Diagnostic Cytology: Its Origins and Principles
EARLY EVENTS: THE BIRTH OF MICROSCOPY AND CLINICAL CYTOLOGY
Diagnostic cytology is the culmination of several centuries of observations and research. Although it is beyond the scope of this overview to give a detailed account of the past events, the readers may find a brief summary of these developments of interest.
Although some cells can be seen with the naked eye, for example, birds’ or reptiles’ eggs, it was the invention of the microscope that led to the recognition that all living matter is composed of cells. The term microscope was proposed in 1624 by an Italian group of scientists, united at the Academia dei Licei in Florence. The group, among others, included the great astronomer, Galileo, who apparently was also a user of one of the first instruments of this kind (Purtle, 1974). The first microscopes of practical value were constructed in Italy and in Holland in the 17th century. The best instrument, constructed by the Dutchman, Anthony van Leeuwenhoek (1632-1723) allowed a magnification of × 275. Leeuwenhoek reported on the miraculous world of microscopy in a series of letters to the Royal Society in London. His observations ranged from bacteria to spermatozoa. Interested readers will find illustrations of Leeuwenhoek’s work and further comments on him and his contemporaries in the excellent book entitled History of Clinical Cytology by Grunze and Spriggs (1983). For nearly 2 centuries thereafter, these instruments were costly, very difficult to use and, therefore, accessible only to a very small, wealthy elite of interested scientists, most of whom were amateurs dabbling with microscopy as a diversion. Many of these microscopes were works of art (Fig. 1-1). Using one of these microscopes with a focusing adjustment, the Secretary of the Royal College in London, Robert Hooke, observed, in 1665, that corks and sponges were composed of little boxes that he called cells (from Latin, cellula = chamber) but the significance of this observation did not become apparent for almost 200 years. The great 17th century Italian anatomist, Malpighi, was also familiar with the microscope and is justly considered the creator of histology. The event that, in my judgment, proved to be decisive in better understanding of
cell and tissue structure in health and disease was the invention of achromatic lenses that allowed an undistorted view of microscopic images. In the 1820s, the construction of compound microscopes provided with such optics occurred nearly simultaneously in London (by Lister, the father of Lord Lister, the proponent of surgical antisepsis) and in Paris (by the family of opticians and microscope makers, named Chevalier). These microscopes, with many subsequent improvements, were easy to use, could be mass-produced at a reasonable price, and thus became available to a great many interested professional investigators, leading to a better understanding of cell structure and, indirectly, to an insight into the mechanisms of cell function and, hence, of life processes. Although, even in the age of molecular biology, much remains to be discovered about the interplay of molecules leading to cell differentiation and function, some progress has been made (see Chaps. 3 and 7) and more can be expected in the years to come.
cell and tissue structure in health and disease was the invention of achromatic lenses that allowed an undistorted view of microscopic images. In the 1820s, the construction of compound microscopes provided with such optics occurred nearly simultaneously in London (by Lister, the father of Lord Lister, the proponent of surgical antisepsis) and in Paris (by the family of opticians and microscope makers, named Chevalier). These microscopes, with many subsequent improvements, were easy to use, could be mass-produced at a reasonable price, and thus became available to a great many interested professional investigators, leading to a better understanding of cell structure and, indirectly, to an insight into the mechanisms of cell function and, hence, of life processes. Although, even in the age of molecular biology, much remains to be discovered about the interplay of molecules leading to cell differentiation and function, some progress has been made (see Chaps. 3 and 7) and more can be expected in the years to come.
 Figure 1-1 Two beautiful 17th century microscopes. (Courtesy of the Billing’s Collection, Armed Forces Institute of Pathology, Washington, DC.) |
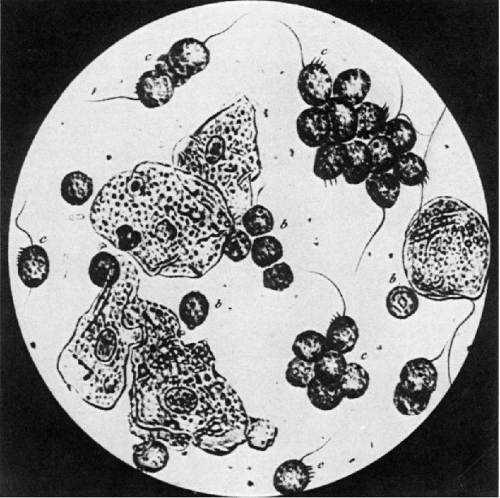
Nearly all the microscopic observations during the first half of the 19th century were conducted on cells because the techniques of tissue processing for microscopic examination were very primitive. Early on, the investigators observed that animal cells from different organs varied in size and shape and that some were provided with specialized structures, such as cilia. Perhaps the most remarkable record of these observations was an atlas of microscopic images by a French microscopist, André François Donné, published in Paris in 1845. The atlas was the first book illustrated with actual photomicrographs of remarkable quality (Fig. 1-2), obtained by the newly described method of Daguerre. The observations by many early observers led to the classification of normal cells and, subsequently, tissues as the backbone of normal cytology and histology. In the middle of the 19th century, the pioneering German pathologist, Rudolf Virchow, postulated that each cell is derived from another cell (omnis cellula a cellula). This assumption, which repeatedly has been proved to be correct, implies that at some time in a very distant past, probably many million years ago, the first cell, the mother of all cells, came to exist. How this happened is not known and is the subject of ongoing investigations.
By the middle of the 19th century, several books on the use of the microscope in medicine became available. In the book, The Microscope in its Applications to Practical Medicine,
that appeared in two editions (1854 and 1858), Lionel Beale of London described the cells as follows: “A cell consists of a perfectly closed sac containing certain contents. The most important structure within the cell wall, in most instances, is the nucleus, upon which the multiplication of the cell … (and other functions) … depend. It must be borne in mind, however, that in some cells, such as the human blood corpuscles (erythrocytes, comment by LGK) a nucleus is not to be demonstrated. Within the nucleus there usually exists … a clear bright spot. This is the nucleolus.” Beale further classified cells into several categories according to their shapes (scaly or squamous cells, tesselated cells [epithelial cells lining serous membranes, LGK], polygonal cells, columnar cells, spherical cells, spindle-shaped cells, fusiform cells, etc.), thus describing the entire spectrum of cell configuration. He further described cells derived from various organs (including the central nervous system) and reported that some cells were ciliated, notably those of the trachea, bronchus, fallopian tubes and portions of the endocervical canal. Beale also reported that “some cells have a remarkable power of multiplication … distinguished for the distinctness and number of its nuclei” (cancer cells). Beale described the use of the microscope to identify cancer of various organs that he could distinguish from a benign change of a similar clinical appearance. It is evident, therefore, that by the middle of the 19th century, approximately 150 years ago, there was considerable knowledge of the microscopic configuration of human cells and their role in the diagnosis of human disease.
that appeared in two editions (1854 and 1858), Lionel Beale of London described the cells as follows: “A cell consists of a perfectly closed sac containing certain contents. The most important structure within the cell wall, in most instances, is the nucleus, upon which the multiplication of the cell … (and other functions) … depend. It must be borne in mind, however, that in some cells, such as the human blood corpuscles (erythrocytes, comment by LGK) a nucleus is not to be demonstrated. Within the nucleus there usually exists … a clear bright spot. This is the nucleolus.” Beale further classified cells into several categories according to their shapes (scaly or squamous cells, tesselated cells [epithelial cells lining serous membranes, LGK], polygonal cells, columnar cells, spherical cells, spindle-shaped cells, fusiform cells, etc.), thus describing the entire spectrum of cell configuration. He further described cells derived from various organs (including the central nervous system) and reported that some cells were ciliated, notably those of the trachea, bronchus, fallopian tubes and portions of the endocervical canal. Beale also reported that “some cells have a remarkable power of multiplication … distinguished for the distinctness and number of its nuclei” (cancer cells). Beale described the use of the microscope to identify cancer of various organs that he could distinguish from a benign change of a similar clinical appearance. It is evident, therefore, that by the middle of the 19th century, approximately 150 years ago, there was considerable knowledge of the microscopic configuration of human cells and their role in the diagnosis of human disease.
Perhaps the most important series of observations pertinent to this narrative was the recognition that cells obtained from clinically evident cancerous growths differed from normal cells. The initial observations on cancer cells is attributed to a young German physiologist, Johannes Müller, who, in 1838, published an illustrated monograph entitled On the Nature and Structural Characteristics of Cancer and Those Morbid Growth That Can Be Confounded With It. In this monograph, Müller discussed at some length the differences in configuration of cells and their nuclei in cancer when compared with normal cells. Müller’s original observations on the differences between normal and cancerous cells were confirmed by several investigators. For example, in 1860, Beale identified and described cancer cells in sputum. It may come as a surprise to some of the readers that as early as 1845 and 1851, a German microscopist, working in Switzerland and writing in French, Hermann Lebert, used cell samples aspirated from patients by means of a cannula for the diagnosis of cancer. In 1847, M. Kün of Strasbourg, about whom little is known, described a needle with a cutting edge useful in securing material from subcutaneous tumors, examined as smears (Grunze and Spriggs, 1983; Webb, 2001).
Virchow, often considered the father of contemporary pathology, and who was Müller’s pupil, was a superb observer at the autopsy table and a good microscopist. He recognized and described the gross and microscopic features of a large number of entities, such as infarcts, inflammatory lesions, leukemia, and various forms of cancer. However, his views on the origin of human cancer were erroneous because he believed that all cancers were derived from connective tissue and not by transformation of normal tissues (Virchow, 1863). For this reason, he had difficulties in accepting the observations of two of his students and contemporaries, Thiersch in 1865 and Waldayer in 1867, who independently advocated the origin of carcinomas of the skin, breast, and uterus from transformed normal epithelium. Because Virchow wielded a tremendous influence in Germany, not only as a scientist but also as a politician (he was a Professor of Pathology in Berlin as well as a Deputy to the German Parliament, a socialist of sorts, who fought with the famous Chancellor, Bismarck), views that were in conflict with his own were often rejected, thus delaying the development of independent scientific thought. It took about 40 years until the confirmation of Thiersch’s and Waldayer’s concepts of the origin of carcinomas was documented by Schauenstein for the uterine cervix in 1908 (see Chap. 11). It took many more years until the concept of a preinvasive stage of invasive cancer, originally designated as carcinoma in situ by Schottlander and Kermauner in 1912, was generally accepted and put to a good clinical use in cancer detection and prevention.
These are but a few of the early contributions that have bearing on diagnostic cytology as it is known today. In addition to the contributors mentioned by name, there were many other heroes and antiheroes who made remarkable contributions to the science of human cytology during the second half of the 19th century, and this brief narrative doesn’t do justice to them. The interested reader should consult a beautifully illustrated book on the history of clinical cytology by Grunze and Spriggs (1983).
Still, in spite of these remarkable developments, the widespread application of cytology to the diagnosis of human disease did not take place until the 1950s. Although
sporadic publications during the second half of the 19th century and the first half of the 20th century kept the idea of cytologic diagnosis alive, it was overshadowed by developments in histopathology.
sporadic publications during the second half of the 19th century and the first half of the 20th century kept the idea of cytologic diagnosis alive, it was overshadowed by developments in histopathology.
THE ERA OF HISTOPATHOLOGY
The Beginning
Although cells teased from tissues were the main target of microscopic investigations during the first half of the 19th century, consistent efforts have been made to develop methods of tissue processing. Thus, in the 1858 edition of Beale’s book, several pages are dedicated to the methods of hardening soft tissue samples by boiling and to the methods of preparation of transparent, thin sections suitable for microscopic examination with hand-held cutting instruments. Subsequently, various methods of tissue fixation were tried, such as chromium salts, alcohol, and ultimately, formalin and the manual cutting instruments were replaced by mechanical microtomes around 1880. Simultaneously, many methods of tissue staining were developed. There is excellent evidence that, by 1885, tissue embedding in wax or paraffin, cutting of sections with a microtome, and staining with hematoxylin and eosin were the standard methods in laboratories of pathology, as narrated in the history of surgical pathology at the Memorial Hospital for Cancer, now known as the Memorial Sloan-Kettering Cancer Center (Koss and Lieberman, 1997).
Two events enhanced the significance and value of tissue pathology. One was the introduction of the concept of a tissue biopsy, initially proposed for diagnosis of cancer of the uterine cervix and endometrium by Ruge and Veit in 1877, who documented that the microscope is superior to clinical judgment in the diagnosis of these diseases. However, the term biopsy is attributable to a French dermatopathologist, Ernest Besnier, who coined it in 1879 (Nezelof, 2000). The second event was the introduction of frozen sections, popularized by Cullen in 1895, which allowed a rapid processing of tissues and became an essential tool in guiding surgeons during surgery (see also Wright, 1985). With these two tools at hand, the study of cells was practically abandoned for nearly a century. Next to autopsy pathology, the mainstay of classification of disease processes during the 18th and 19th centuries, histopathology became the dominant diagnostic mode of human pathology, a position that it holds until today. Histopathology is based on analysis of tissue patterns, which is a much simpler and easier task than the interpretation of smears that often requires tedious synthesis of the evidence dispersed on a slide. Further, histopathology is superior to cytologic samples in determining the relationship of various tissues to each other, for example, in identifying invasion of a cancer into the underlying stroma.
Current Status
The introduction of histopathology on a large scale led to the rapid spread of this knowledge throughout Europe and the Americas. The ever-increasing number of trained people working in leading institutions of medical learning was capable of interpretation of tissue patterns supplementing clinical judgment with a secure microscopic diagnosis. Further, the tissue techniques allowed the preparation of multiple identical samples from the same block of tissue, thus facilitating exchanges between and among pathologists and laying down the foundation of accurate classification of disease processes, staging and grading of cancers and systematic follow-up of patients, with similar disorders, leading to statistical behavioral studies of diseases of a similar type. Such studies became of critical importance in evaluating treatment regimens, initially by surgery or radiotherapy and, even more so, after the introduction of powerful antibiotics and anti-cancer drugs that were active against diseases previously considered hopeless. Nearly all clinical treatment protocols are based on histologic assessment of target lesions. Histologic techniques were also essential in immunopathology that allowed the testing of multiple antibodies on samples of the same tissue. Such studies are difficult to accomplish with smears, which are virtually always unique.
THE RETURN OF CYTOLOGY
Papanicolaou and the Cytology of the Female Genital Tract
The beginnings of the cytology of the female genital tract can be traced to the middle of the 19th century. The microscopic appearance of cells from the vagina was illustrated by several early observers, including Donné and Beale, whose work was discussed above (see Fig. 1-2). In 1847, a Frenchman, F.A. Pouchet, published a book dedicated to the microscopic study of vaginal secretions during the menstrual cycle. In the closing years of the 19th century, sporadic descriptions and illustrations of cancer cells derived from cancer of the uterine cervix were published (see Chap. 11).
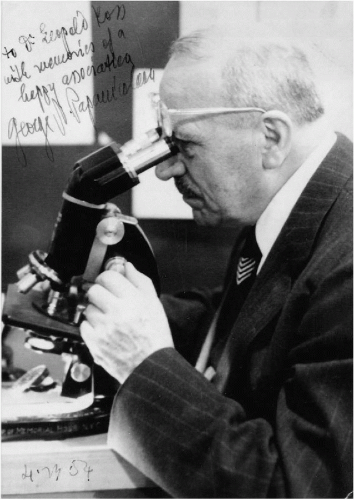
However, there is no doubt whatsoever that the current resurgence of diagnostic cytology is the result of the achievements of Dr. George N. Papanicolaou (1883-1962), an American of Greek descent (Fig. 1-3). Dr. Pap, as he was generally known to his coworkers, friends, and his wife Mary, was an anatomist working at the Cornell University with a primary interest in endocrinology of the reproductive tract. Because of his interest in the menstrual cycle, he developed a small glass pipette that allowed him to obtain cell samples from the vagina of rodents. In smears, he could determine that, during the menstrual cycle, squamous cells derived from the vaginal epithelium of these animals followed a pattern of maturation and atrophy corresponding to maturation of ova. He made major contributions to the understanding of the hormonal mechanisms of ovulation and menstruation and is considered to be one of the pioneering contributors to reproductive endocrinology.
However, his fame is based on an incidental observation of cancer cells in vaginal smears of women whose menstrual cycle he was studying. Papanicolaou had no training in pathology and it is, therefore, not likely that he himself identified the cells as cancerous. It is not known who helped Papanicolaou in the identification of cancer cells. It is probable that it was James Ewing who was at that time Chairman of Pathology at Cornell and who was thoroughly familiar with cancer cells as a consequence of his exposure to aspiration biopsies performed by the surgeon, Hayes Martin, at the Memorial Hospital for Cancer (see below). Papanicolaou’s initial contribution to the subject of “New Cancer Diagnosis,” presented during an obscure meeting on the subject of the Betterment of the Human Race in Battle Creek, MI, in May, 1928, failed to elicit any response. Only in 1939, prodded by Joseph Hinsey, the new Chairman of the Department of Anatomy at Cornell, had Papanicolaou started a systematic cooperation with a gynecologist, Herbert Traut, the Head of Gynecologic Oncology at Cornell, who provided him with vaginal smears on his patients. It soon became apparent that abnormal cells could be found in several of these otherwise asymptomatic patients who were subsequently shown to harbor histologically confirmed carcinomas of the cervix and the endometrium. Papanicolaou and Traut’s article, published in 1941 and a book published in 1943, heralded a new era of application of cytologic techniques to a new target: the discovery of occult cancer of the uterus. Papanicolaou’s name became enshrined in medical history by the term Pap smear, now attached to the cytologic procedure for cervical cancer detection. The stain, also invented by Papanicolaou and bearing his name, was nearly universally adopted in processing cervicovaginal smears.
Papanicolaou’s name was submitted twice to the Nobel Committee in Stockholm as a candidate for the Nobel Award in Medicine. Unfortunately, he was not selected. As a member of the jury told me (LGK) many years later, the negative decision was based on the fact that Papanicolaou had never acknowledged previous contributions of a Romanian pathologist, Aureli Babés (Fig. 1-4), who, working with the gynecologist C. Daniel, reported in January 1927 that cervical smears, obtained by means of a bacteriologic loop, fixed with methanol and stained with Giemsa, were an accurate and reliable method of diagnosing cancer of the uterine cervix. On April 11, 1928, Babés published an extensive, beautifully illustrated article on this subject in the French publication, Presse Médicale, which apparently had remained unknown to Papanicolaou. One of the highlights
of Babés’ article was the observation that a cytologic sample may serve to recognize cancer of the uterine cervix before invasion. Babés’ observations were confirmed only once, by an Italian gynecologist, Odorico Viana in 1928, whereas Papanicolaou’s work stimulated a large number of publications and received wide publicity. Both Babés’ and Viana’s articles were translated into English by Larry Douglass (1967 and 1970).
of Babés’ article was the observation that a cytologic sample may serve to recognize cancer of the uterine cervix before invasion. Babés’ observations were confirmed only once, by an Italian gynecologist, Odorico Viana in 1928, whereas Papanicolaou’s work stimulated a large number of publications and received wide publicity. Both Babés’ and Viana’s articles were translated into English by Larry Douglass (1967 and 1970).
The reason for Papanicolaou’s success and Babés’ failure to attract international attention clearly lies in the differences in geographic location (New York City vs. Bucharest) and in timing. If Papanicolaou’s 1928 article were his only publication on the subject of cytologic diagnosis of cancer, he would have probably remained obscure. He had the great fortune to publish again in the 1940s and his ideas were slowly accepted after the end of World War II, with extensive help from Dr. Charles Cameron, the first Medical and Scientific Director of the American Cancer Society, which popularized the Pap test. A summary of these events was presented at a meeting of the American Cancer Society (Koss, 1993).
The Pap Smear: The Beginning
The value of the vaginal smear as a tool in the recognition of occult cancers of the uterine cervix and the endometrium was rapidly confirmed in a number of articles published in the 1940s (Meigs et al, 1943 and 1945; Ayre, 1944; Jones et al, 1945; Fremont-Smith et al, 1947). It soon became apparent that the vaginal smear was more efficient in the discovery of cervical rather than endometrial cancer and the focus of subsequent investigations shifted to the uterine cervix. In 1948, Lombard et al from Boston introduced the concept of the vaginal smear as a screening test for cancer of the uterine cervix.
Because the vaginal smear was very tedious to screen and evaluate, the proposal by a Canadian gynecologist, J. Ernest Ayre, to supplement or replace it with a cell sample obtained directly from the uterine cervix under visual control was rapidly and widely accepted. In 1947, Ayre ingeniously proposed that a common wooden tongue depressor could be cut with scissors to fit the contour of the cervix, thus adding a very inexpensive tool that significantly improved the yield of cells in the cervical sample. Ayre’s scraper or spatula, now made of plastic, has remained an important instrument in cervical cancer detection.
In 1948, the American Cancer Society organized a national conference in Boston to reach a consensus on screening for cervical cancer. The method was enthusiastically endorsed by the gynecologists but met with skepticism on the part of the participating pathologists. Nonetheless, the first recommendations of the American Cancer Society pertaining to screening for cervical cancer were issued shortly thereafter. In 1950, Nieburgs and Pund published the first results of screening of 10,000 women for occult cancer of the cervix, reporting that unsuspected cancers were detected in a substantial number of screened women. This seminal article, followed by a number of other publications, established the Pap test as a standard health service procedure. Further support for the significance of the test was a series of observations that the smear technique was helpful in discovering precancerous lesions (initially collectively designated as carcinoma in situ), which could be easily treated, thus preventing the development of invasive cancer.
Unfortunately, no double-blind studies of the efficacy of the cervicovaginal smear have ever been conducted, and it became the general assumption that the test had a very high specificity and sensitivity. The legal consequences of this omission became apparent 40 years later.
The Pap Smear From the 1950 to the 1980s
Although the American pathologists, with a few notable exceptions (Reagan, 1951), were reluctant to acknowledge the value of the cervicovaginal smear, toward the end of the 1960s, an ever-increasing number of hospital laboratories were forced to process Pap smears at the request of the gynecologists. In those years, the number of pathologists trained in the interpretation of cytologic material was very small, and it remained so for many years. The responsibility for screening and, usually the interpretation of the smears, was assumed by cytotechnologists who, although few in number, were better trained to perform this function than their medical supervisors. With the support of the National Cancer Institute, several schools for training of cytotechnologists were established in the United States in the 1960s. These trained professionals played a key role in the practice of cytopathology. This time period has also seen the opening of several large commercial laboratories dedicated to the processing of cervicovaginal smears. New books, journals, and postgraduate courses offered by a number of professional organizations gave the pathologists an opportunity to improve their skills in this difficult field of diagnosis.
Several very successful programs of cervix cancer detection were established in the United States and Canada, and it became quite apparent that the mortality from cancer of the uterine cervix could be lowered in the screened populations. As a consequence, by the end of the 1980s, a 70% reduction in the mortality from this disease was recorded in several geographic areas where mass screening was introduced. However, in none of the populations screened was cancer of the cervix completely irradicated.
The Pap Smear From the 1980s to Today
In the 1970s and early 1980s, several articles commenting on the failure of the cervicovaginal smear in preventing the developments of invasive cancer of the uterine cervix appeared in the American literature and in Sweden (Rylander, 1976; Fetherstone, 1983; Koss, 1989; summary in Koss and Gompel, 1999). The reports did not fully analyze the reasons for failure and were generally ignored. In 1987, however, an article in the Wall Street Journal by an investigative journalist, Walt Bogdanich, on failure of laboratories to identify cancer of the cervix in young women, some who were mothers of small children, elicited a great deal of attention. It prompted the Congress of the United States in 1988 to promulgate a law, known as the Amendment to the Clinical
Laboratory Improvement Act (CLIA 88), governing the practice of gynecologic cytology in the United States. The implications of the law in reference to practice of cytopathology are discussed elsewhere in this book (see Chap. 44). Suffice it to say, cytopathology, particularly in reference to cervicovaginal smears, has become the object of intense scrutiny and legal proceedings against pathologists and laboratories for alleged failure to interpret the smears correctly, casting a deep shadow on this otherwise very successful laboratory test.
Laboratory Improvement Act (CLIA 88), governing the practice of gynecologic cytology in the United States. The implications of the law in reference to practice of cytopathology are discussed elsewhere in this book (see Chap. 44). Suffice it to say, cytopathology, particularly in reference to cervicovaginal smears, has become the object of intense scrutiny and legal proceedings against pathologists and laboratories for alleged failure to interpret the smears correctly, casting a deep shadow on this otherwise very successful laboratory test.
As a consequence of these events, several manufacturers have proposed changes in collection and processing of the cervicovaginal smears. The collection methods of cervical material in liquid media, followed by automated processing with resulting “monolayer” preparations, have been approved by the Food and Drug Administration (USA). Other manufacturers introduced apparatuses for automated screening of conventional smears. New sampling instruments were also developed and widely marketed, notably endocervical brushes. All these initiatives were designed to reduce the risk of errors in the screening and interpretation of cervicovaginal smears. These issues are discussed in Chapters 8, 11, 12, and 44.
DEVELOPMENTS IN NONGYNECOLOGIC CYTOLOGY
Historical Overview
At the time of early developments in general cytology in the 19th century, summarized above, numerous articles were published describing the application of cytologic techniques to various secreta and fluids, such as sputum, urine, effusions, and even vomit for diagnostic purposes. These contributions have been described in detail in Grunze and Spriggs’ book. The recognition of lung cancer cells in sputum by Beale in 1858 was mentioned above.
As lung cancer became a serious public health dilemma in the 1930s and 1940s, in Great Britain, Dudgeon and Wrigley developed, in 1935, a method of “wet” processing of smears of fresh sputum for the diagnosis of lung cancer. The method was used by Wandall in Denmark in 1944 on a large numbers of patients, with excellent diagnostic results. Woolner and McDonald (1949) at the Mayo Clinic and Herbut and Clerf (1946) in Philadelphia also studied the applications of cytology to lung cancer diagnosis. In the late 1940s and early 1950s, Papanicolaou, with several co-workers, published a number of articles on the application of cytologic techniques to the diagnosis of cancer of various organs, illustrated in his Atlas. In the United Kingdom, urine cytology was applied by Crabbe (1952) to screening of industrial workers for cancer of the bladder and gastric lavage techniques by Schade (1956) to screening for occult gastric cancer, a method extensively used in Japan for population screening. Esophageal balloon technique was applied on a large scale in China for detecting precursor lesions of esophageal carcinoma. Screening for oral cancer has been shown to be successful in discovering occult carcinomas in situ. Thus, conventional cytologic techniques, when judiciously applied, supplement surgical pathology in many situations when a tissue biopsy is either not contemplated, indicated, or not feasible. It needs to be stressed that cytopathology has made major contributions to the recognition of early stages of human cancer in many organs and, thus, contributed in a remarkable way to a better understanding of events in human carcinogenesis and to preventive health care. These, and many other applications of cytologic techniques to the diagnosis of early and advanced cancer and of infectious disorders of various organs, are discussed in this text.
THE ASPIRATION BIOPSY (FNA)
The Beginning
Ever since syringes or equivalent instruments were introduced into the medical armamentarium, probably in the 15th century of our era, they were used to aspirate collections of fluids. With the introduction of achromatic microscopes and their industrial production in the 1830s, the instrument became accessible to many observers who used it to examine the aspirated material. It has been mentioned above that a French physician, Kün, and a German-Swiss pathologist, Lebert, described, in 1847 and 1851, the use of a cannula to secure cell samples from palpable tumors and used the microscope to identify cancer. Sporadic use of aspirated samples has been described in the literature of the second half of the 19th century and in the first years of the 20th century. An important contribution was published in 1905 by two British military surgeons, Greig and Gray, working in Uganda who aspirated the swollen lymph nodes, by means of a needle and a syringe, of patients with sleeping sickness to identify the mobile trypanosoma (see Webb, 2001 for an excellent recent account of early investigators).
In the 20th century, to my knowledge, the first aspiration biopsy diagnosis of a solid tumor of the skin (apparently a lymphoma) was published by Hirschfeld (1912), who was the first person to use a small-caliber needle. He subsequently extended his experience to other tumors, but was prevented by World War I from publishing his results until 1919. Several other early observers reported on the aspiration of lymph nodes and other accessible sites (Webb, 2001).
The most notable development in diagnostic aspiration biopsy was a paradoxical event. James Ewing, the Director of the Memorial Hospital for Cancer in New York City and also a Professor of Pathology at Cornell University Medical School, was a dominant figure in American oncologic pathology between 1910 and 1940. Although Ewing has made great contributions to the classification and identification of human cancer, he was adamantly opposed to tissue biopsies because they allegedly contributed to the spread of cancer (Koss and Lieberman, 1997). Because of the ban on tissue biopsies, a young surgeon and radiotherapist at the Memorial Hospital, Hayes Martin, who refused to treat patients
without a preoperative diagnosis, began to aspirate palpable tumors of various organs by means of a large-caliber needle and a Record syringe. The material was prepared in the form of air-dried smears, stained with hematoxylin and eosin by Ewing’s technician, Edward Ellis. Tissue fragments (named clots) were embedded in paraffin and processed as cell blocks. Palpable lesions of lymph nodes, breast, and thyroid were the initial targets of aspiration. The material was interpreted by Ewing’s associate and subsequent successor (and my Chief-LGK), Dr. Fred W. Stewart. In response to a specific query, the reasons for this development were explained many years later in a letter dated June 30, 1980, written by Dr. Fred W. Stewart to this writer.
without a preoperative diagnosis, began to aspirate palpable tumors of various organs by means of a large-caliber needle and a Record syringe. The material was prepared in the form of air-dried smears, stained with hematoxylin and eosin by Ewing’s technician, Edward Ellis. Tissue fragments (named clots) were embedded in paraffin and processed as cell blocks. Palpable lesions of lymph nodes, breast, and thyroid were the initial targets of aspiration. The material was interpreted by Ewing’s associate and subsequent successor (and my Chief-LGK), Dr. Fred W. Stewart. In response to a specific query, the reasons for this development were explained many years later in a letter dated June 30, 1980, written by Dr. Fred W. Stewart to this writer.
Martin and Ewing were at sword’s point on the need for biopsy proof prior to aggressive surgery or radiation (in neck nodes since Hayes Martin dealt exclusively in head and neck stuff) and the needle was a sort of compromise. Ewing thought biopsy hazardous—a method of disease spread. The material was seen mostly by me (FWS). Ewing, at the time, was quite inactive. Eddie Ellis merely fixed and stained the slides. He probably looked at them—he was used to looking at stuff with Ewing and really knew more about diagnoses than a lot of pathologists of the period. The needle really spread from neck nodes to the various other regions, especially to the breast, of course.
The method proved to be very successful and accurate with very few errors or clinical complications. Martin and Ellis published their initial results in 1930 and 1934. In 1933, Dr. Fred W. Stewart published a classic article, “The Diagnosis of Tumors by Aspiration,” in which he discussed, at length, the pros and cons of this method of diagnosis, its achievements, and pitfalls, based on experience with several hundred samples. As Stewart himself stated in a letter (to LGK), he was “damned by many for having advocated this insecure and potentially harmful method of diagnosis, without a shred of proof.” For a detailed description of these events, see Koss and Lieberman (1997)




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree