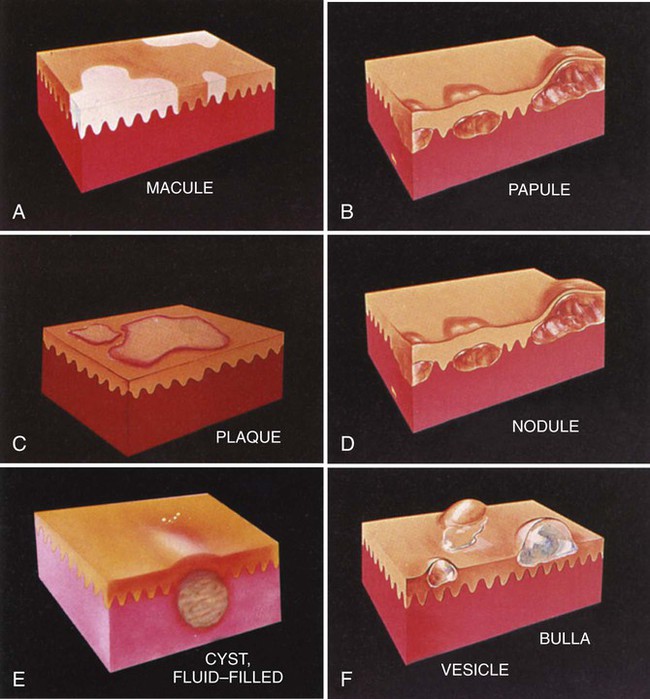
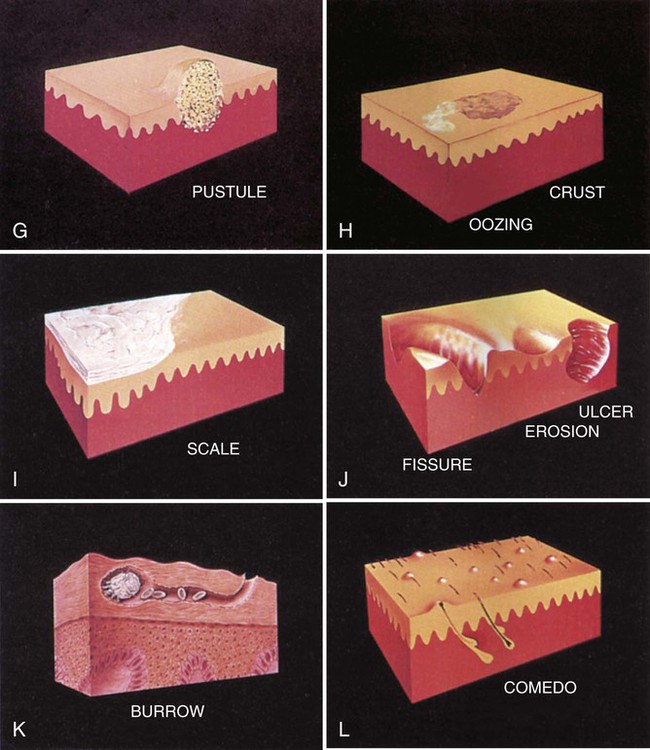
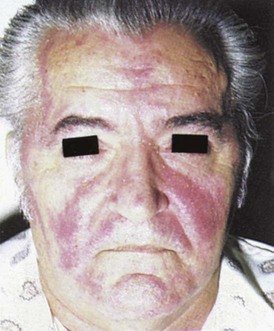
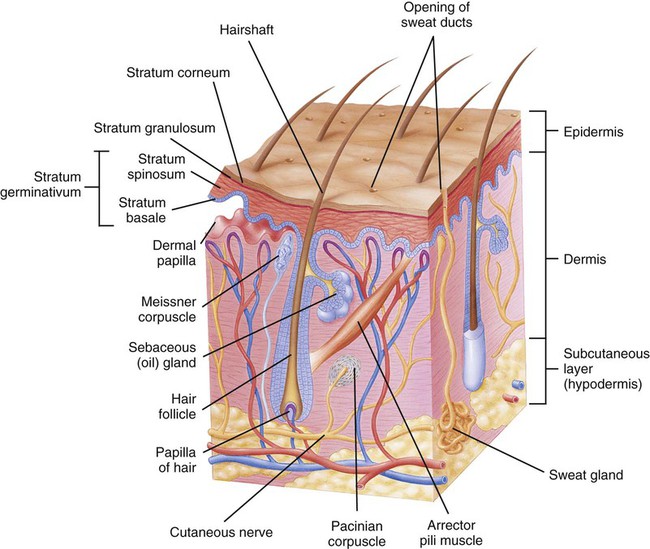
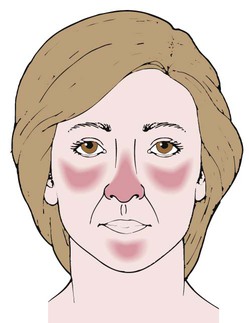
After studying Chapter 6, you should be able to: 1. Explain the functions of the skin. 2. Recognize common skin lesions. 3. Describe how seborrheic dermatitis affects the skin. 4. Discuss the possible causes of contact dermatitis, atopic dermatitis, and psoriasis. 5. Describe the treatment of acne vulgaris. 6. Explain the pathologic course of herpes zoster. 7. Name the etiology of impetigo. 8. Explain why the treatment of cellulitis is important. 9. Cite examples of the classifications of fungal infections of the skin. 10. List preventive measures for decubitus ulcers. 11. Name the two most common parasitic insects to infest man. Describe how infestation can occur. 12. Name two common premalignant tumors. 13. Differentiate the three types of skin cancer. 14. Describe the guidelines for avoiding excessive sun exposure. 15. List some conditions that are caused by the abnormal development or distribution of melanocytes. 16. Name some possible causes of alopecia. 18. List some of the likely causes of deformed or discolored nails. The skin has three main structural layers (Figure 6-1). The epidermis (outer layer) is a thin, cellular, multilayered membrane that is responsible for the production of keratin and melanin. The dermis, or corium (middle layer), is a dense, fibrous layer of connective tissue that gives skin its strength and elasticity. Within the dermis are blood and lymph vessels, nerve fibers, hair follicles, and sweat and sebaceous glands. Third is the subcutaneous layer, a thick, fat-containing section that insulates the body against heat loss. Skin diseases frequently are manifested by cutaneous lesions, or alterations of the skin surface (Table 6-1). The diagnosis of a cutaneous disease often is based on the appearance of a specific type of lesion or group of lesions (Figure 6-2). TABLE 6–1 Description of Some Skin Lesions From Gould B: Pathophysiology for the health professions, ed 3, Philadelphia, 2006, Saunders. Common presenting symptoms that need attention from health care professionals include: Seborrheic dermatitis is marked by a gradual increase in the amount of, and a change in the quality of, the sebum produced by the sebaceous glands. The inflammation occurs in areas with the greatest number of sebaceous glands. These include the scalp, eyebrows, eyelids, sides of the nose, the area behind the ears, and the middle of the chest. Affected skin is reddened and covered by yellowish, greasy-appearing scales (Figure 6-3). Itching may occur but is usually mild. Seborrheic dermatitis can occur at any age, but is most common during infancy, when it is called cradle cap. Cradle cap usually clears without treatment by 8 to 12 months of age. Seborrheic dermatitis occurs at a higher rate in adults with disorders of the central nervous system, such as Parkinson’s disease. Patients who are recovering from stressful medical conditions, such as a myocardial infarction (heart attack); patients who have been confined to hospitals or nursing homes for long stays; and those who have immune system disorders, such as acquired immunodeficiency syndrome (AIDS), appear to be more prone to this disorder. More intense forms of seborrheic dermatitis can be seen in patients with psoriasis (see “Psoriasis” section). Mild forms are mainly cosmetic problems that can be easily treated or may disappear spontaneously. 692.1 (Due to oils and greases) 692.3 (Due to drugs and medicines in contact with skin) 692.4 (Due to chemical products) 692.5 (Due to food in contact with skin) 692.6 (Due to plants, except food) 692.72 (Due to solar radiation) 692.8 (Due to other specified agents) L24.0 (Irritant contact dermatitis due to detergents) L24.1 (Irritant contact dermatitis due to oils and greases) L24.2 (Irritant contact dermatitis due to solvents) L25.1 (Unspecified contact dermatitis due to drugs in contact with skin) L25.3 (Unspecified contact dermatitis due to other chemical products) L25.4 (Unspecified contact dermatitis due to food in contact with skin) L25.5 (Unspecified contact dermatitis due to plants, except food) L56.0 (Drug phototoxic response) L56.1 (Drug photoallergic response) L56.2 (Photocontact dermatitis [berloque dermatitis]) L25.8 (Unspecified contact dermatitis due to other agents) Urticaria, or hives, is associated with severe itching followed by the appearance of redness and an area of swelling (wheal) in a localized area of skin (Figure 6-7). Psoriasis is a chronic skin condition marked by thick, flaky, red patches of various sizes, covered with characteristic white, silvery scales (Figure 6-8). Psoriasis is an inflammatory chronic and recurrent skin condition with silvery scales. These scales develop into dry plaques (see Figure 6-2, C), sometimes progressing to pustules (see Figure 6-2, G). They usually do not cause discomfort but might be slightly itchy or sore. Affected skin typically appears dry, cracked, and encrusted. The most common areas in which psoriasis develops are the scalp; the outer sides of the arms and legs, especially the elbows and knees; and the trunk of the body. In addition, the palms of the hands and soles of the feet may be affected. In some patients, psoriasis spreads to the nail beds, causing the nails to thicken and crumble. Psoriasis plaques can also develop in areas of physical trauma (Koebner phenomenon). Psoriasis can occur at any age, but is more common between 10 and 30 years of age. It is noninfectious and does not affect general health. The onset of rosacea is insidious and often is mistaken for a complexion change, a sunburn, or even acne. The redness becomes more noticeable and does not go away. The skin then may begin exhibiting dryness and pimples that may become inflamed or filled with pus. In addition, small blood vessels of the cheeks and face enlarge and show through the skin as red lines even after the redness diminishes (Figure 6-9 and Figure 6-10). Small knobby bumps occasionally appear on the nose, causing it to look swollen, mostly in the male with rosacea. Acne vulgaris is marked by the appearance of papules, pustules, and comedones (see Figure 6-2, B, G, and L). Deeper, boil-like lesions called nodules sometimes can occur. Scars may develop if the chronic irritation and inflammation continue for a long period. Acne is found most often on the face but also can occur on the neck, shoulders, chest, and back (Figure 6-12). Acne can appear at any age, but is more common in adolescents. In girls, it is usually at its worst between the ages of 14 and 17 years. In boys, it reaches its peak in the late teens.
Diseases and Conditions of the Integumentary System
Orderly Functioning of The Integumentary System
Macule
Small, flat circumscribed lesion of a different color than the normal skin
Papule
Small, firm, elevated lesion
Nodule
Palpable elevated lesion; varies in size
Pustule
Elevated erythematous lesion, usually containing purulent exudate
Vesicle
Elevated, thin-walled lesion containing clear fluid (blister)
Plaque
Large, slightly elevated lesion with flat surface, often topped by scale
Crust
Dry, rough surface or dried exudate or blood
Lichenification
Thick, dry, rough surface (leatherlike)
Keloid
Raised, irregular, and increasing mass of collagen resulting from excessive scar tissue formation
Fissure
Small, deep, linear crack or tear in skin
Ulcer
Cavity with loss of tissue from the epidermis and dermis, often weeping or bleeding
Erosion
Shallow, moist cavity in epidermis
Comedo
Mass of sebum, keratin, and debris blocking the opening of a hair follicle
Dermatitis
Seborrheic Dermatitis
Symptoms and Signs
Contact Dermatitis
Description
 ICD-10-CM Code L25.9 (Unspecified contact dermatitis, unspecified cause)
ICD-10-CM Code L25.9 (Unspecified contact dermatitis, unspecified cause)
Atopic Dermatitis (Eczema)
Urticaria
Description

Psoriasis
Description
Symptoms and Signs
Rosacea
Symptoms and Signs
Acne Vulgaris
Symptoms and Signs