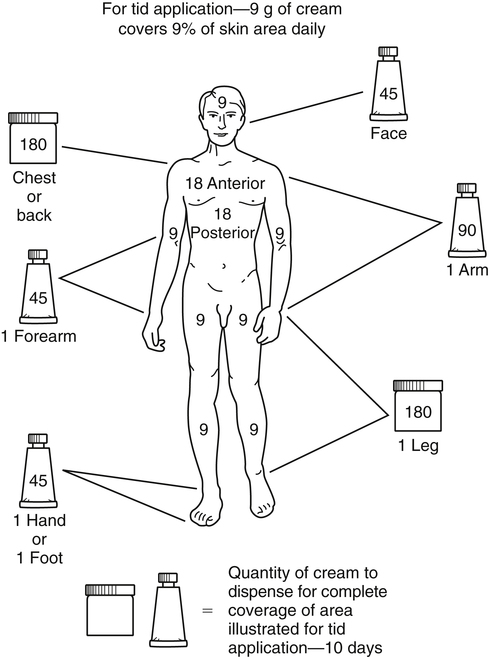
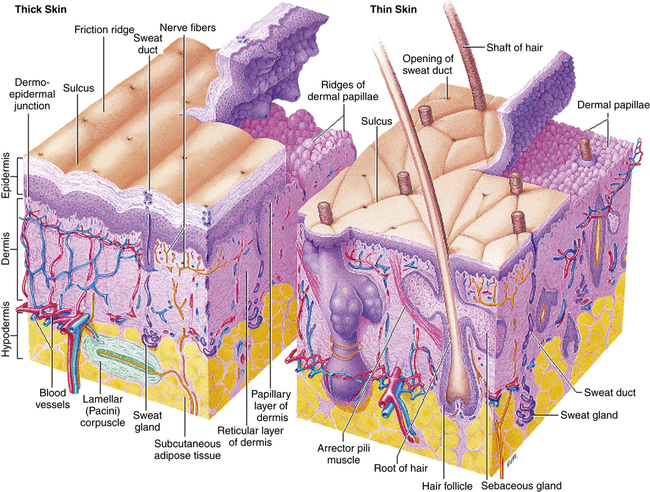
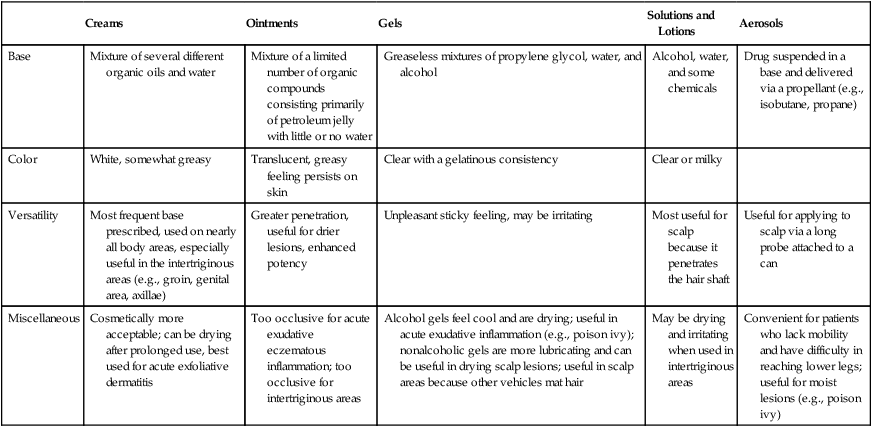
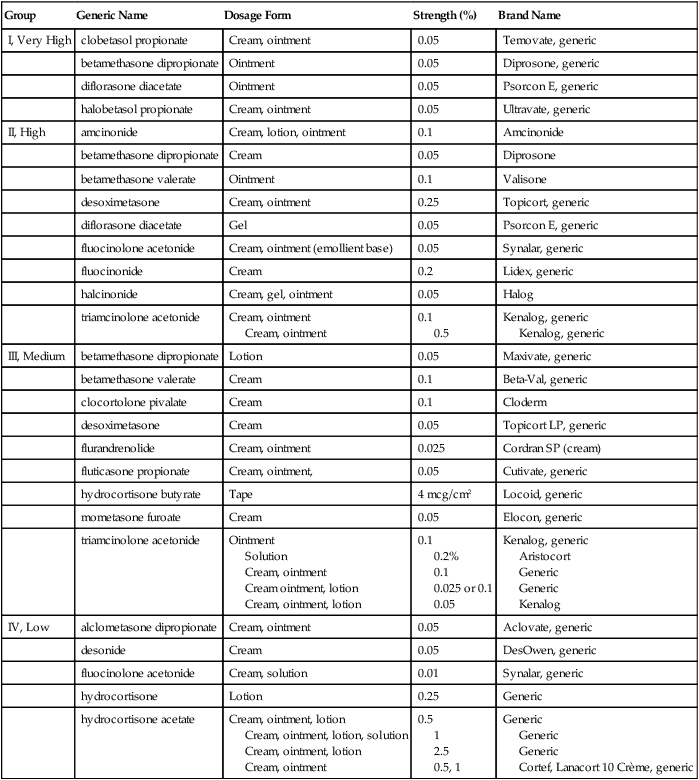
Chapter 13 The skin, the largest organ of the body, consists of three distinct layers: epidermis, dermis, and subcutaneous tissue (Figure 13-1). The epidermis is the outer layer of the skin. The thickness of the epidermis ranges from 0.05 mm on the eyelids to 1.5 mm on the palms and soles. Five layers make up the epidermis. Basal cells form a single layer of cells that make up the innermost layer of the epidermis. These basal cells divide to form keratinocytes. The other layers are formed as keratinocytes change until they migrate to the outer layer to become the major component of the stratum corneum. The stratum corneum provides protection to the skin by acting as a barrier. The thicker the epidermis, the greater the barrier protection. Factors that affect the extent of drug absorption into the skin include the status of the skin, the characteristics of the drug, and the characteristics of the administration vehicle. Absorption is increased when the skin is broken or inflamed. In addition, absorption increases in cases in which skin integrity is compromised or the skin is thinner. Because of the vascular composition of the skin, mucous membranes absorb medication in high concentrations. The vehicle or base affects percutaneous absorption (Table 13-1). The vehicle may hydrate the outer layer of skin by preventing water loss. With improved hydration, the absorption of medication and the depth of penetration are enhanced. TABLE 13-1 Characteristics of Vehicle of Selected Topical Products Prescribing the appropriate amount of topical medication is important. Too large a tube may be very costly to the patient, yet a small tube may not include enough medication to cover the entire area. To estimate the amount that should be prescribed, the rule of nines can be used (Figure 13-2). 1. Take a small amount of cream or ointment into the palm of the hand, and rub the hands together until the medication has a thin sheen. 2. Apply a small amount of ointment or cream as a thin layer to the skin. Excess medication is lost when it rubs off onto the clothing. 3. Apply topical medications with long, downward strokes to the affected areas. Avoid back-and-forth strokes because they may cause irritation of the hair follicles. 4. A tongue blade may be used for the application of topicals in a paste form. 1. Instruct the patient to shake the container to mix the suspension well. 2. Carefully pour a small quantity of lotion into the palm of the hand. 3. Apply a thin layer to the skin using firm, downward strokes. Avoid using gauze unless the liquid is very thin. Cotton balls should be avoided when medication is applied because they retain the suspended particles of medication. • Specifics are discussed under each class of drug. • Geriatric skin is thinner and is more absorbent than the skin of younger adults. • Children absorb about three times as much as adults do. • Children younger than 12 years of age generally should not be treated with group I or II topical corticosteroids. • Pregnant and lactating women need to be especially careful about topical agents that are absorbed systemically. Agents known to be harmful to the fetus include tretinoin, lindane, and podophyllum. • Apply a small amount to the affected area two to four times a day. • These products are for external use only. Do not use in the eyes. • If the condition does not improve in 3 to 5 days, call the health care provider. • If the condition worsens, or if a skin reaction develops, discontinue the agent. Wash the affected area and call the health care provider. For a listing, see Table 13-2. TABLE 13-2 Topical Corticosteroids Ranked by Potency∗ ∗Range: Group I (very potent) to Group IV (least potent). Note: Some of the drugs appear in more than one category. Topical corticosteroids diffuse across cell membranes and induce cutaneous vasoconstriction commensurate with their potency. This results in a local antiinflammatory effect. The topical route is elected when a local effect is preferred to the systemic effect produced by the same product given orally. Topical corticosteroids inhibit the migration of macrophages and leukocytes into the area by reversing vascular dilation and permeability of small vessels in the upper dermis. See Chapter 51 for further information. No general standardized guidelines are found. There are some guidelines for treatment of specific diseases or skin conditions. See www.guidelines.gov for specific conditions. (See Table 13-4.) • Initiate therapy with an agent of the lowest potency needed, and use for as short a time as possible. • Group I corticosteroids are used for severe dermatoses over nonfacial/nonintertriginous areas such as psoriasis, severe atopic dermatitis, or severe contact dermatitis. They are especially useful over the palms and soles, which tend to resist topical corticosteroid penetration because of skin thickness. • Preparations of intermediate to potent strength are appropriate for mild to moderate nonfacial/nonintertriginous dermatoses. • Eyelid and genital dermatoses should be treated with topical corticosteroids of mild strength. • Preparations of mild to intermediate strength should be considered when large areas are treated because of the likelihood of systemic absorption. • Treatment should be discontinued when the skin condition has resolved. Tapering the corticosteroid will prevent recurrence of the skin condition. Tapering is best performed by gradually reducing the potency and dosing frequency at 2-week intervals. • Therapy may be continued for chronic diseases that are responsive to treatment; patients should be monitored for the development of adverse effects and/or tachyphylaxis (rapid development of a decreased response). • Generic topical corticosteroids are effective for treatment of most skin disorders in the primary care setting. Generic medications often have slightly less potency or vehicles that are less cosmetically appealing, but the substantial cost savings may offset any differences in efficacy or feel. • Reevaluate after about 10 days to determine whether the condition is responding to treatment. • High-potency topical corticosteroids may require periodic evaluation of HPA axis suppression with the use of morning plasma cortisol, urinary free cortisol, and adrenocorticotropic hormone (ACTH) stimulation tests. If evidence of HPA axis suppression is noted, the health care provider should attempt to withdraw the topical corticosteroid very gradually. Decrease the number of applications or change to the use of a less-potent corticosteroid to begin withdrawing the corticosteroid from the patient. • Geriatric patients are more susceptible to secondary infection when corticosteroids are used. • They also are more susceptible to the systemic effects of topically applied medications because their skin tends to be thin. • Children, in comparison with adults, have a larger skin surface area–to–body weight ratio. They may be more susceptible to topical corticosteroid–induced HPA axis suppression and Cushing’s syndrome. In children, symptoms of HPA may include linear growth retardation, delayed weight gain, and low cortisol levels. • The least-potent corticosteroid that is compatible with effective treatment should be used. • Potent corticosteroids should not be used to treat diaper dermatoses. • Children younger than 12 years of age generally should not be treated with group I or II topical corticosteroids. • Category C: No reports have described congenital anomalies or adverse effects associated with the use of corticosteroids during pregnancy. The use of group I through III corticosteroids in large amounts and with occlusive dressings for long periods of time has been shown to cause fetal abnormalities in animals, although none have been documented in humans. • There is a significant association of fetal growth restriction with maternal exposure to potent/very potent topical corticosteroids, but not with mild/moderate topical corticosteroids. • Effects on lactation are not known. • Corticosteroids absorbed systemically can be detected in breast milk in quantities that are not likely to affect the infant. • These drugs should not be applied to the nipples prior to nursing. Mupirocin is the only drug in this class that is used exclusively for topical infection, and it is the only one discussed here in detail. Mupirocin represents a major advance because it allows topical treatment of impetigo. Bacitracin is very effective for most topical infections. Triple antibiotic ointments vary in their composition; usually, they contain neomycin, which causes a greater number of allergic reactions than are produced by other topical agents. See Chapter 58 for information on other drugs in this class. • Appropriate drug selection depends on diagnosis and culture whenever possible. • Prolonged use of any of these topical agents may result in overgrowth of nonsusceptible organisms. • Systemic antibiotics are needed for diffuse impetigo, cellulitis, and other more-than-superficial infections. Apply gauze dressing if indicated. • Treatment should be reevaluated if no improvement is seen in 3 to 5 days (Table 13-3). TABLE 13-3 Important Characteristics of Topical Antibiotics
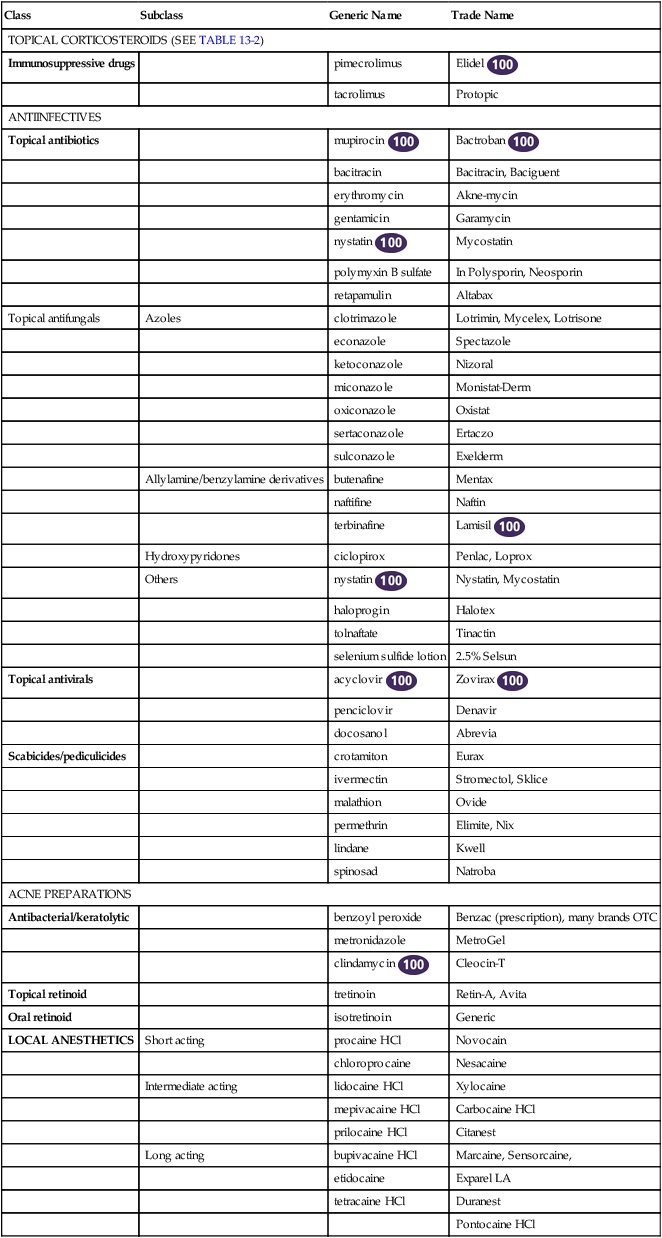
Dermatologic Agents
Class
Subclass
Generic Name
Trade Name
TOPICAL CORTICOSTEROIDS (SEE TABLE 13-2)
Immunosuppressive drugs
pimecrolimus
Elidel ![]()
tacrolimus
Protopic
ANTIINFECTIVES
Topical antibiotics
mupirocin ![]()
Bactroban ![]()
bacitracin
Bacitracin, Baciguent
erythromycin
Akne-mycin
gentamicin
Garamycin
nystatin ![]()
Mycostatin
polymyxin B sulfate
In Polysporin, Neosporin
retapamulin
Altabax
Topical antifungals
Azoles
clotrimazole
Lotrimin, Mycelex, Lotrisone
econazole
Spectazole
ketoconazole
Nizoral
miconazole
Monistat-Derm
oxiconazole
Oxistat
sertaconazole
Ertaczo
sulconazole
Exelderm
Allylamine/benzylamine derivatives
butenafine
Mentax
naftifine
Naftin
terbinafine
Lamisil ![]()
Hydroxypyridones
ciclopirox
Penlac, Loprox
Others
nystatin ![]()
Nystatin, Mycostatin
haloprogin
Halotex
tolnaftate
Tinactin
selenium sulfide lotion
2.5% Selsun
Topical antivirals
acyclovir ![]()
Zovirax ![]()
penciclovir
Denavir
docosanol
Abrevia
Scabicides/pediculicides
crotamiton
Eurax
ivermectin
Stromectol, Sklice
malathion
Ovide
permethrin
Elimite, Nix
lindane
Kwell
spinosad
Natroba
ACNE PREPARATIONS
Antibacterial/keratolytic
benzoyl peroxide
Benzac (prescription), many brands OTC
metronidazole
MetroGel
clindamycin ![]()
Cleocin-T
Topical retinoid
tretinoin
Retin-A, Avita
Oral retinoid
isotretinoin
Generic
LOCAL ANESTHETICS
Short acting
procaine HCl
Novocain
chloroprocaine
Nesacaine
Intermediate acting
lidocaine HCl
Xylocaine
mepivacaine HCl
Carbocaine HCl
prilocaine HCl
Citanest
Long acting
bupivacaine HCl
Marcaine, Sensorcaine,
etidocaine
Exparel LA
tetracaine HCl
Duranest
Pontocaine HCl
Therapeutic Overview of Dermatologic Agents
Anatomy and Physiology
Mechanism of Action
Creams
Ointments
Gels
Solutions and Lotions
Aerosols
Base
Mixture of several different organic oils and water
Mixture of a limited number of organic compounds consisting primarily of petroleum jelly with little or no water
Greaseless mixtures of propylene glycol, water, and alcohol
Alcohol, water, and some chemicals
Drug suspended in a base and delivered via a propellant (e.g., isobutane, propane)
Color
White, somewhat greasy
Translucent, greasy feeling persists on skin
Clear with a gelatinous consistency
Clear or milky
Versatility
Most frequent base prescribed, used on nearly all body areas, especially useful in the intertriginous areas (e.g., groin, genital area, axillae)
Greater penetration, useful for drier lesions, enhanced potency
Unpleasant sticky feeling, may be irritating
Most useful for scalp because it penetrates the hair shaft
Useful for applying to scalp via a long probe attached to a can
Miscellaneous
Cosmetically more acceptable; can be drying after prolonged use, best used for acute exfoliative dermatitis
Too occlusive for acute exudative eczematous inflammation; too occlusive for intertriginous areas
Alcohol gels feel cool and are drying; useful in acute exudative inflammation (e.g., poison ivy); nonalcoholic gels are more lubricating and can be useful in drying scalp lesions; useful in scalp areas because other vehicles mat hair
May be drying and irritating when used in intertriginous areas
Convenient for patients who lack mobility and have difficulty in reaching lower legs; useful for moist lesions (e.g., poison ivy)
Treatment Principles
How Topical Agents Are Used
Creams, Ointments, and Pastes
Lotions
Patient Variables
Patient Education
Topical Corticosteroids
Group
Generic Name
Dosage Form
Strength (%)
Brand Name
I, Very High
clobetasol propionate
Cream, ointment
0.05
Temovate, generic
betamethasone dipropionate
Ointment
0.05
Diprosone, generic
diflorasone diacetate
Ointment
0.05
Psorcon E, generic
halobetasol propionate
Cream, ointment
0.05
Ultravate, generic
II, High
amcinonide
Cream, lotion, ointment
0.1
Amcinonide
betamethasone dipropionate
Cream
0.05
Diprosone
betamethasone valerate
Ointment
0.1
Valisone
desoximetasone
Cream, ointment
0.25
Topicort, generic
diflorasone diacetate
Gel
0.05
Psorcon E, generic
fluocinolone acetonide
Cream, ointment (emollient base)
0.05
Synalar, generic
fluocinonide
Cream
0.2
Lidex, generic
halcinonide
Cream, gel, ointment
0.05
Halog
triamcinolone acetonide
Cream, ointment
Cream, ointment
0.1
0.5
Kenalog, generic
Kenalog, generic
III, Medium
betamethasone dipropionate
Lotion
0.05
Maxivate, generic
betamethasone valerate
Cream
0.1
Beta-Val, generic
clocortolone pivalate
Cream
0.1
Cloderm
desoximetasone
Cream
0.05
Topicort LP, generic
flurandrenolide
Cream, ointment
0.025
Cordran SP (cream)
fluticasone propionate
Cream, ointment,
0.05
Cutivate, generic
hydrocortisone butyrate
Tape
4 mcg/cm2
Locoid, generic
mometasone furoate
Cream
0.05
Elocon, generic
triamcinolone acetonide
Ointment
Solution
Cream, ointment
Cream ointment, lotion
Cream, ointment, lotion
0.1
0.2%
0.1
0.025 or 0.1
0.05
Kenalog, generic
Aristocort
Generic
Generic
Kenalog
IV, Low
alclometasone dipropionate
Cream, ointment
0.05
Aclovate, generic
desonide
Cream
0.05
DesOwen, generic
fluocinolone acetonide
Cream, solution
0.01
Synalar, generic
hydrocortisone
Lotion
0.25
Generic
hydrocortisone acetate
Cream, ointment, lotion
Cream, ointment, lotion, solution
Cream, ointment, lotion
Cream, ointment
0.5
1
2.5
0.5, 1
Generic
Generic
Generic
Cortef, Lanacort 10 Crème, generic
Mechanism of Action
Treatment Principles
Standardized Guidelines
Cardinal Points of Treatment
How to Monitor
Patient Variables
Geriatrics
Pediatrics
Pregnancy and Lactation
Antiinfectives
Topical Antibiotics
Treatment Principles
Antibiotic
Effective Against
Formulation
Administration
mupirocin
Gram positive
2% cream, ointment
tid
bacitracin
Gram positive
500 units/g ointment
daily to qid
erythromycin
Gram positive
0.5% (ophthalmic), 2% ointment; 2% gel
bid/tid
gentamicin
Gram negative
0.3% ointment (ophthalmic); 0.1% ointment, cream
tid or qid
neomycin
Gram negative
3.5, 5 mg/g ointment; 3.5 mg/g cream
tid
polysporin with neomycin and bacitracin
Gram negative
5000 or 10,000 units/g cream, ointment
tid
retapamulin
Gram positive, anaerobes
1% ointment
bid ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Dermatologic Agents
Only gold members can continue reading. Log In or Register to continue