Diffuse Large B-cell Lymphoma, NOS, Immunoblastic
Francisco Vega, MD, PhD
Key Facts
Terminology
Diffuse proliferation of large neoplastic B cells with immunoblastic cytologic features
Immunoblasts must be > 90% of all cells
DLBCL-IB variant superseded by specific types of DLBCL as defined in WHO classification
Clinical Issues
Some studies identified immunoblastic variant as being more clinically aggressive than centroblastic variant
Stage IV in at least 1/3 of cases
Bone marrow involvement less frequent than low-grade B-cell lymphomas
Microscopic Pathology
Diffuse growth pattern
Composed predominantly of immunoblasts
Express pan-B cell markers
Ancillary Tests
2 major molecular groups
GC type
ABC type
Top Differential Diagnoses
DLBCL, centroblastic variant
DLBCL, anaplastic variant
Plasmablastic lymphoma
Primary cutaneous DLBCL, leg type
ALK(+) large B-cell lymphoma
B-cell lymphoma, unclassifiable, with features between DLBCL and Burkitt lymphoma
TERMINOLOGY
Abbreviations
Diffuse large B-cell lymphoma, immunoblastic variant (DLBCL-IB)
Synonyms
Immunoblastic lymphoma
Immunoblastic sarcoma
Definitions
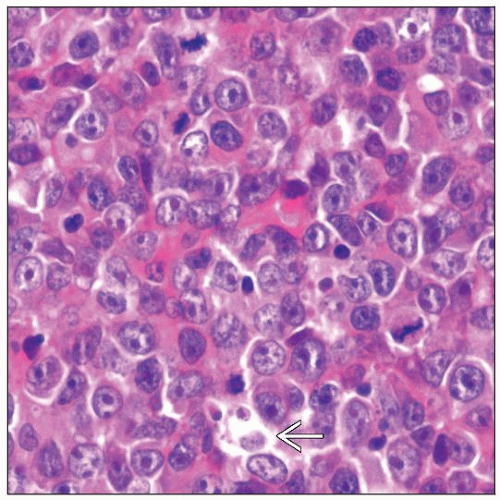
Diffuse proliferation of large neoplastic B cells with immunoblastic cytologic features
By definition, immunoblasts must be > 90% of all cells
Immunoblast
Large lymphocyte with centrally located nucleolus and moderate basophilic cytoplasm
DLBCL-IB variant superseded by specific types of DLBCL as defined in WHO classification
CLINICAL ISSUES
Epidemiology
Incidence
Predominantly disease of older adults
Children and young adults can be affected
Presentation
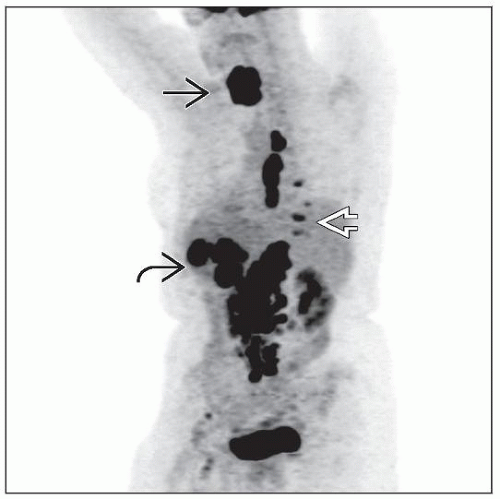
Enlarging mass in nodal or extranodal sites
Gastrointestinal tract is frequent extranodal site
˜ 1/3 of patients have stage IV disease
Bone marrow involvement less frequent than in patients with low-grade B-cell lymphomas
Frequent B symptoms (fever, night sweats, or weight loss)
Treatment
R-CHOP regimen (rituximab + cyclophosphamide, doxorubicin, vincristine, and prednisone)
Prognosis
Some studies have identified immunoblastic variant as being clinically more aggressive than centroblastic variant
5-year overall survival for patients with DLBCL ranges from 25-75% depending on prognostic factors present at diagnosis
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse growth pattern
Irrespective of location, DLBCL-IB diffusely replaces normal architecture
Immunoblastic morphology
Plasmacytoid differentiation is common
ANCILLARY TESTS
Immunohistochemistry
Pan-B cell antigens(+)
CD20 can be dim, attributable to plasmacytoid differentiation
CD10(+), Bcl-6(+), LM02(+), HGAL(+) in subset
MUM1(+) in cases with plasmacytoid differentiation
FoxP1(+/-), Bcl-2(+/-), CD30(-/+), and usually weak and partial
Proliferation fraction (Ki-67) is usually high
Algorithms proposed to identify GC and non-GC types
Hans et al
Choi et al
DIFFERENTIAL DIAGNOSIS
DLBCL, Centroblastic Variant
Centroblastic and immunoblastic variants can be difficult to distinguish reliably
Justifies their inclusion into DLBCL as variants
By definition, at least a significant number (> 10%) of neoplastic cells are centroblasts
Subtle morphologic features supporting centroblastic variant
2-3 nucleoli with 1 central and 1-2 apposed to nuclear membrane
Absence of plasmacytoid differentiation
Presence of small and large cleaved cells
Residual follicular pattern
DLBCL, Anaplastic Variant
Large neoplastic cells with bizarre morphology; may resemble Hodgkin &/or Reed-Sternberg cells
These neoplasms may have intrasinusoidal growth pattern
CD30 often positive
Plasmablastic Lymphoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree