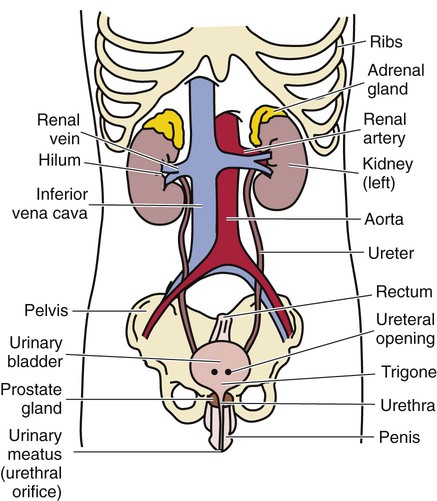
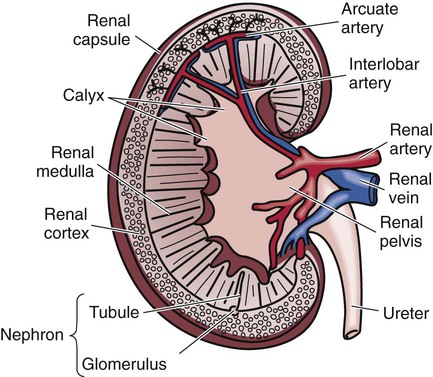
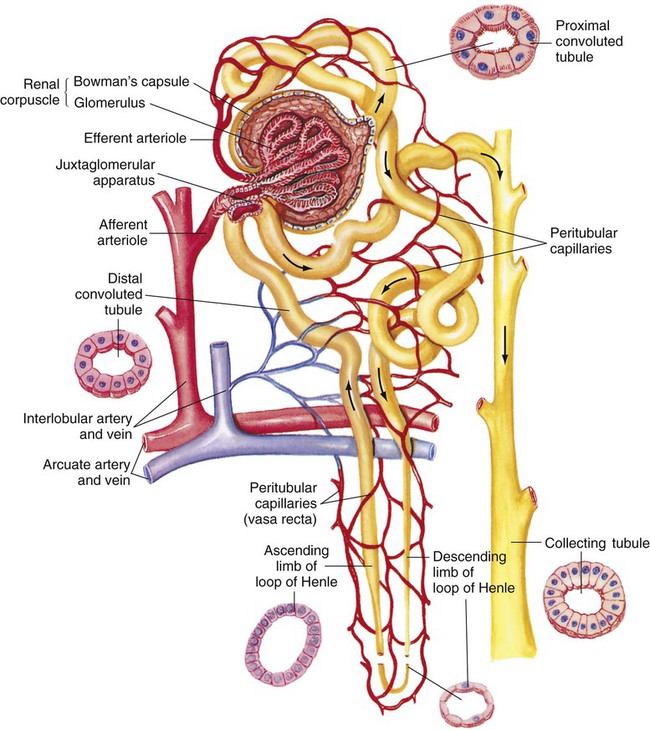
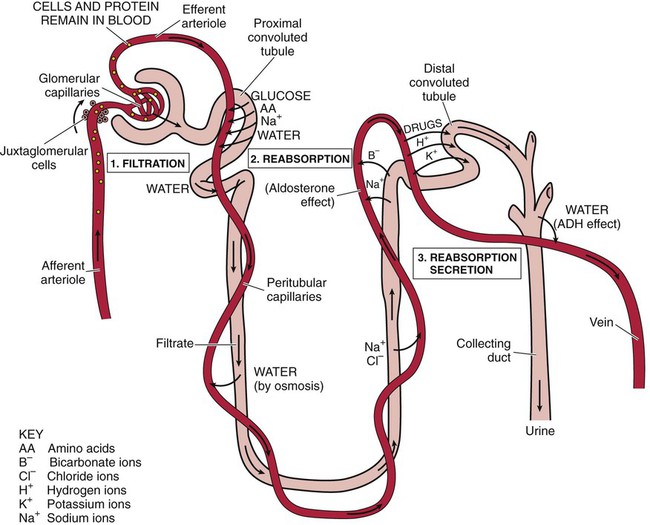
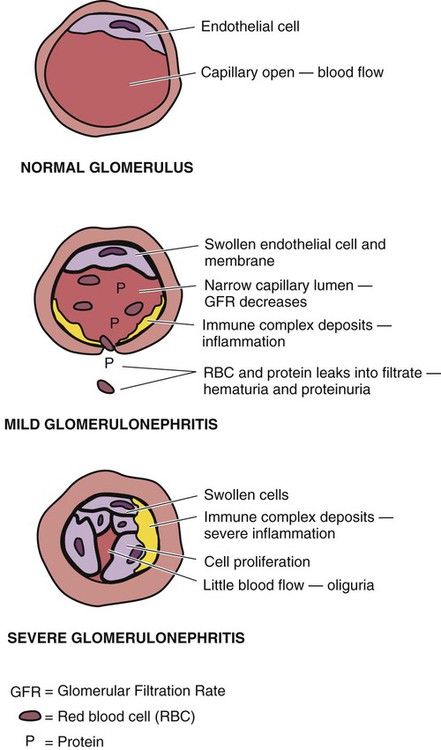
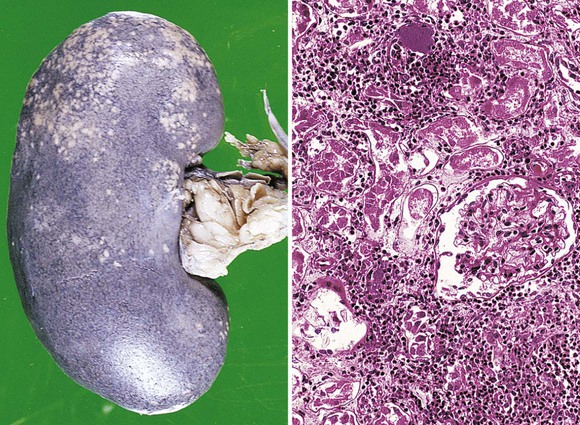
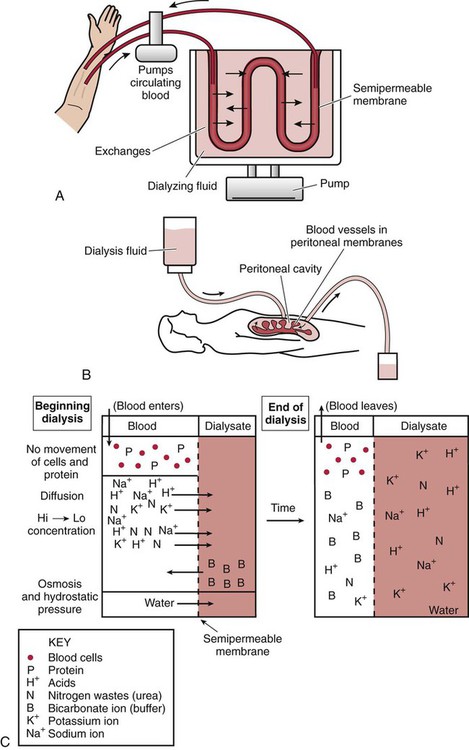
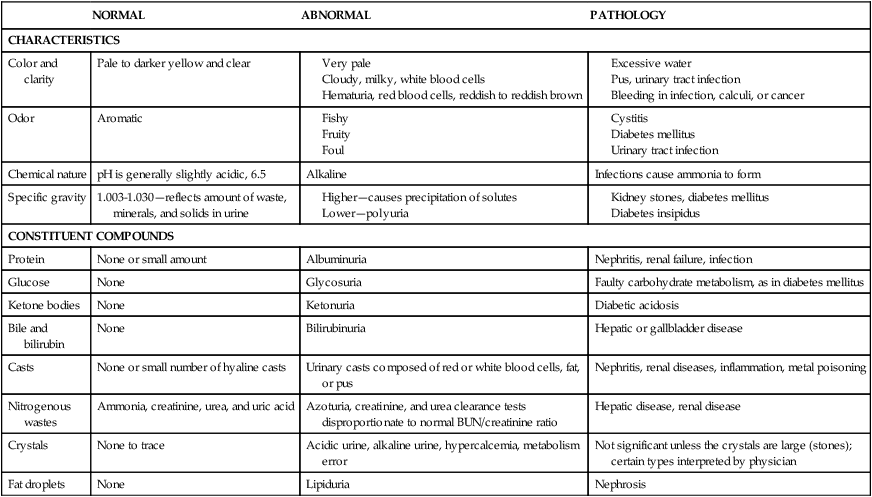
After studying Chapter 11, you should be able to: 1. Explain the structure and function of the normal urinary system. 2. Explain how pathologic conditions of the urinary system threaten homeostasis and result in illness. 3. Explain the diagnostic value of urinalysis. 4. Relate the symptoms and signs of acute glomerulonephritis. 5. Describe how immune mechanisms are suspected to be a causative factor of acute and chronic glomerulonephritis. 6. Distinguish between hemodialysis and peritoneal dialysis. 7. Identify the hallmark sign of nephrosis. 8. List some nephrotoxic agents. 9. Explain why acute renal failure is considered a clinical emergency. 10. Discuss treatment measures for prolonging life of the patient with chronic renal failure. 11. Identify the etiology and diagnosis of pyelonephritis. 13. Describe the common symptoms of renal calculi and list possible complications. 14. List causes of infectious cystitis and urethritis. 15. Describe diabetic nephropathy. 16. Contrast neurogenic bladder with stress incontinence. 17. Describe the polycystic kidney and discuss the treatment options. 18. Identify those most at risk for renal cell carcinoma and bladder tumors. 19. List and describe symptoms of renal cell and bladder carcinoma. The urinary system is responsible for producing, storing, and excreting urine; these processes prevent the body from becoming toxic. The kidneys facilitate reabsorption of necessary nutrients, water, and electrolytes. Cleansing the blood of the waste products of metabolism and regulating the water, salts, and acids in the body fluids ensure the body’s homeostasis. Regulation of volume of water in the body is an essential function of the urinary system. E11-1 The urinary system includes the kidneys, which manufacture urine and play a role in the regulation of systemic blood pressure and the accessory structures. The ureters transport urine and the bladder stores urine until it is excreted voluntarily through the urethra. The organs and accessory structures of the urinary system consist of two kidneys, two ureters, the urinary bladder, and the urethra (Figure 11-1). Each kidney (Figure 11-2) is composed of about 1 million microstructures called nephrons (Figure 11-3). The nephrons, the units of function in the kidney, are responsible for filtration, reabsorption, and secretion of urine. Figure 11-4 depicts the formation of urine. The urine is transported from the nephron to the renal pelvis and then to the ureters. The kidney has many other functions, including the secretion of rennin, a hormone that raises blood pressure, and erythropoietin, which acts as a stimulus for red blood cell (RBC) production. It also has a role in the activation of vitamin D. Each kidney, (see Figure 11-2) as a primary organ of the urinary system, processes blood to form urine that contains waste products to be eliminated from the body. The bean-shaped organs, about the size of a human fist, are located in the back retroperitoneally to the abdominal cavity and lateral to the spinal column. Each kidney is separated into three areas or regions: the cortex, the medulla, and the renal pelvis. Blood enters the kidneys by way of the renal arteries through the hilum. Refer to Figures 11-1 and 11-2 for blood supply to and from the kidneys. The arteries divide and divide again and again into smaller arteries that ultimately enter the nephrons. Blood leaves the kidneys by way of the renal veins. Urine leaves the kidneys by way of two long, slender tubes, the ureters that enter the lower part of the urinary bladder. Peristalsis in the muscular walls of the ureters moves the urine into the urinary bladder where it is temporarily stored until it is passed from the body by way of the urethra. Urine is voluntarily excreted from the bladder by way of the urethra in a process called urination or micturition. The urethra is a tubular structure that extends from the base of the urinary bladder to the urinary meatus (urethral orifice) on the external surface of the body. Refer to Figure 11-1. The function of the urinary system often is evaluated by urinalysis (Table 11-1) and blood tests (Table 11-2). Normal results demonstrate proper filtration, absorption, and elimination of metabolic waste, as well as precise fluid and electrolyte balance. Other tests for urinary tract disorders include culture and sensitivity tests to determine appropriate antibiotic therapy, radiologic tests that visualize structural and functional abnormalities, cystoscopy (see Figure 11-4), and biopsy of lesions. TABLE 11-1 *Routine urinalysis is a physical, chemical, and microscopic examination of urine for abnormal elements that may help to estimate renal function and provide clues of systemic disease. This table includes some important characteristics and elements screened for in basic urinalysis. Other normal constituents of urine that are studied routinely for diagnosis include calcium, urea, uric acid, creatinine, sodium chloride, hormones, potassium, magnesium, phosphates, and sulfates. TABLE 11-2 Acute glomerulonephritis is an inflammation and swelling of the glomeruli (see Figure 11-3) of the kidneys. It can be a primary disease of the kidney or may develop secondary to a systemic disease. This condition usually follows a streptococcal bacterial infection of the throat or skin. This condition usually follows an infection caused by group A β-hemolytic streptococcus. E11-2 It also can be idiopathic or may result from an immune reaction that causes circulating antigen-antibody complexes to become trapped within the network of capillaries of a glomerulus. In some cases, the antigen is endogenous (arising from within) as an accompaniment of tumors. The injury to the glomeruli results in a decrease in the rate of filtration of the blood, and consequently retention of water and salts in the body. Figure 11-5 is a schematic representation of changes occurring in the nephron with acute poststreptococcal glomerulonephritis. The diagnosis is made by the clinical findings, clinical history, and urinalysis. The urine shows gross blood and the presence of RBCs, white blood cells (WBCs), renal tubular cells, and casts. Proteinuria may be present because of increased permeability of the glomerular membrane. Blood tests show elevated blood urea nitrogen (BUN), hypoalbuminemia, and an elevated erythrocyte sedimentation rate (ESR). Kidney-ureter-bladder (KUB) radiographic films and ultrasonography may reveal bilateral enlargement of the kidneys. Renal biopsy may confirm the diagnosis (Figure 11-6). The goals of treatment are to control edema, treat the hypertension, and prevent congestive heart failure and uremia. The patient is given supportive measures for comfort. Medical treatment includes the administration of antihypertensives, diuretics, and antibiotics if urinary tract infection (UTI) develops. Protein, salt (Na+ and phosphate), and fluid intake may be limited in the diet. ACE inhibitors are often used to aid in the reduction of excess protein in the urine. The patient may require dialysis (see Figure 11-8) or may be a candidate for kidney transplantation. Nephrotic syndrome is caused by increased permeability of the glomerulus, indicating renal damage. This condition may follow an attack of glomerulonephritis or it may be the result of exposure to certain toxins or drugs (Box 11-1), pregnancy, or kidney transplants. Metabolic diseases, such as diabetes mellitus, certain infections, and allergic reactions are conditions that may lead to nephrotic syndrome. Prompt treatment of glomerulonephritis is important in prevention of this condition. Avoiding exposure to certain toxins or drugs (see Box 11-1) helps prevent the syndrome, as does prompt treatment after exposure to these toxins. Monitoring the kidney function of women during pregnancy and of any patients with metabolic diseases, such as diabetes mellitus, certain infections, and allergic reactions may assist the physician in detecting malfunction early on, and therefore treatment can be instituted early on.
Diseases and Conditions of the Urinary System
Orderly Function of the Urinary System
NORMAL
ABNORMAL
PATHOLOGY
CHARACTERISTICS
Color and clarity
Pale to darker yellow and clear
Odor
Aromatic
Chemical nature
pH is generally slightly acidic, 6.5
Alkaline
Infections cause ammonia to form
Specific gravity
1.003-1.030—reflects amount of waste, minerals, and solids in urine
CONSTITUENT COMPOUNDS
Protein
None or small amount
Albuminuria
Nephritis, renal failure, infection
Glucose
None
Glycosuria
Faulty carbohydrate metabolism, as in diabetes mellitus
Ketone bodies
None
Ketonuria
Diabetic acidosis
Bile and bilirubin
None
Bilirubinuria
Hepatic or gallbladder disease
Casts
None or small number of hyaline casts
Urinary casts composed of red or white blood cells, fat, or pus
Nephritis, renal diseases, inflammation, metal poisoning
Nitrogenous wastes
Ammonia, creatinine, urea, and uric acid
Azoturia, creatinine, and urea clearance tests disproportionate to normal BUN/creatinine ratio
Hepatic disease, renal disease
Crystals
None to trace
Acidic urine, alkaline urine, hypercalcemia, metabolism error
Not significant unless the crystals are large (stones); certain types interpreted by physician
Fat droplets
None
Lipiduria
Nephrosis
TEST
DESIGNED TO EVALUATE
Clearance test
Rate of glomerular filtration
Concentration and dilution tests
Functional capacity of renal tubular cells to adaptively retain and/or eliminate water
Serum creatinine and BUN
Capacity to eliminate end products of protein metabolism
Protein in urine
Permeability of glomerular membrane
Acute Glomerulonephritis
Description
Etiology
Diagnosis
Chronic Glomerulonephritis
Treatment
Nephrotic Syndrome (Nephrosis)
Etiology
Prevention
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree