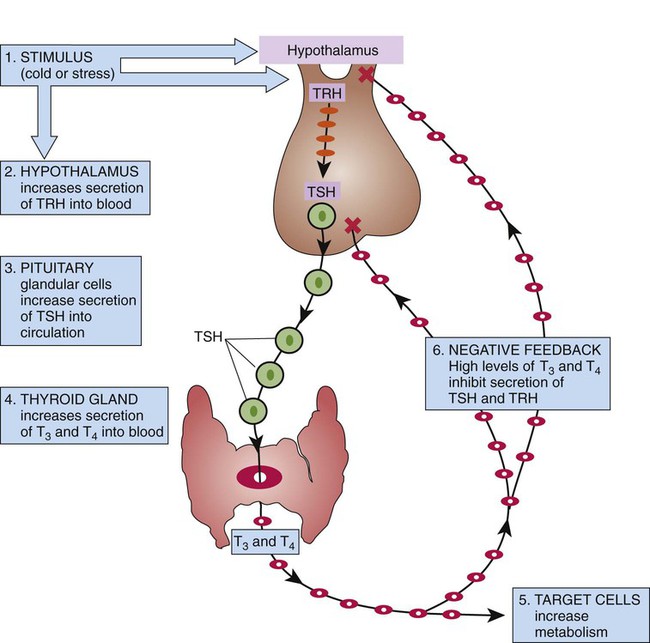
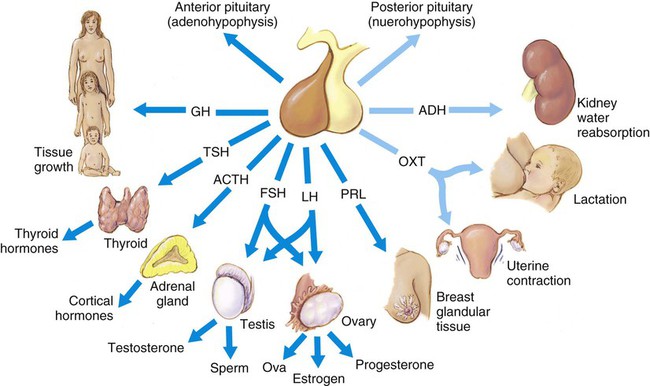
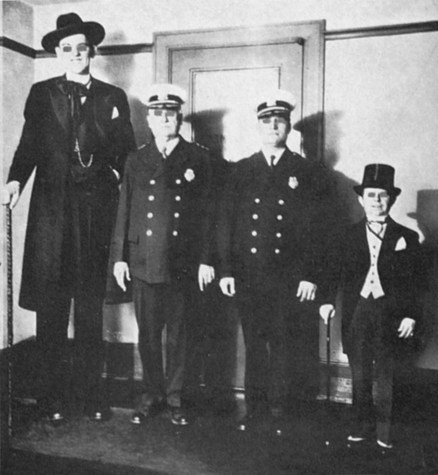
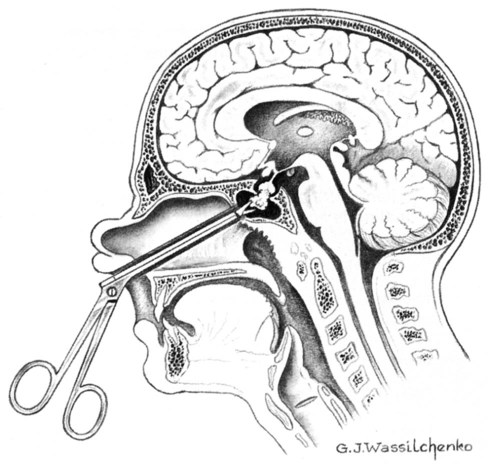
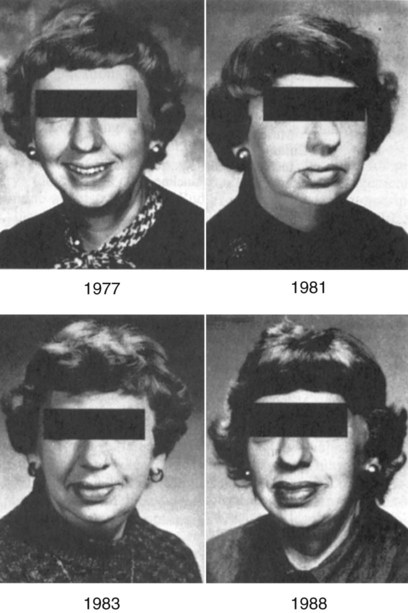
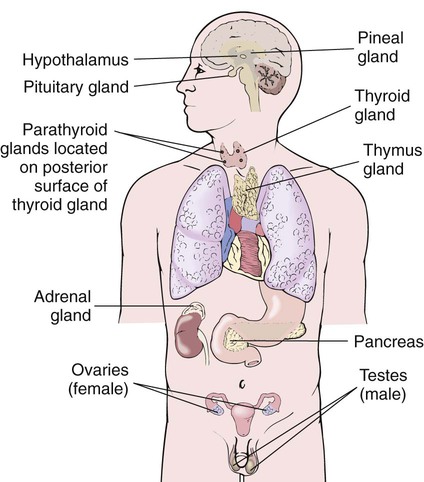
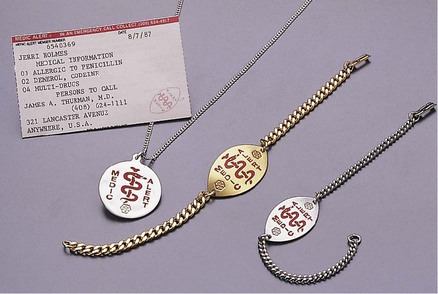
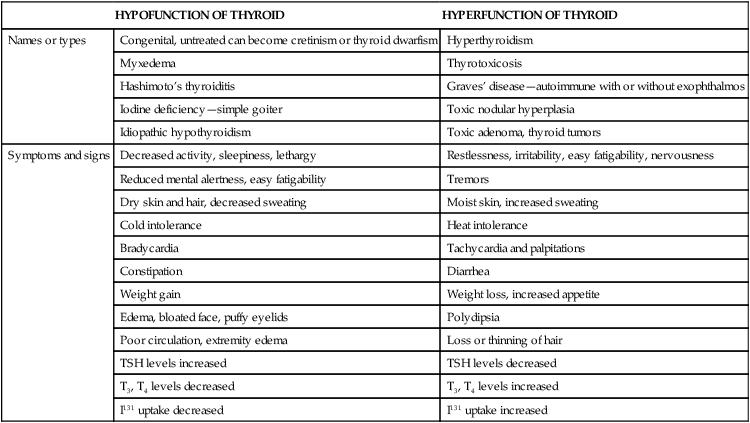
After studying Chapter 4, you should be able to: 1. List the major glands of the endocrine system. 2. Describe the importance of hormones and explain some of the critical body functions that they control. 3. Explain the importance of normal pituitary function. 4. Compare gigantism to acromegaly. 5. Describe the condition of dwarfism and its etiology. 6. Explain the cause of diabetes insipidus. 7. Explain the treatment of a simple goiter. 8. List the signs and symptoms of Graves’ disease. 9. Distinguish between cretinism and myxedema. 10. Explain the pathogenesis of diabetes mellitus. 11. Identify the two major types of diabetes mellitus. 12. Distinguish between diabetic coma and insulin shock. 13. Explain the medical management of all three types of diabetes mellitus. 14. Explain why hypoglycemia can be a serious medical condition. 15. Compare the signs and symptoms of thyroid hypofunction with those of thyroid hyperfunction. 16. Describe the signs and symptoms of thyroid malignancy. Discuss the most important prognostic factor. Body activities, homeostasis, and the response to stress are controlled by two distinct but interacting systems: the nervous system and the endocrine system. The systems interact as one system starts, ends, or extends the activity of the other. The nervous system (discussed in Chapter 13) creates an immediate but short-lived response, operating on the principles of electricity through impulse conduction. The endocrine system has a slightly slower onset and a longer duration of action, and uses highly specific and powerful hormones to control its response chemically. Hormones are chemical messengers classified as either amino acids (proteins) or steroids. The endocrine system is composed of many glands scattered throughout the body; these glands secrete unique and potent chemicals called hormones directly into the bloodstream (Figure 4-1). Most hormones direct their action to target glands or tissues at distant receptor sites, thereby regulating critical body functions, such as urinary output, cellular metabolic rate, and growth and development. Hormonal secretions typically are regulated by negative feedback; information about the hormone level or its effect is fed back to the gland, which then responds accordingly (Figure 4-2). • Emotional disturbances or psychiatric problems • Skin, hair, and nail changes • Menstrual irregularity or amenorrhea • Impotence or changes in libido To appreciate the effect of endocrine gland function on health and disease, review the main glands and their primary hormones (Table 4-1). The pituitary gland, intimately related to the hypothalamus, plays a central role in regulating most of the endocrine glands; it has a cascading effect on the glands it stimulates. The pituitary gland is divided into anterior and posterior lobes; the anterior lobe accounts for about 80% of the gland. The hypothalamus, a part of the brain that also has endocrine functions, controls many activities of the pituitary gland via neural and chemical stimuli. Pituitary dysfunction can affect some or all of the glands that are targets of pituitary hormones, thereby indirectly affecting body structure and function (Figure 4-3). TABLE 4–1 Major Endocrine Gland Secretions and Functions When the hypersecretion of GH (growth hormone, somatotropin) occurs before puberty, the result is gigantism, a proportional overgrowth of all body tissue (Figure 4-4). The child experiences abnormal and accelerated growth, especially of the long bones, because epiphyseal closure has not begun. Typically an accelerated linear growth prompts an initial investigation in children. Sexual and mental developments are often retarded. The object of treatment is to reduce the amount of GH that is secreted. This is performed ideally by surgery (transsphenoidal approach) with or without the addition of radiation to the pituitary gland to reduce its size (Figure 4-5). Appropriate gonadal hormones may be needed in children or adolescents exhibiting hypogonadism. Yearly follow-up examinations are recommended. When the hypersecretion of GH occurs after puberty, acromegaly (an overgrowth of the bones of the face, hands, and feet) occurs, with an excessive overgrowth of soft tissue because there is already epiphyseal closure (Figure 4-6). It is often seen in people 30 to 40 years old after they experience years of excess growth hormone. The patient notices that he or she must wear larger gloves, shoes, or both. The jaw grows, causing larger spaces between the teeth. He or she may experience joint pain resulting from osteoarthritis and a host of other clinical features in the body systems. The object of treatment is to reverse or prevent tumor mass effects and reduce the amount of GH secreted. Correcting the disorder prevents further disfigurement and reduces the mortality that results from production of excess growth hormone. This is performed ideally by surgery (transsphenoidal approach) with or without the addition of radiation to the pituitary gland to reduce its size (see Figure 4-5). The success of medical therapies depends on the response of tumor cells to the intervention. Hyposecretion of the pituitary gland hormones, especially GH, results in growth retardation. As a result, the child is extremely short, with a body that is small in proportion (see Figure 4-4). The prepubescent child does not develop secondary sex characteristics. The condition may be linked to other defects and a varying degree of mental retardation. Give the patient guidelines for monitoring fluid intake and output to ensure adequate water replacement. Instruct the patient to notify the physician of any increase in symptoms, including weight loss or gain. Demonstrate the procedure of checking the specific gravity of urine. Discuss the side effects or toxic effects of prescribed medications. Encourage the patient to wear a Medic Alert bracelet (Figure 4-7). Thyroid diseases present as functional disturbances that produce excessive or reduced secretions of thyroid hormones thyroxine (T4) and triiodothyronine (T3), and mass lesions of the thyroid. Table 4-2 lists types of thyroid diseases with their signs and symptoms. Fortunately, diseases of the thyroid gland may be resolved through medical and surgical intervention. TABLE 4-2 Comparison of Hypothyroid and Hyperthyroid Disorders I131, Radioactive iodine; T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone. E01.2 (Iodine-deficiency related (endemic) goiter, unspecified) (E01.0-E01.8 = 4 codes of specificity) E04.9 (Nontoxic goiter, unspecified)
Diseases and Conditions of the Endocrine System
Orderly Function of the Endocrine System
ENDOCRINE GLAND
HORMONE
TARGET ACTION
Anterior pituitary
Growth hormone (GH)
Promotes bone and tissue growth
Thyrotropin (thyroid-stimulating hormone [TSH])
Stimulates thyroid gland and production of thyroxine
Corticotropin (adrenocorticotropic hormone [ACTH])
Stimulates adrenal cortex to produce glucocorticoids
Gonadotropins
Follicle-stimulating hormone (FSH)
Initiates growth of eggs in ovaries; stimulates spermatogenesis in testes
Luteinizing hormone (LH)
Causes ovulation; stimulates ovaries to produce estrogen and progesterone; stimulates testosterone production
Prolactin
Stimulates breast development and formation of milk during pregnancy and after delivery
Melanocyte-stimulating hormone (MSH)
Regulates skin pigmentation
Posterior pituitary
Vasopressin (antidiuretic hormone [ADH])
Stimulates water resorption by renal tubules; has antidiuretic effect
Oxytocin
Stimulates uterine contractions; stimulates ejection of milk in mammary glands; causes ejection of secretions in male prostate gland
Thyroid
Thyroxine (T4) and triiodothyronine (T3)—thyroid hormone (TH)
Regulates rate of cellular metabolism (catabolic phase)
Calcitonin
Promotes retention of calcium and phosphorus in bone; opposes effect of parathyroid hormone
Parathyroid
Parathyroid hormone (parathormone, PTH)
Regulates metabolism of calcium; elevates serum calcium levels by drawing calcium from bones
Adrenal cortex
Mineralocorticoids (MC), primarily aldosterone
Promote retention of sodium by kidneys; regulate electrolyte and fluid homeostasis
Glucocorticoids (GC): cortisol, corticosterone, cortisone
Regulate metabolism of carbohydrates, proteins, and fats in cells
Gonadocorticoids: androgens, estrogens, progestins
Govern secondary sex characteristics and masculinization
Adrenal medulla
Catecholamines: epinephrine and norepinephrine
Produce quick-acting “fight or flight” response during stress; increase blood pressure, heart rate, and blood glucose level; dilate bronchioles
Pancreas
Insulin
Regulates metabolism of glucose in body cells; maintains proper blood glucose level
Glucagon
Increases concentration of glucose in blood by causing conversion of glycogen to glucose
Ovaries
Estrogens
Cause development of female secondary sex characteristics
Progesterone
Prepares and maintains endometrium for implantation and pregnancy
Testes
Testosterone
Stimulates and promotes growth of male secondary sex characteristics and is essential for erections
Thymus
Thymosin
Promotes development of immune cells (gland atrophies during adulthood)
Pineal gland
Melatonin
Regulates daily patterns of sleep and wakefulness. Inhibits hormones that affect ovaries; other functions unknown
Pituitary Gland Diseases
Hyperpituitarism
Gigantism
Symptoms and Signs
Treatment
Acromegaly
Symptoms and Signs
Treatment
Dwarfism
Symptoms and Signs
Diabetes Insipidus
Patient Teaching
Thyroid Gland Diseases
HYPOFUNCTION OF THYROID
HYPERFUNCTION OF THYROID
Names or types
Congenital, untreated can become cretinism or thyroid dwarfism
Hyperthyroidism
Myxedema
Thyrotoxicosis
Hashimoto’s thyroiditis
Graves’ disease—autoimmune with or without exophthalmos
Iodine deficiency—simple goiter
Toxic nodular hyperplasia
Idiopathic hypothyroidism
Toxic adenoma, thyroid tumors
Symptoms and signs
Decreased activity, sleepiness, lethargy
Restlessness, irritability, easy fatigability, nervousness
Reduced mental alertness, easy fatigability
Tremors
Dry skin and hair, decreased sweating
Moist skin, increased sweating
Cold intolerance
Heat intolerance
Bradycardia
Tachycardia and palpitations
Constipation
Diarrhea
Weight gain
Weight loss, increased appetite
Edema, bloated face, puffy eyelids
Polydipsia
Poor circulation, extremity edema
Loss or thinning of hair
TSH levels increased
TSH levels decreased
T3, T4 levels decreased
T3, T4 levels increased
I131 uptake decreased
I131 uptake increased
Simple Goiter
Description
 ICD-9-CM Code 240.0 Goiter (specified as simple)
ICD-9-CM Code 240.0 Goiter (specified as simple)
 ICD-10-CM Code E04.0 (Nontoxic diffuse goiter)
ICD-10-CM Code E04.0 (Nontoxic diffuse goiter)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree