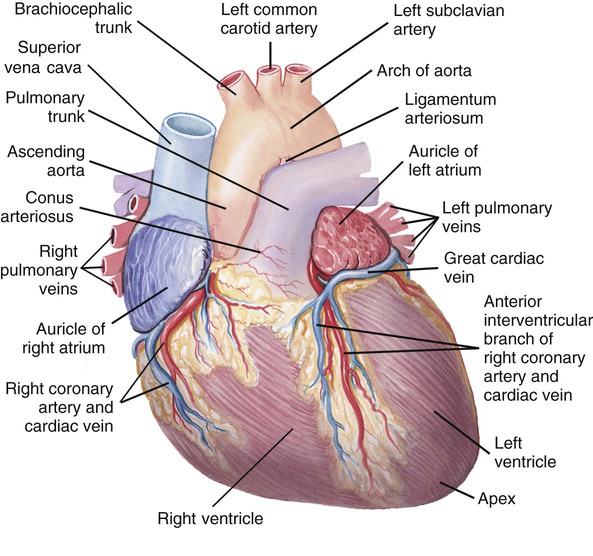
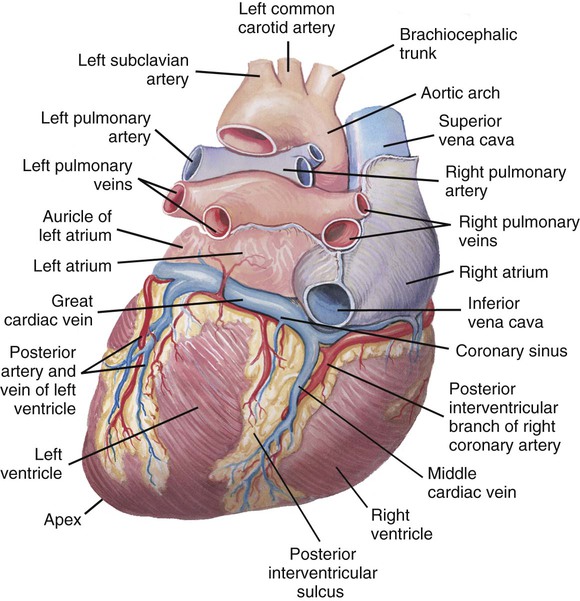
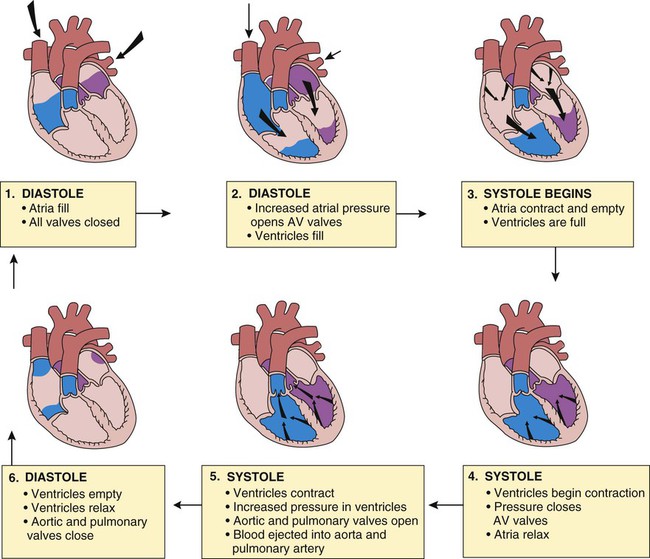
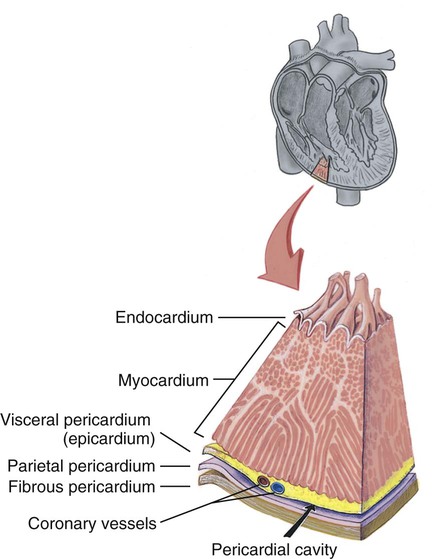
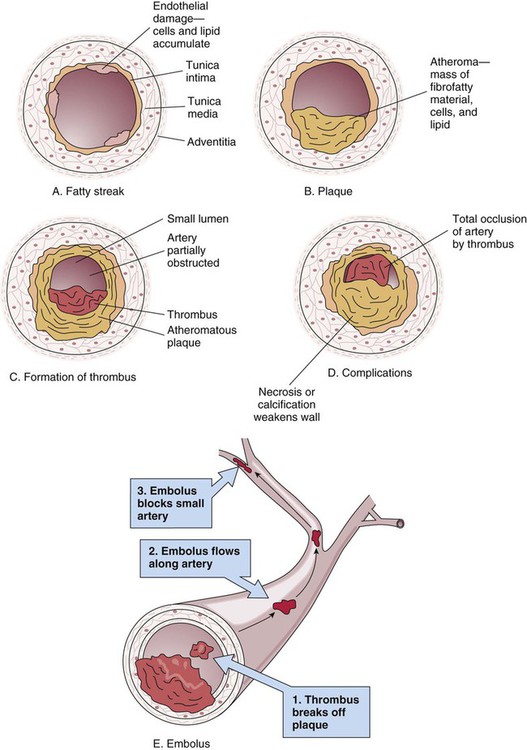
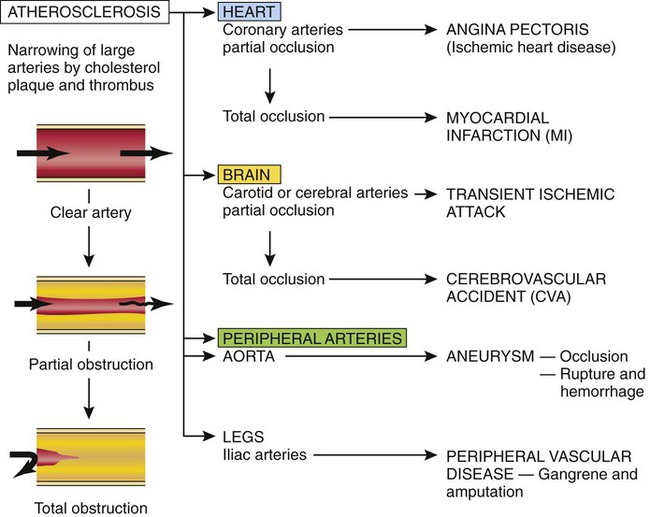
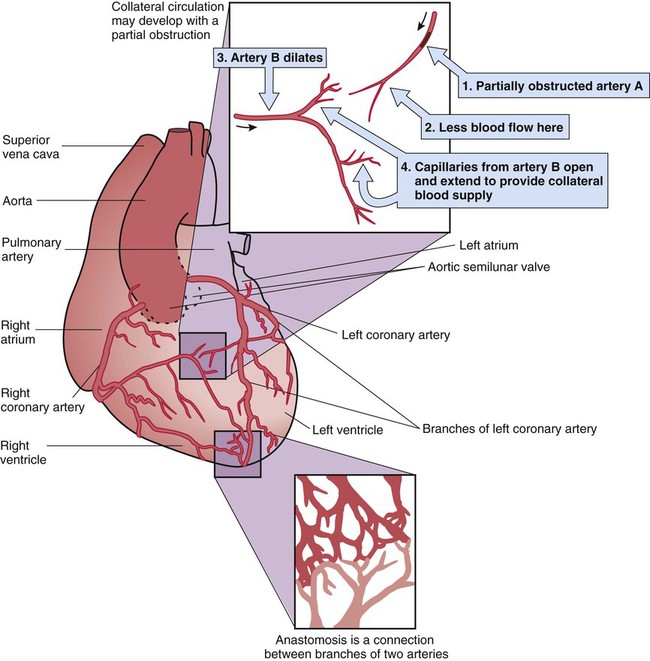
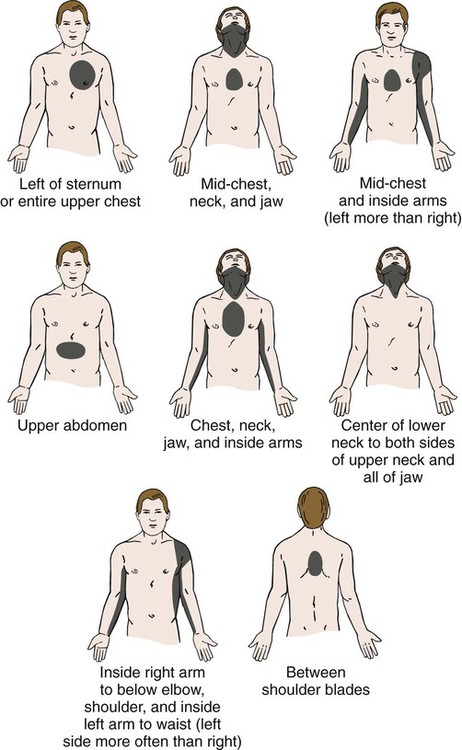
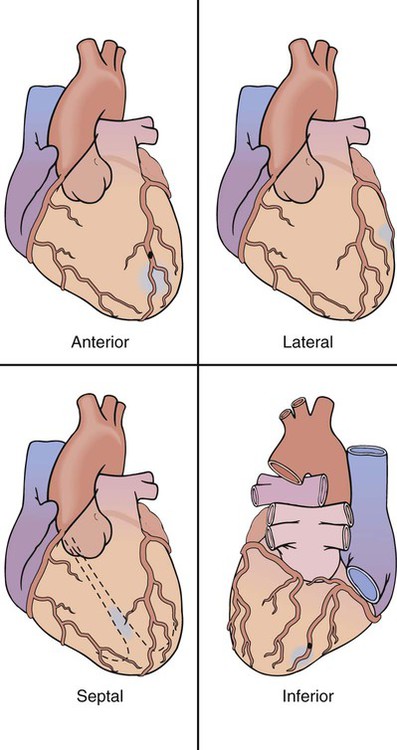
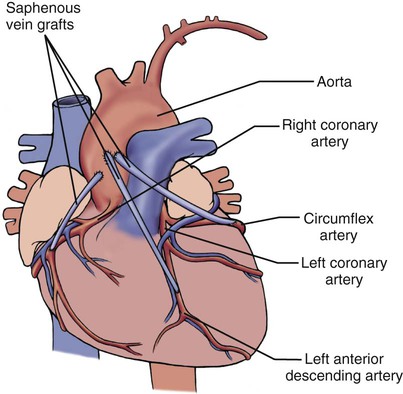
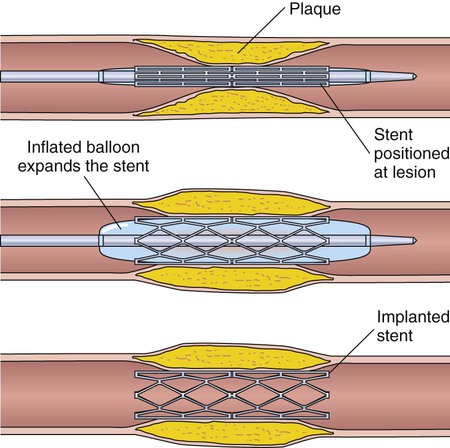
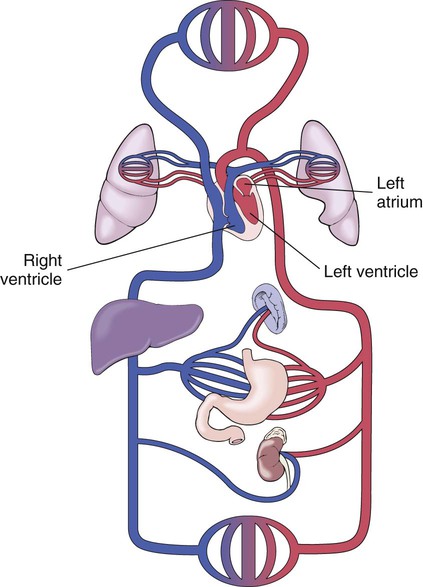
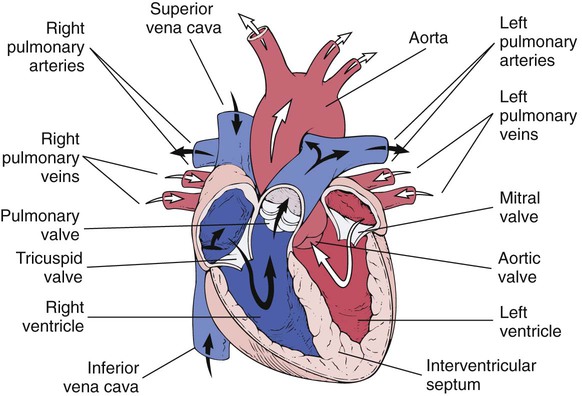
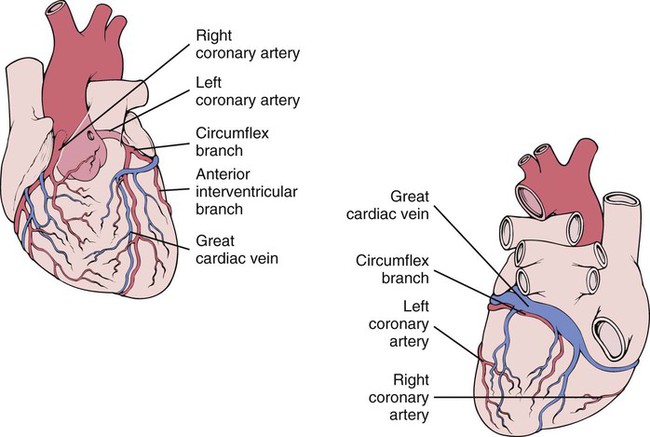
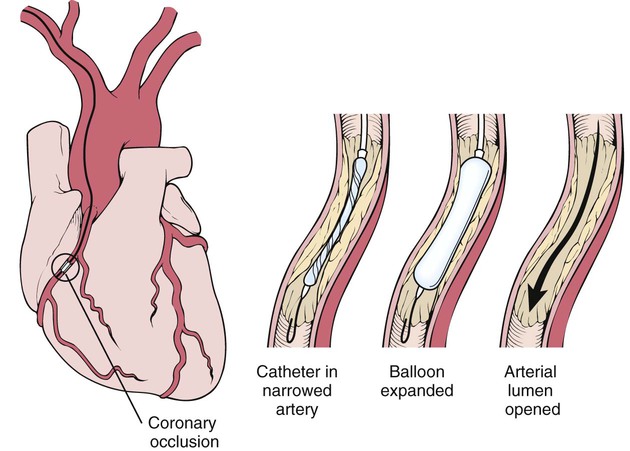
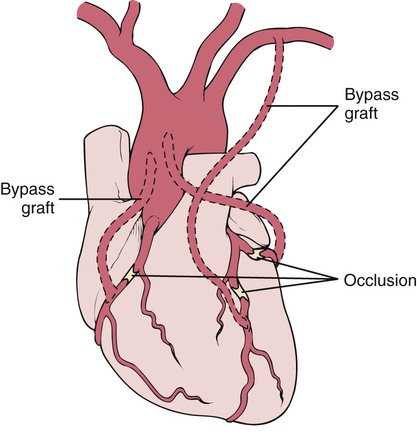
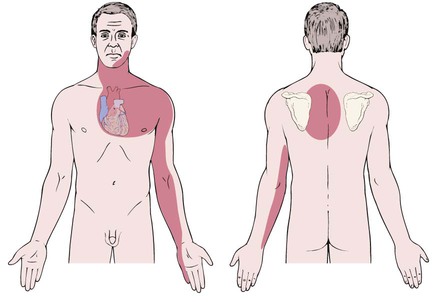
After studying Chapter 10, you should be able to: 1. Name the common presenting symptoms in patients with cardiovascular disease. 2. Describe the pathology of coronary artery disease. 3. Name the contributing factors for coronary heart disease. 4. Explain what causes the pain of angina pectoris. 5. Explain the difference between myocardial infarction and angina pectoris. 6. Describe the treatment of myocardial infarction. 7. Name and describe the symptoms of the most prevalent cardiovascular disorder in the United States. 8. Explain what happens when the pumping action of the heart fails. 9. Compare right-sided heart failure with left-sided heart failure. 10. Name some causes of cardiomyopathy. 11. Distinguish among pericarditis, myocarditis, and endocarditis. 12. Explain why rheumatic fever is considered a systemic disease. 13. Recall the cardiac manifestations of rheumatic heart disease. 14. Explain the pathophysiology of valvular heart disease. 15. Name the causes of cardiac arrhythmias. 16. Discuss treatment options for cardiac arrhythmias. 17. Describe the signs and symptoms of shock. 18. Explain the possible consequences of emboli. 19. Compare arteriosclerosis with atherosclerosis. 20. Describe an aneurysm and explain how it is diagnosed. 21. Explain the treatment for (a) thrombophlebitis and (b) varicose veins. 22. Describe the vascular pathology of Raynaud’s disease. 23. Define anemia and list the presenting symptoms. 24. Describe how anemias are classified and give some examples. 25. State the causes of agranulocytosis. 26. Describe the typical symptoms in all types of leukemias. 27. Distinguish between lymphedema and lymphangitis. 28. Explain the diagnostic significance of Reed-Sternberg cells in lymphoma. 29. Name the signs and symptoms of transfusion incompatibility reaction. Circulation of blood to the organs and tissues of the body is the primary function of the circulatory system. The heart is at the center of the circulatory system (Figures 10-1 and 10-2). Its steady beating pumps about 5 quarts of blood through a complete vascular circuit of the body every minute in an adult; this is called the cardiac cycle. This circuit comprises a network of vessels: the arteries, veins, and capillaries (Figure 10-3). The heart consists of two side-by-side pumps, each divided into two chambers: two upper chambers called atria, and two lower chambers called ventricles. As venous blood returns to the heart from the body, it enters the right atrium, passes through the tricuspid valve, and with atrial contraction, enters the right ventricle. Heart valves prevent the blood from flowing backward. From the right ventricle, blood is pumped through the pulmonary valve and, with ventricular contraction, into the pulmonary arteries and on to the lungs. In the lungs, carbon dioxide is removed and oxygen is added to the blood. Freshly oxygenated blood then returns to the heart via the pulmonary veins. It enters the left atrium, moves through the mitral (bicuspid) valve with atrial contraction, and enters the left ventricle. As the left ventricle contracts, the blood is forced through the aortic valve, into the aorta, and on to the rest of the body (Figures 10-3 and 10-4). This process is called the cardiac cycle (Figure 10-5). The heart is enclosed by the double-layered pericardium, which is composed of an inner serous layer (visceral pericardium or epicardium) and an outer fibrous layer (parietal pericardium). Between these layers in the pericardial cavity is a small amount of serous fluid that reduces friction during cardiac movements. Cardiac muscle tissue or myocardium is composed of striated muscle cells that can contract rhythmically on their own and characteristically are both voluntary and involuntary responses. Inside the cavities of the heart is a smooth serous lining called the endocardium (Figure 10-6). The conduction system of the heart coordinates the contraction and relaxation (cardiac cycle) of the heart by initiating impulses and distributing the impulses throughout the myocardium (see Figure 10-34). Coronary arteries and a network of vessels continuously supply cardiac muscle tissue with oxygen (Figure 10-7). Coronary artery disease (CAD) is a condition involving the arteries supplying the myocardium (heart muscle) (see Figure 10-7). The arteries become narrowed by atherosclerotic deposits over time, causing temporary cardiac ischemia and eventually MI (myocardial infarction, or heart attack). Patients are asymptomatic initially, with the first symptom being the pain of angina pectoris (see “Angina Pectoris” section). In advanced disease, the severe pain of MI is described as burning, squeezing, crushing, and radiating to the arm, neck, or jaw (see “Myocardial Infarction” section) and is due to diminished blood flow and lower oxygen saturation. Nausea, vomiting, and weakness also can be experienced. Changes in the electrocardiogram (ECG) are often but not always recognized. Many patients may be asymptomatic up until an MI or sudden death event; this is why noninvasive screening of high-risk patients is imperative. Deposits of fat-containing substances called plaque in the lumen (opening) of the coronary arteries result in atherosclerosis and subsequent narrowing of the lumen of the arteries (Figure 10-8). The myocardium must have an adequate blood supply to function. The coronary arteries supply the cardiac muscle with blood but become constricted by atherosclerosis (Figure 10-9). The patient usually does not experience chest pain from atherosclerosis until the coronary arteries are about 75% occluded. Collateral circulation often develops to supply the tissue with needed oxygen and nutrients (Figure 10-10). An ECG shows ischemia (caused by a lack of blood supply) and possibly arrhythmias. Treadmill testing, thallium or Cardiolite scan, CT scans, stress echocardiograms, cardiac catheterization, E10-1, and angiograms are other tools of cardiac status evaluation used to detect insufficient oxygen supply and to confirm the diagnosis. Electron beam computerized testing, a noninvasive assessment identifying calcium buildup in arteries, is another means of risk evaluation. Treatment consists of measures to restore adequate blood flow to the myocardium. Vasodilators and other types of medicines are prescribed. Angioplasty with a balloon or stenting is attempted in some instances to open the constricted arteries (Figure 10-11). Claims of reduction of the plaque buildup with hypolipidemic drugs are being confirmed in some cases. First line drug therapy for the prevention of CAD may include angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), thiazide diuretics, or vasodilators. Beta-blockers and anticoagulants are used to prevent blood clots from breaking off and lodging in cerebral arteries. When the blockage is severe or does not respond to drug therapy or angioplasty, coronary artery bypass surgery may be indicated to restore circulation to the affected myocardium (Figure 10-12). The patient has a sudden onset of left-sided chest pain during or shortly after exertion. The pain may radiate to the left arm or back (Figure 10-13). The patient also may experience dyspnea. The pain usually is relieved by ceasing the strenuous activity and placing nitroglycerin tablets sublingually or using nitroglycerin spray also sublingually (under the tongue). The blood pressure may increase during the attack, and arrhythmias may occur. Myocardial infarction is death of myocardial tissue caused by the development of ischemia. 410.1 (Of other anterior wall) 410.3 (Of inferoposterior wall) 410.4 (Of other inferior wall) 410.6 (True posterior wall infarction) 410.7 (Subendocardial infarction) 410.8 (Of other specified sites) I21.09 (ST elevation [STEMI] myocardial infarction involving other coronary artery of anterior wall) I21.19 (ST elevation [STEMI] myocardial infarction involving other coronary artery of inferior wall) I21.11 (ST elevation [STEMI] myocardial infarction involving right coronary artery) I21.19 (ST elevation [STEMI] myocardial infarction involving other coronary artery of inferior wall) I21.29 (ST elevation [STEMI] myocardial infarction involving other sites) I21.4 (Non-ST elevation [NSTEM] myocardial infarction) I21.29 (ST elevation [STEMI] myocardial infarction involving other sites) I21.3 (ST elevation [STEMI] myocardial infarction of unspecified site) An occlusion of a coronary artery resulting in ischemia and infarct (death) of the myocardium causes sudden, severe substernal or left-sided chest pain (Figure 10-14). The pain may be crushing, causing a feeling of massive constriction of the chest, may be burning, or may just be a vague discomfort. This pain may radiate to the left or right arm, back, or jaw and is not relieved by rest or the administration of nitroglycerin. Irregular heartbeat, dyspnea, and diaphoresis often accompany the pain, and the patient usually exhibits denial and experiences severe anxiety, sometimes with the feeling of impending doom (Figure 10-15). MI occasionally is clinically silent, especially in diabetics. Myocardial infarction (MI) results from insufficient oxygen supply, such as occurs when a coronary artery is occluded by atherosclerotic plaque, thrombus, or myocardial muscle spasm (Figure 10-16). The pain is caused by ischemia, and if ischemia is not reversed within about 6 hours, the cardiac muscle dies. Coronary thrombosis is the most common cause of MI. Oxygen is administered, and morphine is given for pain. Aspirin is given as soon as possible to reduce the risk of additional damage to the heart and tissue by ischemia. Vasodilation is attempted by nitroglycerin drip. Lidocaine or amiodarone given by an intravenous drip, after a loading bolus, helps to control arrhythmias. Thrombolytic drugs, including tissue plasminogen activator (TPA), streptokinase, or alteplase (Activase) may be administered as soon as possible after the diagnosis, unless there are contraindications. Within the 6-hour window before permanent damage, an attempt may be made to open the occlusion and to restore blood flow to the area by angioplasty (see Figure 10-11), the administration of thrombolytic drugs, or by coronary artery bypass surgery (Figure 10-17). Currently, the standard of care is to try to emergently open the artery with a stent (Figure 10-18), preferably within 60 to 90 minutes of arrival; this has been demonstrated to more effectively decrease heart damage than IV thrombolytic drugs. E10-2 Cardiac arrest is a true life-threatening emergency. Immediate intervention with instantaneous initiation of CPR and defibrillation by means of an automated external defibrillator (AED) may successfully restore contraction of the heart (Figure 10-19). The American Heart Association or American Red Cross protocol for caregivers in the field requires immediate contact of the emergency medical system by calling 911. Inpatient facilities use the “Code, Dr. Blue” message to alert personnel. Cardiopulmonary resuscitation (CPR) must be instituted within 4 to 6 minutes of the cardiac arrest. Until recently, cardiac defibrillation was only attempted by trained, advanced life-support personnel. AEDs are now available for use by anyone who observes a cardiac arrest. The latest technology implemented in these devices talks the rescuer through the defibrillation process (see Figure 10-19). The rescuer should be familiar with the device he/she is attempting to use. Cardiac drugs are administered, including epinephrine (Adrenalin) and isoproterenol (Isuprel) or dobutamine to stimulate the heart. Antiarrhythmic drugs, including lidocaine and amiodarone, also may be administered.
Diseases and Conditions of the Circulatory System
Orderly Function of the Circulatory System
Coronary Artery Disease
Description
Symptoms and Signs
Etiology
Diagnosis
Treatment
Angina Pectoris
Symptoms and Signs
Myocardial Infarction
Description
 ICD-9-CM Code 410 (Acute myocardial infarction)
ICD-9-CM Code 410 (Acute myocardial infarction)
 ICD-10-CM Code I21.0 (5th digit required) (ST elevation (STEMI) myocardial infarction of anterior wall)
ICD-10-CM Code I21.0 (5th digit required) (ST elevation (STEMI) myocardial infarction of anterior wall)
Symptoms and Signs
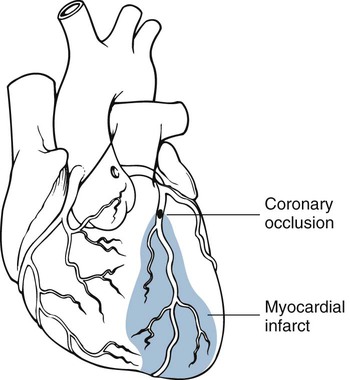
Etiology
Treatment
Cardiac Arrest
Patient Screening
Treatment