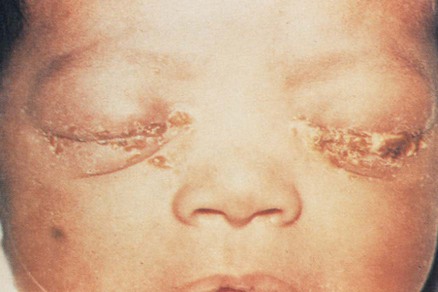
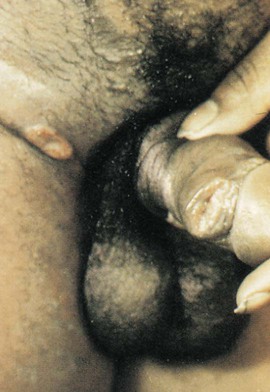
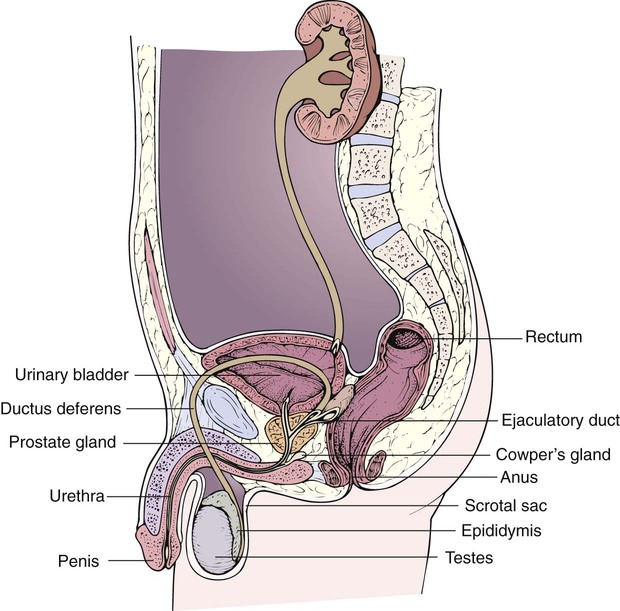
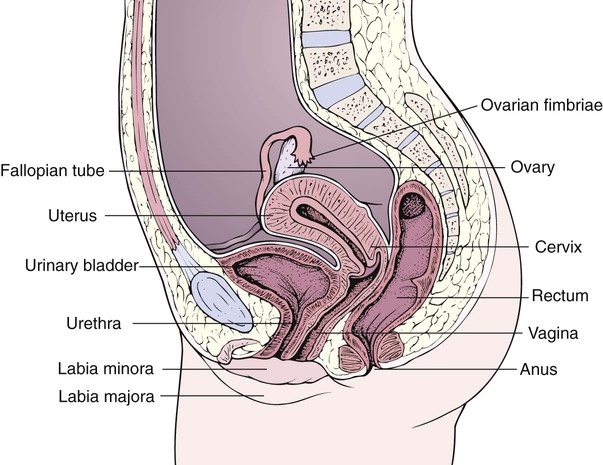
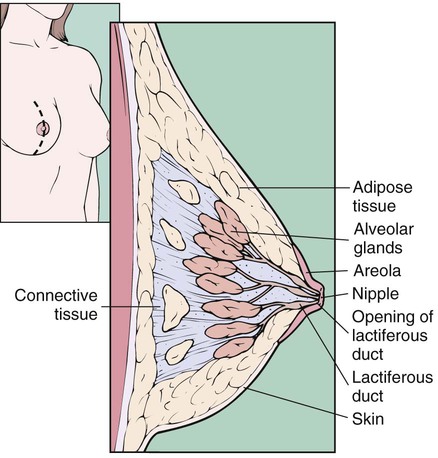
After studying Chapter 12, you should be able to: 1. Identify risk factors for sexually transmitted diseases (STDs). 2. Explain what a silent STD is and give an example. 3. Name the complications of untreated gonorrhea. 4. Recall how trichomoniasis is diagnosed. 5. Explain how genital herpes is transmitted. 6. Explain why women with genital herpes are advised to have regular Pap (Papanicolaou) smears. 7. Describe the stages of untreated syphilis. 8. Explain why hepatitis B is classified as sexually transmitted. 9. List the possible causes of dyspareunia in men and women. 10. Name drugs that can contribute to impotence. 11. Name a common causative factor in male and female infertility. 12. Explain the value of prostate-specific antigen (PSA) as a screening test. 13. Discuss the medical interventions for prostatic cancer. 14. Explain how varicocele may contribute to male infertility. 15. Explain why physicians encourage monthly testicular self-examinations for younger men. 16. Explain what causes the dysmenorrhea associated with endometriosis. 17. Discuss the importance of early diagnosis and prompt treatment of pelvic inflammatory disease. 18. Discuss the advantages and possible risks of hormone replacement therapy for the postmenopausal woman. 19. Explain how uterine prolapse, cystocele, and rectocele may be corrected surgically. 20. List the risk factors for cervical cancer. 21. Name the leading cause of deaths attributed to gynecologic malignancy. 22. List some possible causes of ectopic pregnancy. 23. Explain how a pregnant woman is monitored for toxemia. 24. Describe abruptio placentae. 25. List the factors that place women at higher risk for breast cancer. 26. Explain why the HPV vaccine is recommended for girls and young women, and more recently for men. The male reproductive system functions to transfer the sperm cells to the female for fertilization of the ovum. The testes produce the sperm and the hormones necessary for the development and maintenance of the secondary sex characteristics. The sperm is transported through the series of ducts beginning with the epididymis, the ductus deferens, and the ejaculatory ducts. The seminal vesicles, the prostate gland, the bulbourethral glands, and the penis are accessory organs that help to propel the sperm on its journey to meet the egg (Figure 12-1). The female reproductive system nourishes and enables the development of the fertilized ovum. The ovaries (which contain the woman’s lifetime supply of eggs) produce and release the egg and the hormones necessary for the development of secondary sex characteristics and for maintenance of a pregnancy. The ductal system for transport, nourishment, and growth of the fertilized ovum includes the fallopian tubes and the uterus. Other principal parts of the female reproductive system include the cervix, the vagina, and the external genitalia (Figure 12-2). The breasts are accessory organs of reproduction and are two milk-producing glands (Figure 12-3). When a woman is pregnant, the breast tissue is stimulated by both ovarian and placental hormones to prepare for lactation. After delivery, lactating hormones further stimulate the breast tissue to produce and release milk to nourish the infant. STD rates in the United States are among the highest in the world and are growing; syphilis is rising in the United States for the first time in many years. The majority of reported syphilis cases in the United States continue to be among men who have sex with other men (MSM). Recent statistics show 1 in 4 teenagers get sexually transmitted diseases. Attempts to control this rampant public health problem are focusing on research, education, and prevention campaigns. Prevention messages point out high-risk sexual behavior patterns and lifestyles and warn of possible predisposing health problems. Requirements for reporting STDs vary from state to state. However, several STDs that, when diagnosed, must be reported to state health departments and the CDC for statistical purposes are chlamydia, gonorrhea, syphilis, chancroid, HIV, AIDS, and hepatitis B. (See Chapter 8 for a discussion of hepatitis B.) Infection with the common bacterium Neisseria gonorrhoeae usually results from sexual transmission. Although recent statistics indicate a decline in the disease rate, drug resistance is on the rise. Because transmission is also possible during birth, newborns must be protected from eye infections that can lead to blindness (Figure 12-4). Therefore prophylactic erythromycin salve is administered routinely at birth. Genital herpes is an incurable, recurrent infection of the skin of the genital area, with ulcerations spread by direct skin-to-skin contact, causing painful genital sores similar to cold sores (Figure 12-5). Syphilis is a chronic, systemic, sexually transmitted infection that consists of four stages. Syphilis begins with the presence of a painless but highly contagious local lesion called a chancre on the male or female genitalia (Figure 12-7). Without early treatment during the primary stage, it becomes a systemic, chronic disease that can involve any organ or tissue. In 1 to 2 months, when the primary lesion heals, the causative organism (the Treponema pallidum spirochete) has disseminated throughout the body and multiplied, producing lesions wherever the organisms are most prevalent, including the skin, lymph nodes, cardiovascular system, brain, and spinal cord. The disease continues to be contagious during the secondary stage, when there is systemic manifestation. This stage can present many symptoms, including fever, headaches, aching of the joints, mouth sores, and rashes on the palms of the hands and soles of the feet (Figure 12-8). Then a latent period, lasting from 1 to 40 years, may follow, during which the infection is generally subclinical or asymptomatic. In the late stage, the lesions, called gummas, have invaded body organs and systems, causing widespread damage to the point of being disabling and life threatening. Syphilis is caused by infection with the T. pallidum spirochete through sexual contact or other direct contact with infected lesions or infected body fluids. It is highly contagious when a chancre is present (see Figure 12-7). The rising rate of syphilis among men is driven by men having sex with men (MSM). Congenital transmission can occur during pregnancy. The shallow and painless lesion appears on the skin or mucous membrane, at the site of entry, 7 to 10 days after sexual contact with an infected person (Figure 12-9). Tender superlative inguinal adenopathy is noted upon physical examination. The ulcer usually deepens and becomes purulent and can be spread to other areas of the body by autoinoculation. Erectile dysfunction/impotence is a consistent inability to achieve or maintain penile erection. N52.0 (Vasculogenic erectile dysfunction) N52.01 (Erectile dysfunction due to arterial insufficiency) N52.02 (Corporo-venous occlusive erectile dysfunction) N52.03 (Combined arterial insufficiency and corporo-venous occlusive erectile dysfunction) N52.1 (Erectile dysfunction due to diseases classified elsewhere) N52.2 (Drug-induced erectile dysfunction) N52.3 (Post-surgical erectile dysfunction) N52.31 (Erectile dysfunction following radical prostatectomy) N52.32 (Erectile dysfunction following radical cystectomy) N52.33 (Erectile dysfunction following urethral surgery) N52.34 (Erectile dysfunction following simple prostatectomy) N52.39 (Other post-surgical erectile dysfunction) N52.8 (Other male erectile dysfunction)
Diseases and Conditions of the Reproductive System
The Normally Functioning Reproductive Systems
Sexually Transmitted Diseases
Gonorrhea
Etiology
Genital Herpes
Description
Genital Warts (Condylomata Acuminata)
Syphilis
Description
Symptoms and Signs
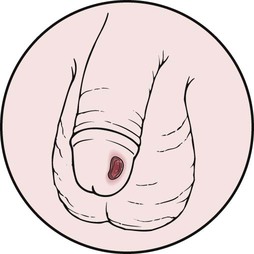
Etiology
Chancroid
Symptoms and Signs
Sexual Dysfunction
Erectile Dysfunction/Impotence
 ICD-9-CM Code 607.84 (Impotence of organic origin)
ICD-9-CM Code 607.84 (Impotence of organic origin)
 ICD-10-CM Code N52 (Male erectile dysfunction)
ICD-10-CM Code N52 (Male erectile dysfunction)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree