Dermatofibroma (Benign Fibrous Histiocytoma)
David S. Cassarino, MD, PhD
Key Facts
Terminology
Benign limited proliferation of histiocytic and fibroblastic cells in dermis
Etiology/Pathogenesis
Evidence supports both neoplastic and reactive pathogenesis
Clinical Issues
Affects all ages and both sexes but most common in young adults
Excellent prognosis in vast majority of cases
Metastasis and death in rare cases of cellular and atypical tumors
Microscopic Pathology
Dermal-based proliferation of typically bland spindled to histiocytic-appearing cells
Collagen trapping at periphery
Overlying epithelial basilar induction with hyperpigmentation
Adjacent adnexal hyperplasia
Ancillary Tests
FXIIIA(+), CD163(+), CD68(+), CD34(-)
Top Differential Diagnoses
Basal cell carcinoma
CD20(+) Merkel cells overlying DF
Angiosarcoma and Kaposi sarcoma
CD31 and HHV8 are negative in aneurysmal DF
Dermatofibrosarcoma protuberans
Deep subcutaneous extension and fat entrapment
CD34, CD163, and FXIIIA usually allow for distinction
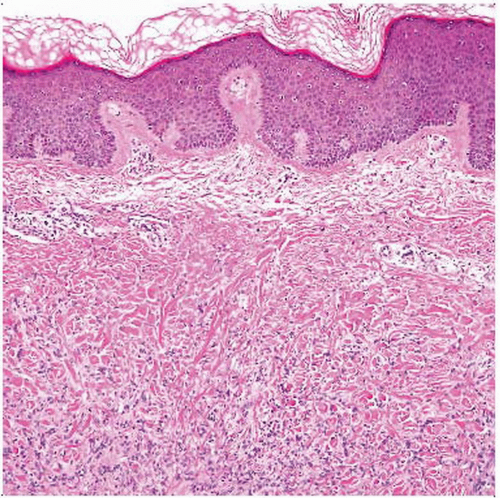 Classic dermatofibroma shows a dermal-based proliferation of bland spindled to histiocytic-appearing cells, associated with a Grenz zone and overlying epidermal hyperplasia and basilar pigmentation. |
TERMINOLOGY
Abbreviations
Dermatofibroma (DF)
Fibrous histiocytoma (FH)
Synonyms
Cutaneous fibrous histiocytoma
Sclerosing hemangioma
Histiocytoma
Epithelioid cell histiocytoma
Definitions
Common, benign, limited proliferation of mesenchymal cells in dermis
Lineage not well defined, although commonly referred to as “fibrohistiocytic”
ETIOLOGY/PATHOGENESIS
Unknown
Evidence supports both reactive and neoplastic pathogenesis
Histiocytic population may be clonal; fibroblast/myofibroblastic population may be polyclonal (reactive)
Tumor may be preceded by local trauma, including insect bite in some cases
However, often no inciting event identified
CLINICAL ISSUES
Epidemiology
Incidence
Common tumors in most populations
Age
All ages, but most common in 4th and 5th decades
Gender
Affects males and females equally
Site
Typically occur on distal extremities but may present at any cutaneous site
Presentation
Firm, isolated, flesh-colored subcutaneous papule or nodule
New DFs are typically pink (vascular); older DFs are brown (overlying melanocyte hyperplasia)
Multiple DFs occur in immunosuppressed populations
“Dimpling” sign when in vivo DF is pinched by fingers
Treatment
Excision usually curative
Prognosis
Excellent in vast majority of cases
Local recurrence potential significant (up to 30%) with cellular variant
Metastasis and death from some cellular and atypical tumors reported
Usually large and deep lesions
MACROSCOPIC FEATURES
General Features
Firm, circumscribed but nonencapsulated, dermalbased tumor
White to yellow cut surface
Can have cystic changes and hemorrhage
MICROSCOPIC PATHOLOGY
Histologic Features
Dermal-based proliferation of typically bland spindled to histiocytic-appearing cells
Either spindled (fibroblastic) or histiocytoid cells may predominate
Early lesions typically show more histiocytes and lymphocytes
Established lesions show greater cellularity and spindled cells
Older lesions show more fibrosis
Spindled cells show elongated eosinophilic cytoplasmic processes
“Histiocytic” type cells are larger, epithelioid-shaped, and have abundant pale vacuolated cytoplasm
Cytologic atypia and pleomorphism are usually minimal
Tumors are grossly circumscribed but microscopically have irregular, often jagged borders
Collagen trapping at periphery
Spheres of intensely eosinophilic collagen (socalled “collagen balls”) separated by bands of pale fibrohistiocytic cells
Grenz zone
Tumor often spares band of superficial dermis
Folliculosebaceous induction and basilar epidermal hyperplasia overlying DF
Can mimic basal cell carcinoma if basilar induction is marked
Adjacent adnexal hyperplasia
Overlying melanocyte hyperplasia occasionally seen
So-called “dirty sock” sign
Predominant Pattern/Injury Type
Ill-defined borders
Nodular proliferation
Fibrous
Histiocytic
Predominant Cell/Compartment Type
“Fibrohistiocytic”
Histologic Subtypes
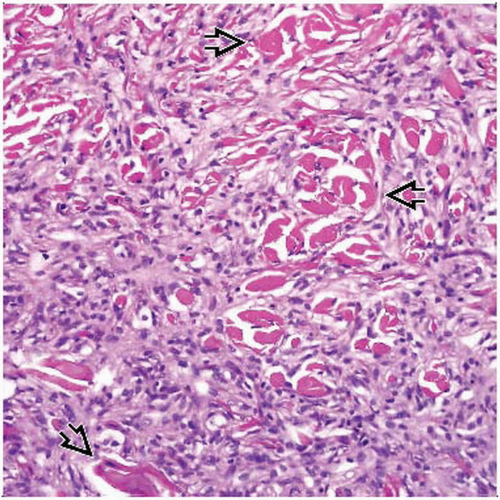
Aneurysmal (hemosiderotic/sclerosing hemangioma variant)
Pseudovascular spaces, hemosiderin, reactive spindle and epithelioid cells
May mimic vascular tumor, including Kaposi sarcoma and angiosarcoma
Aneurysmal DF can show some cytologic atypia but lacks high-grade atypia and shows only a few mitoses
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree