31
Drug Therapy of Mineral Ion Homeostasis and Bone Turnover Disorders
This chapter will be most useful after having a basic understanding of the material in Chapter 44, Agents Affecting Mineral Ion Homeostasis and Bone Turnover in Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition. In addition to the material presented here, the 12th Edition contains:
• A detailed discussion of the physiology of mineral ion homeostasis
• A description of the hormonal regulation of calcium and phosphorous homeostasis
• A discussion of bone physiology
• A detailed discussion of the pharmacological treatment of disorders of mineral ion homeostasis and bone metabolism, including the therapeutic uses of vitamin D, calcitonin, bisphosphonates, parathyroid hormone (PTH), and calcium sensor mimetics
• A description of an integrated approach to the prevention and treatment of osteoporosis
LEARNING OBJECTIVES
 Understand calcium and phosphorous homeostasis.
Understand calcium and phosphorous homeostasis.
 Describe the roles of PTH, calcitonin, and vitamin D in calcium homeostasis.
Describe the roles of PTH, calcitonin, and vitamin D in calcium homeostasis.
 Understand the concept of bone resorption and bone formation.
Understand the concept of bone resorption and bone formation.
 Describe the mechanism of action and untoward effects of bisphosphonates.
Describe the mechanism of action and untoward effects of bisphosphonates.
 Describe the role of bisphosphonates in the prevention and treatment of osteoporosis.
Describe the role of bisphosphonates in the prevention and treatment of osteoporosis.
 Describe the pharmacological management of hypocalcemia and hypercalcemia.
Describe the pharmacological management of hypocalcemia and hypercalcemia.
DRUGS INCLUDED IN THIS CHAPTER
1α-hydroxycholecalciferol (1-OHD, alphacalcidol, ONE-ALPHA)
22-Oxacalcitrol (1,25-dihydroxy-22-oxavitamin D3, OCT, maxacalcitol, OXAROL)
Alendronate (FOSAMAX)
Calcipotriene (DOVONEX, others)
Calcitonin (CALCIMAR, MIACALCIN)
Calcitriol (1,25-dihydroxycholecalciferol; CALCIJEX, ROCALTROL)
Calcium salts
Cinacalcet (SENSIPAR)
Denosumab (investigational)
Dihydrotachysterol (DHT, ROXANE)
Doxercalciferol (1α-hydroxyvitamin D2, HECTOROL)
Ergocalciferol (calciferol, DRISDOL)
Etidronate sodium (DIDRONEL)
Ibandronate (BONIVA)
Lanthanum carbonate (FOSRENOL)
Pamidronate (AREDIA)
Paricalcitol (1,25-dihydroxy-19-norvitamin D2, ZEMPLAR)
Plicamycin (MITHRACIN)
Risedronate (ACTONEL)
Sevelamer hydrochloride (RENAGEL)
Teriparatide (FORTEO)
Tiludronate (SKELID)
Zoledronate (ZOMETA)
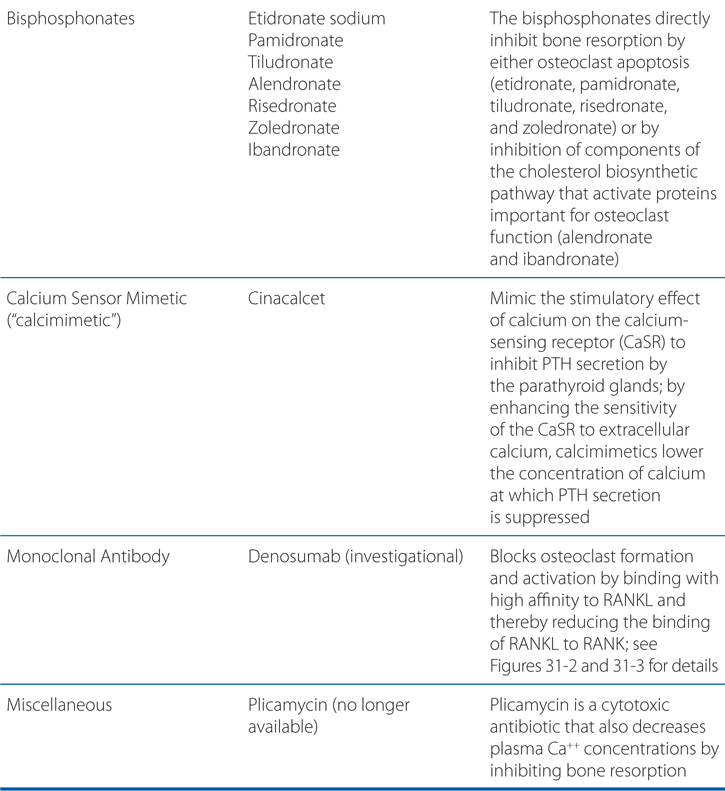
MECHANISMS OF ACTION OF DRUGS USED IN MINERAL HOMEOSTASIS AND BONE TURNOVER DISORDERS
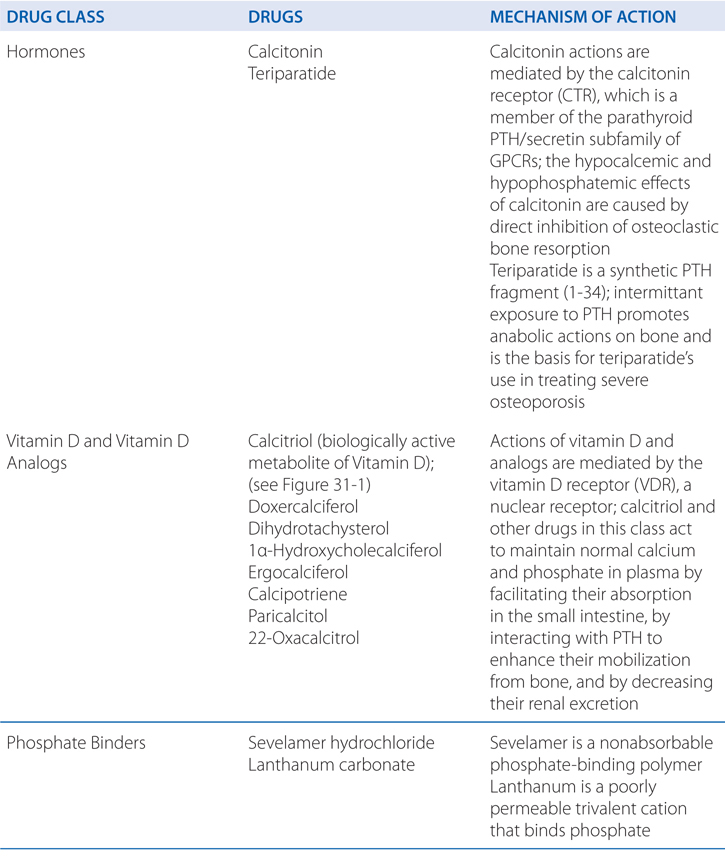
FIGURE 31-1 Regulation of 1α-hydroxylase activity. Changes in the plasma levels of PTH, Ca2+, and phosphate modulate the hydroxylation of 25-OH vitamin D to the active form, 1,25-dihydroxyvitamin D. 25-OHD, 25-hydroxycholecalciferol; 1,25-(OH)2-D, calcitriol; PTH, parathyroid hormone.
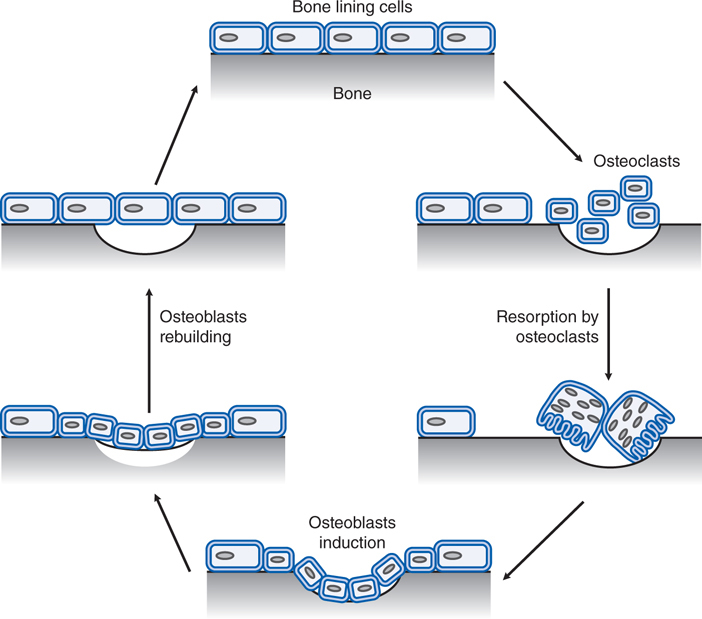
FIGURE 31-2 The bone remodeling cycle. Osteoclast precursors fuse and are activated to resorb a lacuna in a previously quiescent surface. These cells are replaced by osteoblasts that deposit new bone to restore the integrity of the tissue. (Adapted with permission from Skerry TM, Gowen M. Bone cells and bone in remodelling in rheumatoid arthritis. In: Henderson B, Edwards JCW, Pettipher ER, eds. Mechanisms and Models in Rheumatoid Arthritis. London: Academic Press; 1995, pp 205-220.)
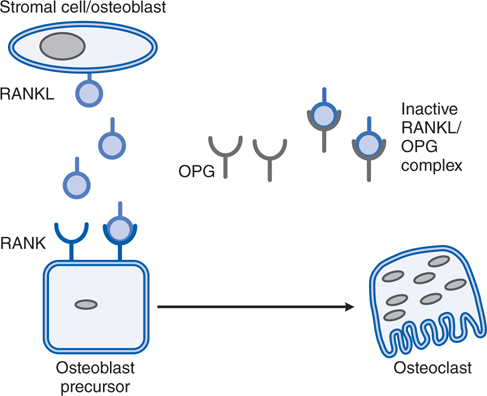
FIGURE 31-3 Receptor for activating NF-κB ligand (RANKL) and osteoclast formation. RANKL, acting on RANK, promotes osteoclast formation and subsequent resorption of bone matrix. Osteoprotegerin (OPG) binds to RANKL, reducing its binding to RANK and thereby inhibiting osteoclast differentiation.
THERAPEUTIC USES OF VITAMIN D
• Prophylaxis and cure of nutritional rickets
• Treatment of metabolic rickets and osteomalacia, particularly in the setting of chronic renal failure
• Treatment of hypoparathyroidism
• Prevention and treatment of osteoporosis
A 56-year-old man with a diagnosis of lung cancer is hospitalized because of lethargy, weakness, and polyuria. His serum calcium is 13 mg/dL.
a. Why is his serum calcium elevated?
Newly diagnosed hypercalcemia in hospitalized patients is most often caused by systemic malignancy, either with or without bone metastasis. PTH-related protein (PTHrP) is a primitive, highly conserved protein that may be abnormally expressed in malignant tissue, particularly in squamous cell and other epithelial cancers. Other tumors release cytokines or prostaglandins that stimulate bone resorption.
b. How does PTH cause hypercalcemia?
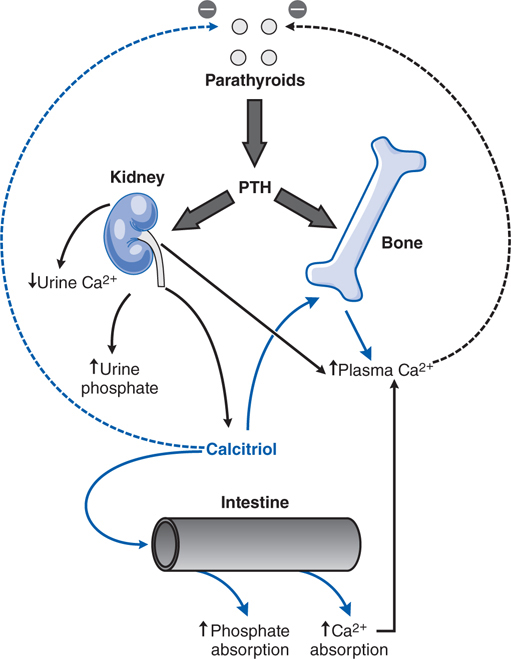
The primary function of PTH is to maintain a constant concentration of calcium and phosphorous in the extracellular fluid. The principal processes regulated are renal calcium and phosphorous absorption and mobilization of bone calcium (Figure 31-4). The actions of PTH on target tissues are mediated by at least 2 receptors: the PTH1 receptor which binds both PTH and PTHrP; and the PTH2 receptor found in vascular tissue, brain, pancreas, and placenta which binds only PTH.
FIGURE 31-4 Calcium homeostasis and its regulation by parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D. PTH has stimulatory effects on bone and kidney, including the stimulation of 1α-hydroxylase activity in kidney mitochondria leading to the increased production of 1,25-dihydroxyvitamin D (calcitriol) from 25-hydroxycholecalciferol, the monohydroxylated vitamin D metabolite. Calcitriol is the biologically active metabolite of vitamin D.
c. What are the treatment options for this patient?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree