Patient Story
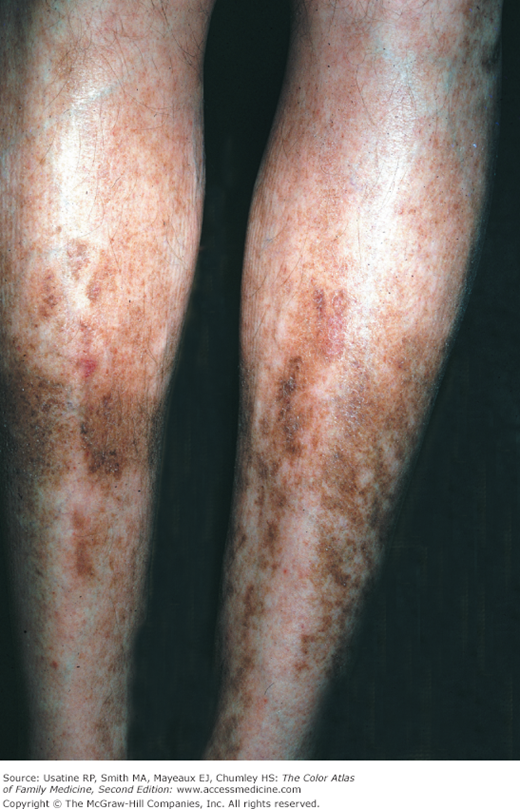
A 60-year-old woman with diabetes mellitus (DM) for the past 10 years began to notice reddish-colored lesions on both anterior shins that turned brown over the past year (Figure 221-1). She reported no pain with the hyperpigmented areas but does have foot pain secondary to neuropathy. The patient is diagnosed with diabetic dermopathy, and she begins working with her physician on achieving better control of her diabetes.
Figure 221-1
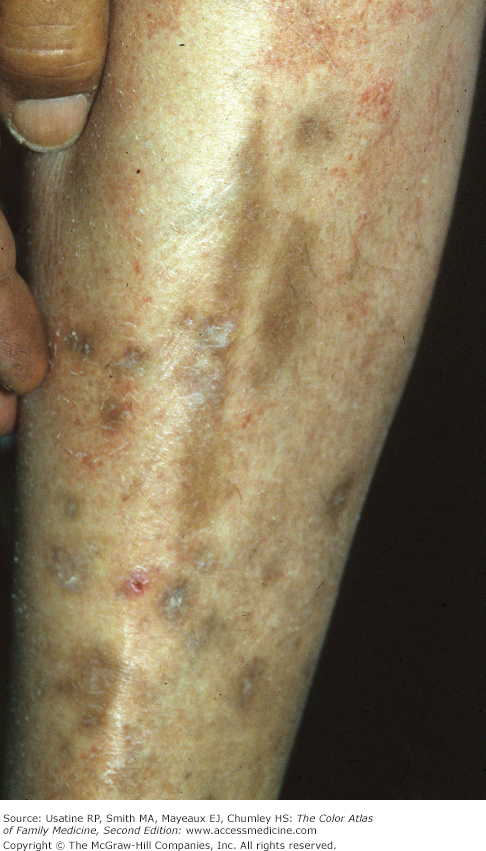
Lesions of diabetic dermopathy (also called pigmented pretibial papules) on both lower extremities of a 60-year-old woman with diabetes. The skin appears atrophic and the lesions are flat and hyperpigmented. (Courtesy of the University of Texas Health Sciences Center, Division of Dermatology.)
Introduction
Epidemiology
- Diabetic dermopathy is found in 12.5% to 40% of patients and most often in the elderly. It is less common in women.1
- In a case series of 100 consecutive inpatients or outpatients in India with DM and skin lesions, diabetic dermopathy was found in 36%.2 The incidence was much lower in a second case series of 500 patients attending a diabetes clinic in India, with only 0.2% diagnosed with diabetic dermopathy; the authors concluded that because the majority of patients were well controlled (fasting blood sugar <130 mg/mL in 60%), cutaneous signs of chronic hyperglycemia were decreased.3
- Sometimes seen in persons without DM, especially patients with circulatory compromise.
Etiology and Pathophysiology
- Diabetic dermopathy may be related to mechanical or thermal trauma, especially in patients with neuropathy.
- Lesions have been classified as vascular because histology sections demonstrate red blood cell extravasation and capillary basement membrane thickening. In one study, patients with type 1 DM and diabetic dermopathy had marked reduction in skin blood flow at normal-appearing skin areas on the pretibial surface of the legs compared with type 1 control and nondiabetic control patients.4
- There is an association between diabetic dermopathy and the presence of retinopathy, nephropathy, and neuropathy.5,6 In a Turkish study, women with diabetic dermopathy appeared to have a more severe sensorial neuropathy (e.g., loss of deep tendon reflexes, superficial sensory loss, and the loss of vibration sense) than did patients without these skin lesions; a high prevalence of carpel tunnel syndrome (63.8%) was also found in these patients.7
Diagnosis
The diagnosis is usually clinical. Lesions often begin as pink patches (0.5 to 1 cm), which become hyperpigmented with surface atrophy and fine scale (Figures 221-1, 221-2, 221-3, and 221-4).