Cystitis Cystica and Glandularis
Jesse K. McKenney, MD
Key Facts
Terminology
Invaginated urothelial nests in superficial lamina propria with cystic dilatation forming luminal space
Cystitis glandularis has luminal cuboidal or columnar lining cells
Cystitis glandularis of intestinal type contains goblet cells
Etiology/Pathogenesis
May be normal variant or secondary to localized inflammatory response
Clinical Issues
Usually incidental finding
When florid, may have polypoid appearance clinically
No convincing evidence of neoplastic precursor lesion
Microscopic Pathology
Cystitis cystica has superficial nests of urothelium with central cysts
Glandular cells line central lumen in cystitis glandularis
Cystitis glandularis with intestinal metaplasia contains goblet cells
Rare cases have extensive mucin extravasation
Top Differential Diagnoses
Invasive adenocarcinoma
Noninvasive urothelial carcinoma with glandular differentiation (adenocarcinoma in situ)
Nested urothelial carcinoma with associated tubules
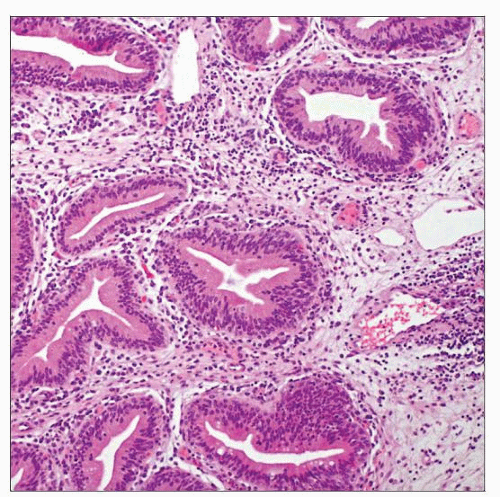
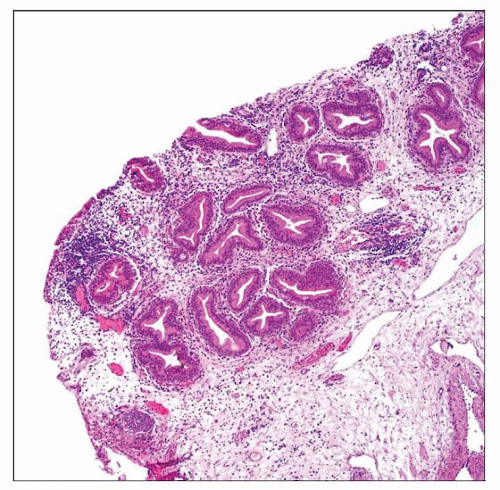 This collection of glandular structures within the superficial lamina propria has overall lobularity and a sharp linear border at the base, features typical of cystitis glandularis. |
TERMINOLOGY
Definitions
Cystitis cystica
Invaginated urothelial nests in superficial lamina propria with cystic dilatation forming luminal space
No cuboidal or columnar luminal cells are present
Cystitis glandularis
Cystitis cystica with luminal cuboidal or columnar lining cells
Cystitis glandularis with intestinal metaplasia (intestinal type)
Cystitis glandularis with at least focal intestinal-type goblet cells
ETIOLOGY/PATHOGENESIS
Environmental Exposure
May be secondary to localized inflammatory response
May be a variation in normal bladder microanatomy
CLINICAL ISSUES
Presentation
Usually incidental finding
When florid, small raised lesion with intact urothelium may be seen
Rare cases with intestinal metaplasia and extensive mucin extravasation may form large mass lesion that can mimic malignancy
Treatment
None
Prognosis
No convincing evidence that cystitis cystica or glandularis represents neoplastic precursor lesion
MACROSCOPIC FEATURES
General Features
May form polypoid mass in some florid examples
Intact overlying mucosa with variable translucent appearance
Usually < 1 cm
MICROSCOPIC PATHOLOGY
Histologic Features
Cystitis cystica
Superficial nests of invaginated urothelium in lamina propria
Connection to surface urothelium is variable
May be organized into lobules
In contrast to von Brunn nests, have cystically dilated lumen
No glandular-lining cells are present
Often admixed with von Brunn nests
Cystitis glandularis
Identical to cystitis cystica, except glandular cells line central lumen
Cuboidal or columnar cells with luminally oriented cytoplasm
Cystitis glandularis with intestinal metaplasia
Identical to cystitis glandularis with at least scattered intestinal-type goblet cells
Rare cases may have extensive mucin extravasation
No significant cytologic atypia
No irregular epithelial aggregates
No destructive invasion of muscularis propria
DIFFERENTIAL DIAGNOSIS
Invasive Adenocarcinoma
Noninvasive Urothelial Carcinoma with Glandular Differentiation (Adenocarcinoma In Situ)
Exophytic papillary urothelial carcinoma component may be present
Glandular component has more atypia than cystitis cystica
Columnar cells with nucleomegaly, hyperchromasia, and mitotic activity
May also have complex exophytic papillary glandular pattern
Nested Urothelial Carcinoma with Associated Tubules
Individual nests may have significant overlap with cystitis cystica on superficial biopsy
Have subtle nucleomegaly
Typically extends deeply into lamina propria or muscularis propria
Invasive clusters may have surrounding retraction
Prostatic-Type Polyp
Glands within stroma have prostatic secretory phenotype
Lightly eosinophilic, frothy cytoplasm
Round nuclei
PSA and PAP positive
Inverted Urothelial Papilloma
May have cystitis cystica-like pattern
Endophytic thin anastomosing cords are typical
More complex architecture compared to separate individual nests/glands of cystitis glandularis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree