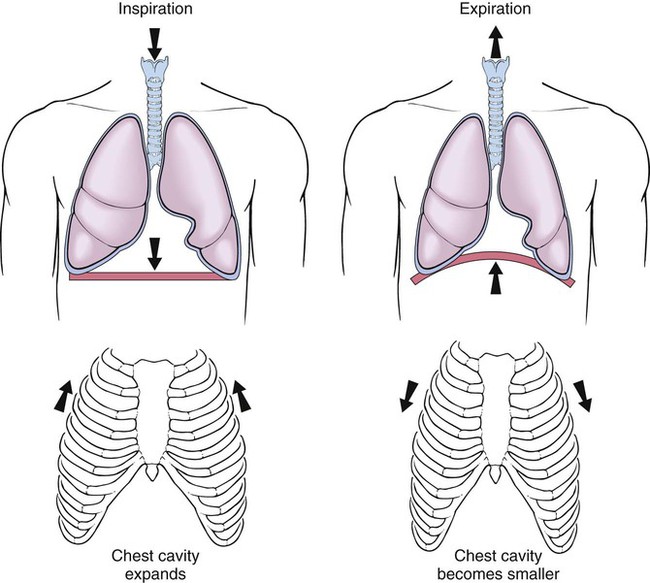
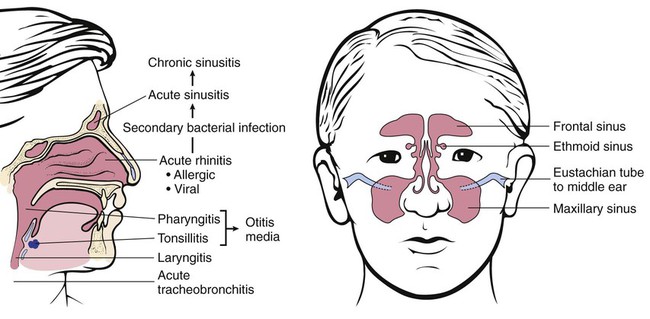
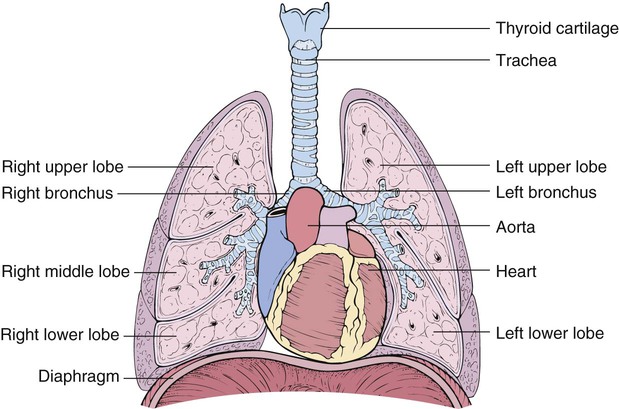
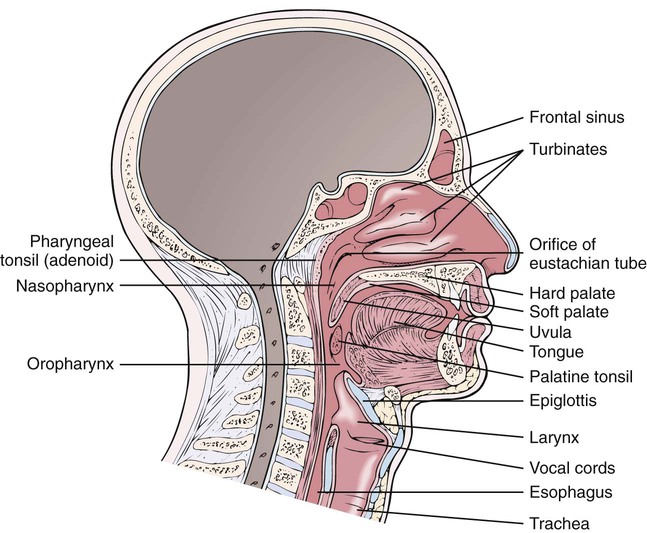
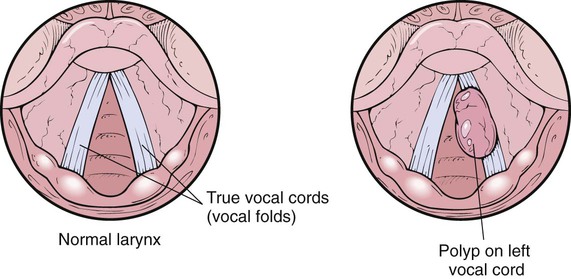
After studying Chapter 9, you should be able to: 1. Explain the process of respiration. 2. Discuss the causes and medical treatment for (a) the common cold, (b) sinusitis, and (c) pharyngitis. 3. Name the treatment of choice for nasal polyps. 4. Discuss the prognosis of cancer of the larynx. 5. Define atelectasis and discuss some possible causes. 6. Name some systemic disorders that might cause epistaxis. 7. Compare the clinical pictures of (a) a patient with pulmonary embolism and (b) one with pneumonia. 8. List some possible causes of pulmonary abscess. 9. Compare legionellosis with Pontiac fever. 10. Explain who is at greatest risk for (a) respiratory syncytial virus pneumonia and (b) histoplasmosis. 11. List the groups recommended to receive prophylactic use of influenza vaccines. 12. Contrast the pathologic course of acute bronchitis with that of chronic bronchitis. 13. Compare the pathology involved in bronchiectasis with that of pulmonary emphysema. 14. Name and describe three causes of pneumoconiosis. 15. Explain the difference between pneumothorax and hemothorax. 16. Describe the presenting symptoms of pleurisy. 17. Discuss contributing factors to, and concern about, the rising prevalence of pulmonary tuberculosis. 18. Describe the clinical course of infectious mononucleosis. 19. Explain the pathologic changes of the lungs in adult respiratory distress syndrome (ARDS). 20. Name the leading cause of cancer deaths worldwide for both men and women. 21. Explain what determines the prognosis of sarcoidosis. The primary function of the pulmonary system is ventilation and respiration (Figure 9-1). Respiration maintains life by supplying oxygen to organs, tissues, and cells and allowing for the removal of carbon dioxide (a waste product of metabolism). This process is made possible by ventilation (the bellowslike action of the chest) and healthy lung tissue that is adequately perfused with blood. Breathing is controlled by the central nervous system; nerve stimulation of breathing begins in the medulla oblongata and pons. Pulmonary circulation is composed of pulmonary arteries that carry deoxygenated venous blood from the heart to the lungs; pulmonary capillaries in which gas exchange occurs; and pulmonary veins, which return the freshly oxygenated blood to the heart for systemic circulation. Lung tissue itself is supplied with oxygen and nutrients by the blood supply that is carried to it by the bronchial arteries. In the lungs, oxygen inhaled from the air is exchanged with carbon dioxide from the blood; this process is called external respiration. Internal respiration refers to the exchange of gases between the blood and tissue cells. Carbon dioxide then is exhaled as a waste product. Inhaled and exhaled air passes through the respiratory tract, which includes the nose, pharynx, larynx, and trachea (Figure 9-2). E9-1 A muscular, dome-shaped partition called the diaphragm attaches to the lower ribs and separates the thoracic cavity from the abdominal cavity. On inspiration, the diaphragm contracts, pulling downward and causing air to be sucked into the lungs. During expiration, the diaphragm relaxes, pushing upward and forcing air out of the lungs (Figure 9-3). The expansion of the chest cavity, along with diaphragmatic contraction, is an active, energy-requiring process. Exhalation occurs as the stretched chest cavity springs back to its resting state along with the relaxation of the diaphragm. This is a passive process. Chief symptoms indicating respiratory tract disorders that should receive medical attention include: • Dyspnea (difficulty in breathing) • Productive or nonproductive cough that is acute or chronic • Hemoptysis (spitting up blood) Although the common, or “head,” cold is confined to the nose and pharynx, the same viruses can infect the larynx (see “Laryngitis” section) and various areas of the lungs (see “Acute and Chronic Bronchitis” section). The suffix “-itis” is added to the anatomical location where most of the inflammation is occurring (i.e., pharyngitis, laryngitis, tracheitis, or bronchitis). The symptoms of a cold tend to be subjective, and to some extent, depend on which virus is responsible; they include nasal congestion and discharge, sneezing, watering eyes, sore throat, hoarseness of the voice, and coughing. When this highly contagious inflammatory process first begins, the nasal discharge is usually clear and thin. In the adult, the symptoms usually abate in 5 to 7 days and without antibiotic therapy. In some cases the cold progresses and the discharge becomes greenish yellow and thick. Headache, a slight fever, and chills often accompany a cold. A high fever and malaise, however, are more likely to be symptoms of influenza (see “Influenza” section). The common cold is a group of minor illnesses that can be caused by almost 200 different viruses. Cold viruses are not part of normal body flora, thus viruses that cause a cold are passed from one human to another. Colds are frequent diseases and a common cause of absenteeism from work and school. Rhinoviruses cause about one half of the colds in adults. (Some colds may result from mycoplasma and other atypical organisms that are more like bacteria than viruses. These are also transmitted by airborne respiratory droplets.) Viral infections sometimes are followed by bacterial infections of the pharynx, middle ear (see “Otitis Media” section in Chapter 5), sinuses, larynx, or lungs. General poor health, lack of exercise, and poor nutrition predispose one to the common cold. The benefit to be gained from taking oral antihistamines to treat a cold is controversial. Antibiotics are of little value in treating viral infections; however, patients with recurring attacks of bronchitis (see “Acute and Chronic Bronchitis” section) or frequent middle ear infections may receive some protection against these bacteria-caused complications by taking antibiotics. There is some data to suggest that taking zinc lozenges may shorten (slightly) the course of the common cold. The sinuses, cavities behind the facial bones that shape the nose, cheeks, and eye sockets, are normally air filled. In sinusitis, the frontal sinuses (located in the forehead above the eyes) and the maxillary sinuses (located under the maxillary bones in the face) are the most commonly involved sinuses (Figure 9-4). When the frontal sinuses are affected, a headache is common over one or both eyes, especially upon waking in the morning. Pain and tenderness, felt just above the eyes and that usually intensifies when bending over, are also common symptoms. Pain in the cheeks and upper teeth is a symptom of sinusitis in the maxillary sinuses. Drainage, if present, will be a thick and greenish yellow mucopurulent discharge. The course of acute sinusitis is 3 to 4 weeks. Sinusitis can be caused by either viral, fungal, or, more commonly, bacterial infections that travel to the sinuses from the nose, often after the patient has been infected by a common cold. This occurs easily because the mucous membranes that line the nasal cavity extend into and also line the sinuses. One is predisposed to sinusitis by any condition that blocks sinus drainage and ventilation (e.g., a deviated nasal septum, or nasal polyps). Sinusitis also may result as a consequence of swimming or diving, tooth extractions, or tooth abscess, as well as allergies that affect the nasal passages. The cause of chronic sinusitis may never be determined; however, common variable immunodeficiency disease may be involved (see Chapter 3). Nasal polyps are not harmful but can become large enough to obstruct the nasal airway, making breathing difficult. Polyps often affect or impair the sense of smell (see “Anosmia” section). When polyps obstruct one of the sinuses, symptoms of sinusitis are present (see “Sinusitis” section). Dysphonia is usually the only symptom of a tumor on the larynx. No influenza-like symptoms occur as with laryngitis (see “Laryngitis” section), but when the tumor is malignant, dysphagia may be experienced. In children with tumors, a high-pitched crowing sound called stridor is present because of their small airways. Hoarseness caused by a benign tumor is usually intermittent, whereas hoarseness caused by cancer is continuous and gradually becomes worse. Neither type of laryngeal tumor is common, but malignant tumors are slightly more common in men than women. There are two types of benign tumors: papillomas, which usually appear as multiples, and polyps, which usually appear singly (Figure 9-7). These tumors are caused by misuse or overuse of the vocal cords, although smoking and reflux are contributing factors. Malignant tumors occur more often in those who indulge in heavy tobacco use. If the tumor involves the vocal cord area of the larynx, persistent hoarseness tends to occur early in the disease process and is the most common initial complaint. Hoarseness related to benign causes, such as a vocal cord polyp or nodule caused by chronic irritation or overuse, is usually intermittent, whereas that caused by a malignant neoplasm is continuous and gradually becomes worse over time. Other symptoms may include dysphagia, hemoptysis, chronic cough, referred pain to the ear, and stridor (a high-pitched crowing sound). Airway obstruction also may occur depending on the tumor location. No influenza-like symptoms as with laryngitis are present (see “Laryngitis” section). Hemoptysis is the coughing or spitting up of blood from the respiratory tract.
Diseases and Conditions of the Respiratory System
Orderly Function of the Respiratory System
Common Cold/Upper Respiratory Tract Infection
Symptoms and Signs
Etiology
Treatment
Sinusitis
Symptoms and Signs
Etiology
Nasal Polyps
Symptoms and Signs
Tumors of the Larynx
Symptoms and Signs
Etiology
Laryngeal Cancer
Symptoms and Signs
Hemoptysis
Description