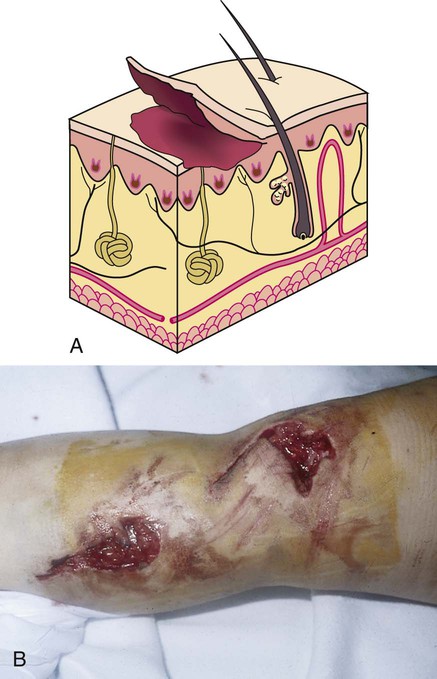
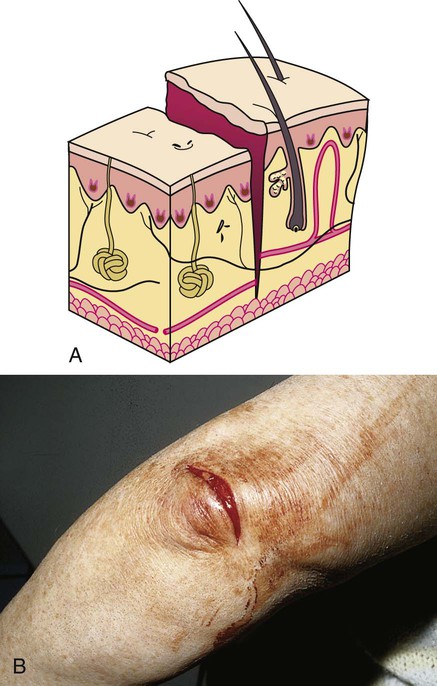
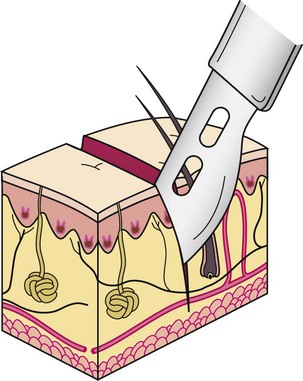
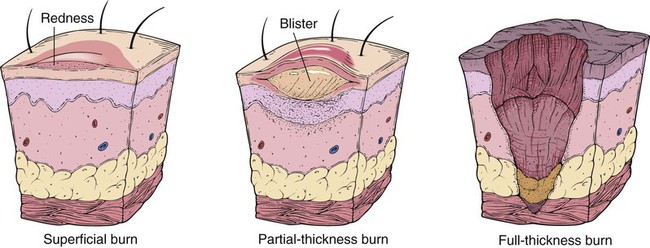
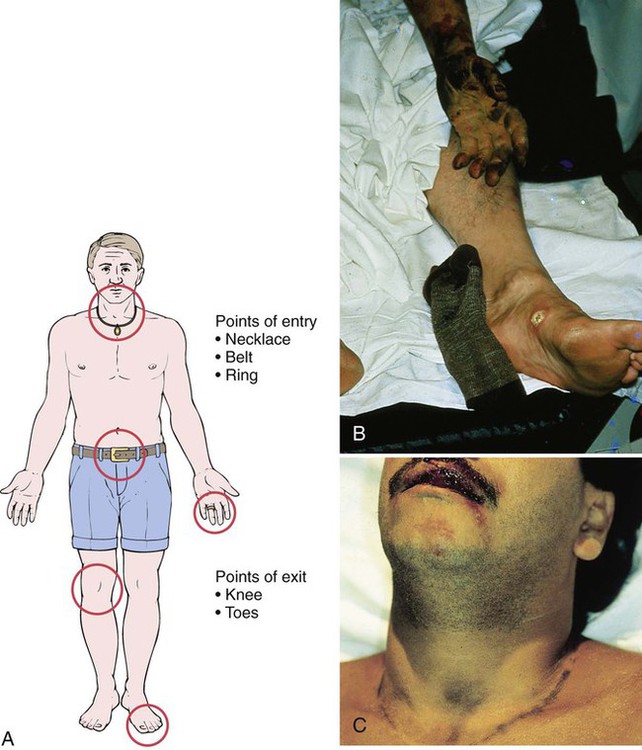
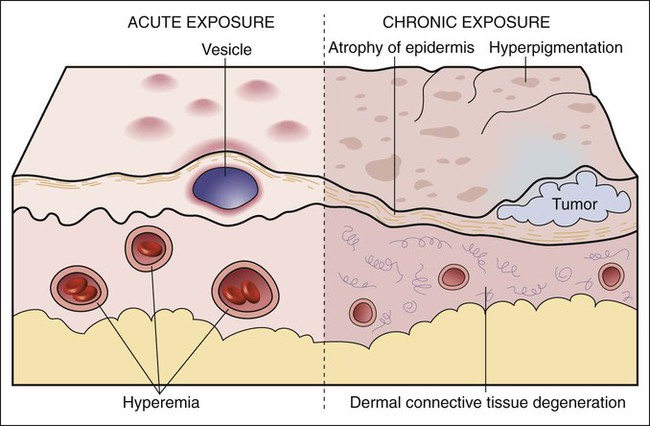
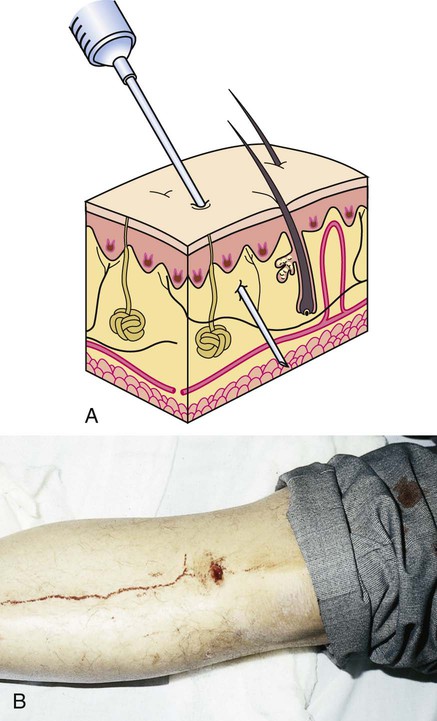
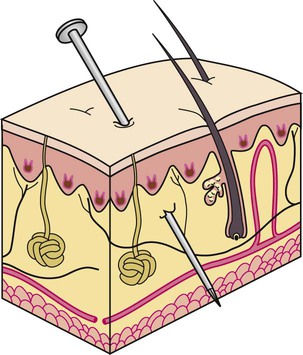
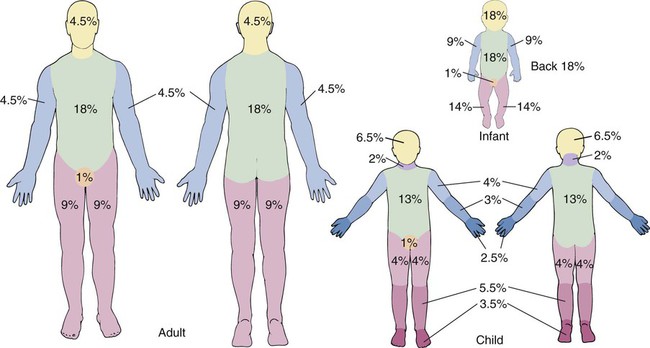
After studying Chapter 15, you should be able to: 1. List the major types of trauma. 2. List environmental factors that may result in trauma. 3. Name three factors that generally need to be addressed in open trauma. 4. Distinguish between an abrasion and an avulsion injury. 5. Describe conditions that require prophylaxis with tetanus toxoid. 6. Explain the risk to health care workers of puncture wounds. 7. Describe management of foreign bodies in the ear, eye, and nose. 8. Name the conditions classified as thermal insults. 9. Explain the rule of nines in adults with burns and how it is used. 10. Describe the possible injuries caused by (a) electrical shock and (b) lightning. 11. Define hypothermia and list those most at risk. 12. Describe the guidelines for treating (a) frostbite, (b) insect bites, and (c) snake bites. 13. Explain the pathology that results in the pain and numbness of carpal tunnel syndrome. 14. Name the best treatment of child abuse and neglect and elder abuse and neglect. 15. Explain the importance of immediate intervention in shaken infant (baby) syndrome. 16. Discuss special concerns in the diagnosis of (a) intimate partner violence, (b) sexual abuse, and (c) sexual assault/rape. Bleeding can be a factor in open trauma and must be addressed at once. Some injuries need only basic first aid, whereas others require medical intervention and surgical repair. Regardless of the severity of the injury, appropriate treatment aids healing and lessens scarring. Orthopedic and neurologic traumas are addressed in Chapters 7 and 13, respectively. With avulsion injuries, a portion of the skin and possibly underlying tissue is torn away, either completely or partially (Figure 15-2, A and B). E15-2, A and B Puncture wounds result when a pointed or sharp foreign object penetrates the soft tissue (Figure 15-3, A and B). Animals bites, discussed later in this chapter, also may be considered puncture wounds. Puncture wounds cause pain and usually very little bleeding. Redness at the site may be noted, or there may be no indication of the wound other than the pain. A puncture wound may not have a dramatic appearance, therefore meticulous inspection of the area and underlying structures should be carefully performed. If the foreign body that caused the injury is protruding out of the wound, it is described as an impaled object (Figure 15-4). Lacerations result when a sharp object cuts the skin and possibly underlying soft tissue. Diagnosis is made by visual and ophthalmoscopic examination of the eye. A history of feeling something in the eye combined with the circumstance of possible exposure to foreign bodies is helpful. Staining the eye with fluorescein to visualize a corneal abrasion will confirm the presence or previous presence of a foreign body. Refer to Chapter 5 for discussion on corneal abrasion. The patient who has experienced a burn usually has pain. The extent of the burn, along with the percent of body surface involved, usually is related proportionately to the degree of pain. Depending on the depth and nature of the burn, the skin surface may be reddened, blistered, or charred (Figure 15-7). E15-8, A and B Determination of the depth (Figure 15-8) and extent (Figure 15-9) of a burn is important. Pain intensity depends on the amount of nerve tissue that is involved or destroyed. Superficial burns involve only the outer layers of the skin, which usually appear only reddened, and yet these burns are painful. Partial-thickness burns involve all layers of the skin; they produce blisters and are quite painful. Full-thickness burns involve both the skin and the underlying subcutaneous tissue. Resultant destruction of nerve endings often results in minimal pain in that particular area; however, pain may be reported in areas around the periphery of the burn site. Prompt assessment of the percent of skin surface area involved in the burn injury is achieved by applying the rule of nines. The rule of nines provides a fast and fairly accurate calculation of the body surface involved. Percentages used to ascertain the burned tissue area in the adult are as follows: head, 9%; anterior trunk, 18%; posterior trunk, 18%; entire right arm, 9%; entire left arm, 9%; anterior surface right leg, 9%; posterior surface right leg, 9%; anterior surface left leg, 9%; posterior surface left leg, 9%; and perineum, 1%. Percentages in children and infants are slightly different. Another method of designating a percentage of body surface involvement is used by the ICD-9-CM and ICD-10-CM code books. Refer to the current edition of the ICD-9-CM and ICD-10-CM code books for these percentages. Treatment depends on the source of the burns. Heat burns (from flame, liquid scalds, or superheated air) should be cooled with cool water and covered with dry sterile dressings until seen by a physician. Sunburns should be treated with the application of cool water, and the damaged skin may be sprayed with antiseptic and analgesic sprays (Figure 15-10). OTC medications including aspirin, ibuprofen, and naproxen may be used for relief of sunburn pain. Cool compresses applied to the areas of sunburned skin may also provide pain relief. Skin burned with chemicals other than lime, which must first be brushed away, should be flushed with cool water for at least 15 minutes, covered with a sterile dressing, and treated by a physician. Electrical burns should be examined for points of entry (rings, belts, necklaces) and exit (knees, toes) (Figure 15-11). These areas should be covered with dry sterile dressings and treated by a physician. The person who has sustained electrical shock experiences tissue damage from the point of entry of the electricity to the point of exit. The electrical current follows the path of least resistance through the body, usually along nerve routes. The current enters the body at the point of contact with the electrical source and exits at the point of grounding (see Figure 15-11) E15-9. As the alternating current passes through the body, it may produce muscle contractions, causing the person to be thrown from the source. This can result in lacerations, fractures, or head trauma. One major concern with electrical shock injuries is the development of cardiac dysrhythmias.
Disorders and Conditions Resulting From Trauma
Trauma
Open Trauma
Abrasions
Avulsion
Description
Puncture Wounds
Description
Symptoms and Signs
Lacerations
Description
Foreign Bodies
Foreign Bodies in the Eye
Description
 ICD-9-CM Code 930.9 (Unspecified site)
ICD-9-CM Code 930.9 (Unspecified site)
 ICD-10-CM Code T15.90XA (Foreign body on external eye, part unspecified, unspecified eye, initial encounter)
ICD-10-CM Code T15.90XA (Foreign body on external eye, part unspecified, unspecified eye, initial encounter)
Diagnosis
Thermal Insults
Burns
Symptoms and Signs
Diagnosis
Treatment
Electrical Shock
Etiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree