Dermatofibrosarcoma Protuberans
Thomas Mentzel, MD
Cyril Fisher, MD, DSc, FRCPath
Key Facts
Terminology
Dermatofibrosarcoma represents superficially located low-grade fibroblastic sarcoma that may show progression to fibrosarcomatous dermatofibrosarcoma protuberans
Clinical Issues
Young adults
Rare in childhood
Trunk (chest, back, shoulder, abdominal wall)
Proximal > distal extremities > head/neck region
Slowly growing nodular dermal neoplasm
Wide excision is necessary
Imatinib treatment in advanced and metastatic cases
Increased number of often repeated local recurrences
Metastases are extremely rare (< 0.5%)
May show progression to fibrosarcomatous DFSP
Microscopic Pathology
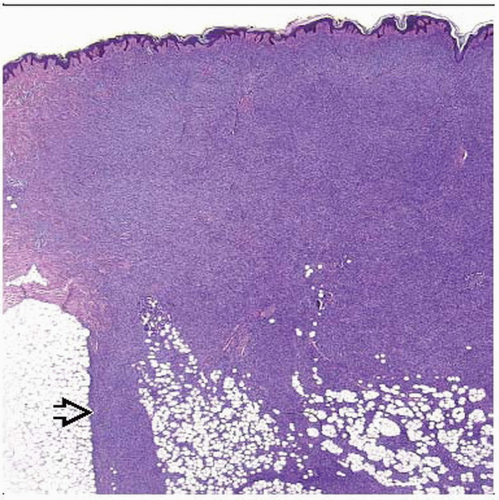
Diffuse infiltration of dermis and subcutis
Infiltration along fibrous septa of subcutaneous fat
Characteristic honeycomb infiltration of subcutaneous fat
Storiform growth
Uniform spindled tumor cells
Homogeneous expression of CD34
Giant cell fibroblastoma
Hypocellular neoplasms with angiectoid spaces and multinucleated giant cells
Fibrosarcomatous DFSP
Abrupt or gradual transition
Cellular spindle cell fascicles with increased atypia and proliferative activity
 Dermatofibrosarcoma protuberans is characterized clinically by an exophytic, multinodular growth in most cases. |
TERMINOLOGY
Abbreviations
Dermatofibrosarcoma protuberans (DFSP)
Definitions
Superficially located low-grade fibroblastic sarcoma
Can progress to fibrosarcomatous dermatofibrosarcoma protuberans
CLINICAL ISSUES
Epidemiology
Incidence
Rare neoplasm
One of most frequent superficially located sarcomas
Age
Young adults
Rare in childhood or older age
Gender
Slight male predominance
Site
Trunk (chest, back, shoulder, abdominal wall)
Proximal extremities > distal extremities
Head and neck region
Rare in genital areas
Presentation
Slowly growing nodular dermal neoplasm
Often history of slow but persistent growth
Can show rapid enlargement due to tumor progression
Can show rapid enlargement in pregnancy
Rarely plaque-like growth
Treatment
Surgical approaches
Wide excision (2-3 cm)
Adjuvant therapy
Imatinib treatment in advanced and metastatic cases
Prognosis
Locally aggressive growth
Increased number of often repeated local recurrences
Metastases extremely rare (< 0.5%)
May progress to fibrosarcomatous DFSP
MACROSCOPIC FEATURES
General Features
Indurated dermal plaques
1 or more tumor nodules
Multiple protuberant tumors are often seen in recurrent cases
Firm gray-white cut surface
Usually no tumor necrosis
Rarely subcutaneous
Sections to Be Submitted
Numerous sections have to be submitted
Resection margins have to be carefully assessed
Size
May reach considerable size
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse infiltration of dermis and subcutis
Infiltration along fibrous septa of subcutaneous fat
Characteristic honeycomb pattern
Tumor cells encase skin appendages
Storiform growth pattern
Uniform spindled tumor cells
Plump spindled or elongated wavy nuclei
Only mild cytologic atypia, < 5 mitoses per 10 high-power fields
Collagenous stroma with small vessels
May contain pigmented melanocytic cells (pigmented DFSP, so-called Bednar tumor)
May show prominent myxoid changes (myxoid DFSP)
May contain bundles and nests of myofibroblastic cells (DFSP with myoid differentiation)
May rarely show flat, plaque-like growth (plaque-like DFSP, atrophic DFSP)
May rarely show granular cell changes (granular DFSP)
Margins
Ill defined, infiltrative
Predominant Pattern/Injury Type
Diffuse
Predominant Cell/Compartment Type
Spindle
Fibroblast
Giant Cell Fibroblastoma
Primarily affects children in 1st decade of life, rarely adults
Strong male predilection
Locally aggressive neoplasm, frequent local recurrence
Metastases have not been reported yet
Hypocellular, with myxoid to collagenous stroma
Spindled tumor cells and scattered mono- &/or multinucleated giant cells
Irregular branching angiectoid spaces
Fibrosarcomatous DFSP
Represents morphologic form of progression (grade 2 malignancy)
10-15% metastasize, and sometimes cause death
Occurs de novo or more rarely in local recurrence
Abrupt or gradual fibrosarcomatous transformation
Often nodular, rather well-circumscribed growth
Cells arranged in cellular “herringbone” fascicles
Increased atypia and mitotic index
Increased p53 expression
ANCILLARY TESTS
Immunohistochemistry
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree