroxyvitamin D regulate bone formation and resorption. This is accomplished by their activation of precursor differentiation and by stimulation of osteoblast production of signaling factors, including RANK ligand (RANKL), macrophage colony-stimulating factor (MCSF), and osteoprotegerin.
(Reproduced and modified, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 42-2.)
At the continuous high concentrations seen in hyperparathyroidism, the net effect of elevated PTH is increased bone resorption, hypercalcemia, and hyperphosphatemia. However, low intermittent doses of PTH produce a net increase in bone formation; this is the basis of the use of teriparatide , a recombinant truncated form of PTH, for parenteral treatment of osteoporosis.
The synthesis and secretion of PTH is primarily regulated by the serum concentration of free ionized calcium; a drop in free ionized calcium stimulates PTH release. Active metabolites of vitamin D play a secondary role in regulating PTH secretion by inhibiting PTH synthesis (Figure 42-2A).
Vitamin D
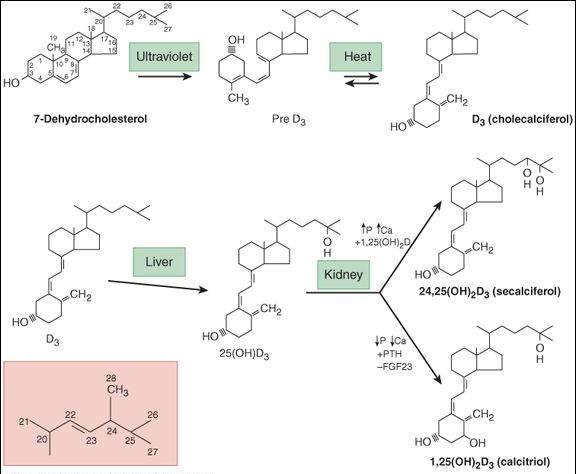
Vitamin D, a fat-soluble vitamin (Figure 42-3), can be synthesized in the skin from 7-dehydrocholesterol under the influence of ultraviolet light or absorbed from the diet in the natural form (vitamin D3 , cholecalciferol ) or the plant form (vitamin D2 , ergocalciferol ). Active metabolites are formed in the liver (25-hydroxyvitamin D or calcifediol) and kidney (1,25-dihydroxyvitamin D or calcitriol plus other metabolites). Renal synthesis of active vitamin D metabolites is stimulated by PTH and by fibroblast growth factor 23 (FGF23), a factor produced by osteoblasts and osteoclasts. Renal synthesis of 1,25-dihydroxyvitamin D2 is inhibited by phosphate and vitamin D metabolites (Figure 41-2). The action of vitamin D metabolites is mediated by activation of 1 or possibly a family of nuclear receptors that regulate gene expression.
FIGURE 42-3
Conversion of 7-dehydroxycholsterol to vitamin D3 and metabolism of vitamin D 3 to 1,25-dihydroxyvitamin D3 (1,25(OH)2D3) and to 24,25-dihydroxyvitamin D3 (24,25(OH)2D3). The inset shows the side chain for ergosterol. Ergosterol undergoes similar transformation to vitamin D2 (ergocalciferol), which, in turn is metabolized to 1,25-dihydroxyvitamin D2 and 24,25-dihydroxyvitamin D2. In humans, corresponding D2 and D3 have equivalent effects and potency. They are therefore referred to in the text without a subscript.
(Reproduced, with permission, from Katzung BG, editor: Basic & Clinical Pharmacology, 11th ed. McGraw-Hill, 2009: Fig. 42-3.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree