II. Carbonic Anhydrase Inhibitors
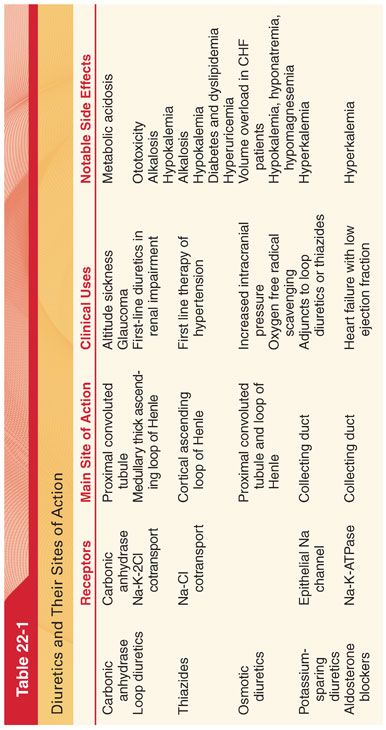
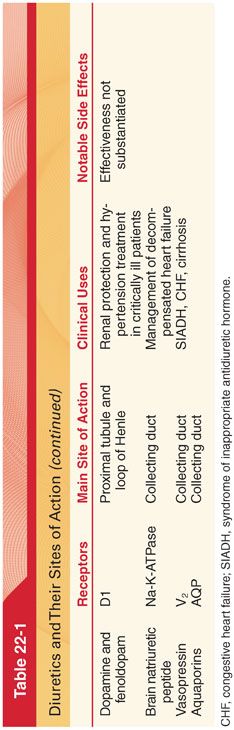
A. Acetazolamide is the prototype of a class of sulfonamide drugs that bind avidly to the enzyme carbonic anhydrase, producing noncompetitive inhibition of enzyme activity, principally in the proximal renal tubules as well as the collecting ducts (Table 22-1) (see Fig. 22-1).
1. Pharmacokinetics and Pharmacodynamics. After oral administration, acetazolamide is excreted unchanged by the kidneys (dose should be adjusted in patients with renal failure and the elderly). Acetazolamide completely blocks membrane-bound and cytoplasmic carbonic anhydrase in the proximal tubule and to a lesser extent in the collecting ducts, preventing Na+ and HCO3– absorption. This increased excretion of HCO3– results in an alkaline urine and metabolic acidosis.
2. Clinical Uses
a. In addition to its diuretic properties, acetazolamide is administered to decrease intraocular pressure in the treatment of glaucoma.
b. Formation of cerebrospinal fluid is inhibited by acetazolamide and it has been used in the treatment of idiopathic intracranial hypertension.
c. Acetazolamide may be beneficial in the management of familial periodic paralysis because the drug-induced metabolic acidosis increases the local concentration of potassium in skeletal muscles.
d. Acetazolamide, by producing metabolic acidosis, may stimulate the respiratory drive in patients who are hypoventilating in a compensatory response to respiratory alkalosis, as occurs with altitude sickness.
3. Side Effects
a. There is a high incidence of systemic side effects associated with the use of acetazolamide (fatigue, decreased appetite, depression, paresthesias), which could be secondary to the development of acidosis.
b. Acetazolamide dose should be reduced in patients with chronic renal insufficiency and avoided in patients with severe chronic renal insufficiency because of the increased risk of metabolic acidosis.
III. Loop diuretics are first-line therapy in patients with fluid retention resulting from heart failure.
A. Pharmacokinetics and Pharmacodynamics
1. Furosemide is effective when administered orally (absorption varies between patients from 10% to 100%, with an average bioavailability of 50%) or intravenously. Furosemide has a rapid onset, producing diuresis within 5 to 10 minutes of administration, with a peak effect at 30 minutes and duration of action of 2 to 6 hours. In patients with normal renal function, 40 mg of intravenous (IV) furosemide will produce maximal natriuresis.
2. Bumetanide and Torasemide
a. Bumetanide is 40 times more potent than furosemide except in its effect on potassium excretion.
b. Torasemide is twice as potent as furosemide and has a longer duration of action allowing for a once a day dosing regimen.
B. Clinical Uses
1. Loop diuretics are the first line of treatment of hypertension in patients with renal insufficiency. The antihypertensive effect of loop diuretics is due to their ability to decrease intravascular fluid volume and eliminate salt. Compared to furosemide, the long-acting drug azosemide produces better blood pressure control while preserving the normal 10% decline in blood pressure in many individuals that occurs at night (nocturnal dipping).
2. Loop diuretics are commonly used in patients admitted with acute exacerbation of heart failure. Diuresis leads to loss of water and salt with resulting decrease in intravascular volume thus lowering ventricular filling pressure and reducing pulmonary edema.
3. Furosemide decreases intracranial pressure by inducing systemic diuresis and decreasing cerebrospinal fluid production. Furosemide can be administered as single-drug therapy (0.5 to 1.0 mg/kg IV) or as a lower dose (0.1 to 0.3 mg/kg IV) in combination with mannitol (combination of furosemide and mannitol is more effective in decreasing intracranial pressure than either drug alone but severe dehydration and electrolyte imbalance are also more likely).
C. Side effects of loop diuretics most often manifest as abnormalities of fluid and electrolyte balance (can lead to hypokalemia and increase the likelihood of digitalis toxicity).
1. Acute or chronic treatment of patients with diuretics, including loop diuretics, may result in tolerance to the diuretic effect (“braking phenomenon”).
a. Acute tolerance is presumed to reflect activation of the renin-angiotensin system to retain sodium and water in the presence of a contracted extracellular fluid volume.
b. With chronic use of diuretics, there is evidence of a compensatory hypertrophy of those portions of the renal tubule (especially distal convoluted tubules) responsible for sodium retention, leading to decreased diuretic effectiveness. When tolerance develops in a patient treated chronically with furosemide, it may be possible to reestablish a diuretic effect with the administration of a thiazide diuretic, which blocks the hypertrophied Na+ reabsorption sites.
2. Loop diuretics should only be administered to patients with a normal or increased intravascular fluid volume. Hypotension may result from administration of loop diuretics to hypovolemic patients exacerbating renal ischemic injury and concentrating nephrotoxins in the renal tubules.
3. Furosemide increases renal tissue concentrations of aminoglycosides and enhances the possible nephrotoxic effects of these antibiotics. Cephalosporin nephrotoxicity may also be increased by furosemide.
4. Loop diuretics potentiate nondepolarizing neuromuscular blockade.
5. The renal clearance of lithium is decreased in the presence of diuretic-induced decreases in sodium reabsorption, and plasma concentrations of lithium may be acutely increased by the IV administration of furosemide in the perioperative period.
6. Ototoxicity, either transient or permanent, is a rare, dose-dependent complication associated with the use of loop diuretics.
IV. Thiazide diuretics are most often administered for long-term treatment of essential hypertension in which the combination of diuresis, natriuresis, and vasodilation are synergistic (thiazides are usually administered in combination with other antihypertensives).
A. Pharmacokinetics and Pharmacodynamics (see Fig. 22-1)
1. Thiazide diuretics are readily absorbed when administered orally (hydrochlorothiazide has a 60% to 70% bioavailability).
2. Thiazides’ effectiveness markedly decreases in patients with renal insufficiency.
3. Thiazide diuretics have a long half-life of 8 to 12 hours, allowing for a convenient once-a-day dosing.
B. Clinical Uses
1. Thiazide diuretics are recommended as first-line therapy for essential hypertension and the use of chlorthalidone specifically has been shown to decrease the risk of major cardiovascular events. The antihypertensive effect of thiazide diuretics is due initially to a decrease in extracellular fluid volume, often with a decrease in cardiac output, which normalizes after several weeks. The sustained antihypertensive effect of thiazide diuretics is due to peripheral vasodilation, which requires several weeks to develop.
2. Because they stimulate calcium reabsorption, thiazide diuretics are used in the treatment of calcium-containing renal calculi.
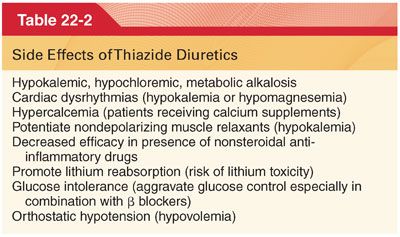
C. Side Effects (Table 22-2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


